Hysteroresectoscopy (HRS) is a modern gynecological procedure that allows surgical treatment of the uterus without compromising the integrity of its wall. During treatment, laser or electrosurgical methods are used to remove tissue under visual control (i.e., using video systems that allow the surgeon to see the organ cavity throughout the entire course of the operation).
- Indications
- Contraindications
- Advantages and disadvantages of GDS
- Preoperative preparation
- Technique for performing GDS
- Postoperative recommendations
- Complications after hysteroresectoscopy
Indications
Hysteroresectoscopy is performed to treat pathological formations, altered tissues or developmental abnormalities of the uterine cavity. Indications for the procedure include:
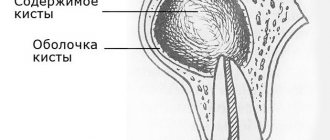
- Submucosal (located under the mucous membrane) fibroids.
- Polyposis or some types of single polyps.
- Asherman's syndrome - intrauterine synechiae (adhesions).
- Endometrial hyperplasia in case of ineffectiveness of drug therapy or in the presence of contraindications to it.
- Menometrorrhagia (abnormally prolonged/heavy bleeding from the genital tract during menstruation). Surgical treatment is indicated in the absence of the effect of hormone therapy.
- A septum in the uterine cavity.
Since hysteroresectoscopy is an organ-saving operation, it is especially relevant in the treatment of patients of reproductive age.
Pain after hysteroscopy
Most patients do not feel pain after hysteroscopy. They can be minor and localized in the perineum or pelvic area. Women have different pain sensitivity thresholds. If the pain is difficult to bear, the doctor prescribes non-narcotic analgesics in therapeutic doses. In cases where the pain is intense, you need to think about complicating the procedure. To exclude perforation of the uterine wall, either an ultrasound examination or repeat hysteroscopy should be performed.
If the pain after hysteroscopy does not go away after two days, the patient should contact the specialist who performed the study. The pain may be due to inflammation of the genitals. With inflammation, not only pain occurs after hysteroscopy, but also body temperature rises, purulent discharge from the genital tract with a foul odor appears. If such symptoms are present, the patient is hospitalized in a gynecological hospital and undergoes intensive therapy, including intravenous infusions of detoxification solutions, the administration of antibiotics in different ways, and immunomodulators and antihistamines are prescribed.
If you need to have a hysteroscopy performed, contact the IVF Center clinic in Yekaterinburg. In our clinic, this procedure is performed by experienced specialists with extensive experience. We regard pain after hysteroscopy that persists for more than two days as a complication of the procedure, and we re-examine the patient, find out the cause of the pain and prescribe treatment according to accepted standards.
Contraindications
Hysteroresectoscopy is an invasive procedure, so it has a list of certain contraindications. This list includes:
- Acute or chronic inflammatory diseases of the genital organs (colpitis, endometritis, cervicitis and others).
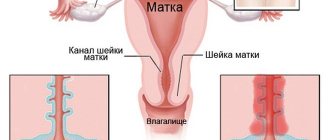
- Narrowing of the cervical canal (for example, due to scar changes).
- Oncological diseases of the reproductive system in the last stages, metastases in the pelvic organs.
- Profuse uterine bleeding.
- Pregnancy.
- Infectious diseases.
With caution, hysteroresectoscopy is prescribed for heart defects, kidney pathology, blood clotting disorders, etc. Sometimes before the procedure, a woman is prescribed special training that can reduce risks.
Book a consultation 24 hours a day
+7+7+78
Advantages and disadvantages of GDS
Hysteroresectoscopy has a number of advantages over other endoscopic and open surgical interventions. This is due, in part, to the use of high-tech equipment that is used to perform it. Thus, video monitoring with high resolution quality, which accompanies the entire operation process, allows the surgeon to clearly see the size, shape and localization of pathological changes. Electrosurgical or laser instruments used during the procedure cause less tissue trauma compared to a conventional scalpel. The positive aspects also include the short duration of hysteroresectoscopy. Usually the operation lasts no more than an hour.
The disadvantages of the procedure include its limited capabilities. Some diseases cannot be eliminated using this method, so the surgeon will be forced to use alternative techniques. In addition, since hysteroresectoscopy is performed using high-tech equipment, it requires an experienced surgeon who is familiar with the operation of laser or electrosurgical instruments and endoscopic techniques to successfully perform it.
Preoperative preparation
Before performing hysteroresectoscopy, as with other surgical interventions, the patient must undergo a certain examination, which includes:
- General blood test, urine test, biochemical blood test, determination of the Rh factor, vaginal smears, Wasserman reaction, etc.
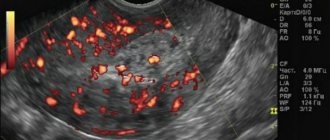
- ECG, chest x-ray, ultrasound of the pelvic organs.
- According to indications, consultations with other specialists are carried out.
The most favorable time for hysteroresectoscopy is the early phase of the menstrual cycle, so it is necessary to plan the operation for this period. In some cases, for the purpose of preparation, a woman is prescribed special hormonal drugs, for example, gonadotropin-releasing hormone agonists (GnRH agonists).
Immediately before the procedure, preparation of the gastrointestinal tract is necessary: the patient is prescribed a cleansing enema. Before surgery, food and water intake is prohibited.
Hysteroresectoscopy at the ABIA clinic, St. Petersburg:
Our clinic performs all examinations necessary for an accurate diagnosis: video colposcopy, ultrasound and ultrasonic hysterosalpingoscopy, laboratory tests. When solving various gynecological problems, the clinic’s gynecologists use modern diagnostic and treatment equipment and equipment from leading manufacturers of medical equipment.
When polyps and myomatous nodes are identified, our gynecologists will select the optimal and effective therapy, which may include hormonal therapy or surgical treatment. If necessary and if indicated, sick leaves are issued for the period of treatment.
Technique for performing GDS
The method of pain relief during hysteroresectoscopy may vary. If a short-term intervention is expected, then intravenous anesthesia is used. Its action lasts for 30-40 minutes. If the operation promises to be long, then endotracheal (mask) or epidural anesthesia is used.

Immediately before surgery, the genitals and inner thighs are treated with antiseptic agents. In this case, the patient is in a gynecological chair. The surgeon dilates the cervix using special instruments, and then inserts the hysteroresectoscope into the uterine cavity. Next, a special liquid is injected that does not conduct current (usually a solution of glucose with sorbitol is used). Due to fluid pressure, the uterine cavity expands, which creates a good overview and the necessary space for various manipulations. Using a hysteroresectoscope, which displays an image on the screen, the surgeon carefully examines the uterine cavity, paying attention to its size, the relief and thickness of the mucous membrane, and the condition of the orifices of the fallopian tubes. The location, size and shape of altered tissues or pathological formations are carefully studied. After the necessary examination, they are excised using laser or electrosurgical instruments. The surgeon tries to remove the pathological focus as much as possible; often part of the normal tissue is captured, which helps avoid relapse of the disease.
Operative hysteroresectoscopy and office hysteroscopy
A woman choosing a clinic for hysteroscopy should especially pay attention to this:
The so-called office hysteroscope does not allow operations; it is intended only for diagnostics. You should not fall for advertising claims that office hysteroscopy is performed with a thinner, more flexible instrument. Why split the diagnostic and treatment procedure into two operations when all identified problems can be solved at once?
The BIRCH clinic uses an operating hysteroresectoscope. Therefore, we can not only diagnose, but also eliminate any uterine pathology detected during the procedure.
The next Video on our YouTube channel is dedicated to this topic.
When is it necessary to use surgical hysteroscopy? - explanations of the chief physician of Birch - Sakhno Alexey Viktorovich:
Postoperative recommendations
The rehabilitation period after hysteroresectoscopy always proceeds individually, depending on the goals and scope of the operation performed. However, there are several general points that are almost always noted:
- After surgery, the patient may feel moderate pain and discomfort in the lower abdomen. In order to eliminate these unpleasant sensations, the doctor will prescribe painkillers.
- Hysteroresectoscopy almost always causes damage to the endometrium. Sometimes it recovers on its own, but in some cases, to improve its regeneration, it is necessary to take estrogen medications. The average duration of the course is about three months, but according to the doctor’s recommendation it can be longer or shorter.
- In some cases, a woman is indicated for other specific treatment. The doctor will select the dosage of the drugs, the regimen and the duration of the course individually.
In general, rehabilitation after hysteroresectoscopy is calm and quick, especially if the operation was performed by an experienced doctor using modern equipment.
Complications after hysteroresectoscopy
Adverse consequences after surgery can occur for various reasons. All of them can be divided into three groups:
- Intraoperative (arising during surgery). These include bleeding and perforation (through damage) of the uterine wall.
- Electrosurgical. Burn tissue damage occurs when the technique of working with electrosurgical instruments is not followed.
- Postoperative. After hysteroresectoscopy, inflammatory lesions of the uterine walls, accumulation of blood in the uterine cavity, narrowing of the cervical canal, acute infectious processes, etc. may develop.
To avoid the development of complications after hysteroresectoscopy, careful preoperative preparation, a complete examination before surgery and individualization of tactics in each clinical case are necessary. The surgeon must have extensive experience in performing such interventions and have at his disposal all the necessary equipment and consumables.
Hysteroresectoscopy allows women to get rid of the disease, eliminate pain and restore the function of the reproductive system. For example, after removal of a uterine polyp, the menstrual cycle normalizes in 60-80% of patients, and in 30% of cases it is possible to restore a woman’s reproductive health. When treating uterine fibroids using hysteroresectoscopy, it is possible to restore reproductive function in 76% of those operated on. Therefore, this operation continues to remain relevant and is actively performed in the best medical institutions around the world.
Book a consultation 24 hours a day
+7+7+78
Doctors
Lukyanova Olga Yurievna Obstetrician-gynecologist, gynecologist-endocrinologist
Doctor of the first qualification category
Make an appointment
Shakhmartova Irina Aleksandrovna Head of the Women's Health Department, obstetrician-gynecologist
Doctor of the highest qualification category
Make an appointment
Ivanova Irina Igorevna Obstetrician-gynecologist MEDSI Premuim
Make an appointment
Minchenkova Anna Vyacheslavovna Obstetrician-gynecologist MEDSI Premuim
Doctor of the highest qualification category, Candidate of Medical Sciences
Make an appointment
Livshits Yulia Igorevna Doctor – gynecologist-sexologist, ultrasound diagnostics doctor
Doctor of the highest qualification category
Make an appointment
Solovyeva Marina Evgenievna Obstetrician-gynecologist
Doctor of the highest qualification category, Candidate of Medical Sciences
Make an appointment
Kvasnetskaya Natalya Vasilievna Obstetrician-gynecologist
Candidate of Medical Sciences, doctor of the highest qualification category
Make an appointment
Sengirbekova Saida Isaevna Obstetrician-gynecologist, gynecologist-endocrinologist
Doctor of the first qualification category
Make an appointment
All doctors (21)