- Causes of fibroids
- When is surgery required for fibroids?
- Methods of surgical treatment
- Preparing for surgery
- Research and diagnostics
- How do you know which type of surgery is right for a particular woman?
- Recovery, postoperative period
- Consequences of hysterectomy
- Alternative Treatments
- Focused ultrasound ablation (FUS-MRI)
- Uterine artery embolization (UAE)
“You have myomatous nodes in your uterus,” 70–80% of women will sooner or later hear these words from a gynecologist. Myoma is one of the most common diseases of the female reproductive system. Because of it, hundreds of thousands of women in Russia every year end up on the operating table and lose their uterus.
Previously, doctors believed that uterine fibroids were a benign tumor that developed from smooth muscle cells. They fought it radically: often the gynecologist immediately referred the patient for a hysterectomy - an operation to remove the uterus.
Today the approaches have changed. The causes of fibroids and methods of their treatment have been significantly revised. But not all women (and, let’s be honest, not all gynecologists) know about this.
Causes of fibroids
Overly aggressive treatment of uterine fibroids in the past was largely due to a lack of understanding of their nature. Open an old medical school gynecology textbook and you will read that fibroids are a benign tumor that occurs due to a hormone imbalance. The question immediately creeps in: what if this benign tumor turns into a malignant one? Isn't it better to remove it right away - along with the uterus, just to be sure?
To date, it has been proven that uterine fibroids are not related to cancer and do not increase the risk of cancer. This is a node that grew from an improperly developing muscle cell. It does not arise due to hormones, but grows under their influence.
Modern scientists do not know exactly why fibroids develop. Some believe that this is the result of a violation of intrauterine development. The muscle layer in the wall of the uterus in the fetus develops slowly and remains in an unstable state for a long time, so disturbances occur in it. According to another theory, the disease is caused by damaging factors that affect a woman throughout her life: abortion, curettage, multiple periods, infections and inflammatory processes.
Whatever the cause, fibroids are not life-threatening or cancerous, so aggressive treatment is often not necessary.
When is surgery required for fibroids?
Let's talk about when fibroids actually require treatment. There are only three indications:
- Myoma is growing according to the latest 3–4 ultrasound examinations performed at intervals of 4–6 months.
- Myoma causes symptoms: prolonged, heavy, painful menstrual bleeding, disturbances in bowel movements, urination, and abdominal enlargement.
- Myoma leads to problems in the reproductive sphere: infertility, miscarriage.
But even if a woman has one of these points, it is often not necessary to undergo surgery. There are minimally invasive treatment options.
Diagnostics
Often, fibroids are discovered accidentally during a medical examination or after heavy bleeding. The diagnosis is made based on diagnostic data:
| Type of diagnosis | results |
| History taking | The patient should be prepared for the doctor to ask not only general questions, but also questions related to the intimate sphere. The truthfulness of the answers affects the final result when making a diagnosis. |
| Gynecological examination | During a bimanual examination, the doctor determines the size and shape of the uterus, the intensity of pain, and the presence of bleeding. |
| Ultrasound sonography transvaginal or transabdominal | The main method of examination for fibroids. On an ultrasound image, the tumor is visualized as dense, round-shaped foci; the location, number, and size of the foci are determined. |
| Smear for microflora and STDs | Identification of pathogenic pathogens with possible inflammation. |
| Oncocytological smear | Detection of dysplastic processes in the uterus and appendages. |
| Hormonal panel | The level of estrogen and pituitary hormones is determined. |
| Blood and urine tests | Exclusion of the inflammatory process in the genitourinary system, determination of complications of bleeding (anemia). |
| MRI | To clarify the diagnosis. |
| Biopsy | For differential diagnosis and exclusion of a malignant process. |
For each patient, a set of studies is selected individually; all of the above methods are not necessarily used.
Methods of surgical treatment
The “old school” approach of removing the uterus from all women with fibroids has now been abandoned. Hysterectomy is a last resort; it is used only in the most severe cases, when other interventions are impossible. The uterus performs important functions in a woman’s body; we should always try to preserve it.
A more gentle operation is myomectomy, when only the fibroid is removed. This intervention can be performed in different ways.
Laparotomy surgery (open method, through an incision)
The intervention is performed through a horizontal incision in the lower abdomen, along the bikini line, or through a vertical incision along the midline. The operation is performed under anesthesia.
This option for removing uterine fibroids is the simplest and does not require special equipment, but after it a large scar remains on the wall of the organ and adhesions are formed, which can lead to infertility. If a woman wants to have a baby in the future, she will most likely have to have a caesarean section.
In some cases, laparotomy myomectomy can be performed through a small 5 cm incision. Moreover, after removal of the node, tissue healing occurs faster and the recovery period is reduced.
Laparoscopic surgery (through punctures)
Removal of uterine fibroids laparoscopically is performed without incisions. Four or five punctures are made in the wall of the abdominal cavity: one near the navel, the rest in the lower abdomen. A laparoscope (an instrument with a video camera) and special surgical instruments are inserted through them. In order to improve visualization and create free space for work, carbon dioxide is injected into the abdominal cavity. During the operation, the woman is under anesthesia.
After laparoscopic operations, there are no large scars left, and the risk of adhesions is lower. But not all fibroids can be removed in this way. Currently, robot-assisted laparoscopic removal of uterine fibroids is performed using Da Vinci units. All manipulations are performed by the robot’s “hands,” and the surgeon controls them using a remote control, watching the process on the screen.
Hysteroscopic surgery
This type of node removal is performed without making any cuts in the skin. A special instrument, a hysteroscopic resectoscope, is inserted into the uterine cavity through the vagina. Its working part is a wire loop to which electric current is supplied. It cuts and cauterizes the tissue, which stops the bleeding. The procedure is performed under general anesthesia. Often, during hysteroscopic removal of nodes, laparoscopy is performed simultaneously: it is needed for control, so as not to open the uterine cavity.
After hysteroscopic removal of uterine fibroids, there are no incisions on the skin, and recovery occurs quickly. But complications are possible: perforation (puncture) of the uterine wall, scarring in its cavity, bleeding. During the intervention, the uterus is filled with fluid, and if this fluid is absorbed in large quantities into the blood vessels, “water intoxication” (TUR syndrome) develops.
Surgical treatment of uterine fibroids.
Surgery is the only way to completely eliminate a benign tumor. Operations can be radical, when the uterus is completely removed, or organ-preserving - removal of myomatous nodes (myomectomy).
Indications for surgical treatment:
- pain syndrome;
- heavy menstruation, bleeding, including those leading to a decrease in hemoglobin numbers (anemia);
- large fibroids (12 weeks or more);
- rapid tumor growth (more than 4 cm per year);
- the occurrence and/or growth of a tumor in postmenopause;
- inflammation and/or necrosis of the node;
- infertility or miscarriage associated with the presence of uterine fibroids;
- disturbance of urination and bowel movements due to compression by the tumor.
Types of surgical interventions for uterine fibroids:
If surgical intervention is necessary in pre- and postmenopause, as well as in combination with other pathology of the uterus, the uterus is completely removed - hysterectomy (hyserectomy) or removal of the uterine body without the cervix, supravaginal amputation of the uterus (subtotal hysterectomy).
During reproductive age, as well as when planning pregnancy, tumor nodes are removed while preserving the uterus - myomectomy.
Hysterectomy or supravaginal amputation of the uterus, like myomectomy, can be performed laparoscopically or by laparotomy.
Enucleation of submucosal nodes is possible by performing hysteroresectoscopy. The essence of the procedure is to expand the cervical canal, introduce a sterile solution into the uterine cavity and remove the tumor with an electrosurgical instrument under the control of an optical system connected to a video camera. This intervention is indicated in the presence of nodes that are almost completely located in the uterine cavity. The advantages of the method are minimal invasiveness, absence of incisions and scars, rapid recovery, and the possibility of reproductive function.
Preparing for surgery
Before removing uterine fibroids, it is important to carefully assess the woman’s health, identify concomitant diseases and, if necessary, undergo treatment from specialized specialists. Preoperative examination before removal of myomatous nodes includes:
- general blood and urine analysis;
- biochemical blood test (determining the levels of protein, sodium, chlorides, potassium, pH, creatinine, urea);
- electrocardiography;
- blood pressure measurement;
- fluorography.
Before surgery, an anesthesiologist talks with the patient, finds out what chronic diseases she has, whether there are any allergic reactions to medications, and assesses possible risks.
Surgical treatment of fibroids is usually performed on days 5–14 of the menstrual cycle.
Symptoms, diagnosis, treatment of uterine fibroids: video.
Head of the Department of Oncogynecology at Clinical Hospital No. 4, Candidate of Medical Sciences, obstetrician-gynecologist, oncologist, surgeon Anton Anatolyevich Ishchenko and obstetrician-gynecologist, employee of the Department of Oncogynecology at Clinical Hospital No. 4 Victoria Viktorovna Ivanova appeared in the TV show “Doctor Knows”, dedicated to the problem of uterine fibroids on the Otkryty TV channel world. Health. The TV program covers methods for diagnosing uterine fibroids, possible complications and modern treatment methods. The advantages and disadvantages of various types of surgical interventions and conservative therapy, as well as the choice of technique depending on the form of the disease and the age of the patient, are discussed.
At the University Clinical Hospital No. 4 of the First Moscow State Medical University named after. THEM. Sechenov experienced specialists perform all types of surgical interventions for uterine fibroids. Hospitalization and surgical treatment are carried out within the framework of compulsory medical insurance, voluntary medical insurance, under the program of high-tech medical care and for a fee.
How do you know which type of surgery is right for a particular woman?
Open surgery through an incision is used to remove subserous fibroids (located on the surface of the uterus under the outer lining) and intramural (in the thickness of the muscular layer of the uterine wall). This type of removal is optimal for large, multiple nodes, if there is a suspicion of a malignant tumor.
Laparoscopic myomectomy is the optimal type of surgical removal of small nodes located subserosally on the outer surface of the uterus. Since laparoscopy does not leave large scars, it is preferable for women who are planning a pregnancy in the future. But punctures cannot remove large, multiple fibroids.
Hysteroscopic surgery is possible when the myomatous node is located inside the uterus under the mucous membrane and protrudes into the organ cavity by at least half. The size of the node is no more than 5 cm - an important condition for the possibility of its removal.
Symptoms of pathology:
- menorrhagia - heavy menstruation, often occurring in the form of bleeding, leading to a decrease in hemoglobin;
- pain in the lower abdomen of varying severity - from minor to extremely intense (with necrosis of the node and the development of peritonitis);
- reproductive dysfunction (infertility or miscarriage);
- constipation – when the rectum is compressed by a fibroid node;
- urinary disorders in the form of frequent urge or acute urinary retention;
- an increase in the size of the abdomen - in the presence of large nodes of uterine fibroids.
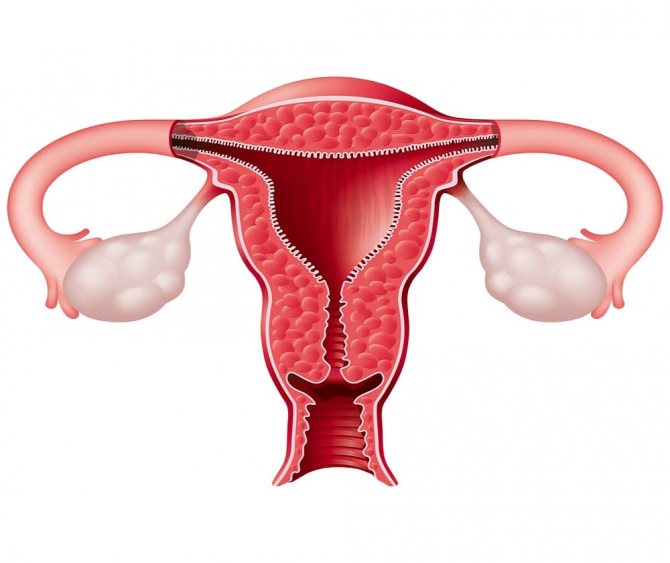
Depending on their location, myomatous nodes are divided into:
Subserous (subperitoneal) - located mainly on the outer surface of the uterus, on a thin stalk or wide base through which feeding vessels approach. Therefore, when the subperitoneal nodes are large, the blood flow is insufficient and ischemia or tumor necrosis and peritonitis occur. Since subserous fibroids are located predominantly in the abdominal cavity, compression of neighboring organs (bladder, ureters or rectum) may occur and, as a result, disruption of their function.
Submucosal (submucosal) - located mainly in the uterine cavity, prevent normal contraction of the uterus and emptying of the uterus during menstruation and lead to an increase in its duration, profuseness, and the occurrence of pain. In addition, submucosal nodes can prevent implantation of the fertilized egg and the development of pregnancy.
In rare cases, submucosal nodes may be “born,” which is accompanied by severe pain and bleeding.
Interstitial (intramural, intermuscular) - nodes are located in the myometrium and often tend to be subperitoneal (centrifugal growth) or deform the uterine cavity (centripetal growth). When small in size, it is often asymptomatic.
Uterine fibroids with an atypical location of nodes – interligamentous, cervical, “parasitic”, etc. – manifests itself, as a rule, with symptoms of compression of neighboring organs or pain.
Some women do not even realize that they have a problem, since the neoplasm may not manifest itself for a long period of time. Often a tumor is detected during a routine examination.
Even in the absence of symptoms, the disease requires observation at least once every 6 months. When the uterus enlarges due to neoplasms up to 8-9 weeks of pregnancy or one of the nodes is more than 2-3 cm, most often symptoms appear that require treatment. It should be noted that submucosal uterine fibroids of any size can be accompanied by pronounced clinical manifestations in the form of heavy menstruation and uterine bleeding.
Recovery, postoperative period
The duration of the recovery period depends on the type of surgery:
- After removal of the uterus, complete recovery occurs within 4–6 weeks. During this time, physical work and sexual intercourse should be avoided. You cannot drive a car for 1–2 weeks.
- After open removal of uterine fibroids, a woman spends 1–2 nights in the hospital, then she is discharged. Physical activity is contraindicated for 4–6 weeks.
- After laparoscopic removal of fibroids, a woman spends only one night in the hospital. Full recovery occurs after 4 weeks.
- Hysteroscopic surgery is often performed on an outpatient basis: you can return home within a few hours. The recovery period lasts from 48 hours to several days.
Usually, you are allowed to get up and walk after open removal of uterine fibroids the next day. After laparoscopic interventions - after a few hours.
To monitor the condition of the uterus after removal of fibroids, women are prescribed regular ultrasound examinations. Pregnancy can be planned after 12 months; before that, doctors recommend protection with oral contraceptives. To reduce the risk of relapse, hormonal drugs can be prescribed, but it must be remembered that they can cause some side effects, including impairing blood supply to the uterus and healing after removal of the node.
The main methods for diagnosing uterine fibroids include:
- gynecological examination, which makes it possible to detect an increase in the size of the uterus, a change in its shape and the presence of subperitoneal nodes.
- Ultrasound examination of the pelvic organs - allows not only to accurately establish the diagnosis of fibroids, carry out differential diagnosis with other gynecological diseases, but also to monitor the growth of nodes. If there are uterine fibroids, an ultrasound of the pelvic organs should be performed at least once every 6 months.
- MRI of the pelvic organs with intravenous contrast - allows you to clarify the location of the nodes, as well as identify possible compression of neighboring organs.
- computed tomography of the pelvic organs with intravenous contrast makes it possible to assess the condition of the pelvic vessels, including in preparation for embolization of the uterine arteries, as well as to identify compression of the ureters and changes in their location.
- hysteroscopy examination of the uterine cavity with an optical system connected to a video camera, which is inserted through the cervix and is often accompanied by separate therapeutic and diagnostic curettage to remove intrauterine pathology. During this intervention, the location of the submucosal nodes and their type, and the possibility of removal by hysteroresectoscopy, are clarified.
Consequences of hysterectomy
A woman needs a uterus not only to give birth to children. It affects the functioning of other organs and metabolism. After its removal, women who have not yet entered menopause often develop a serious complication - posthysterectomy syndrome. Its manifestations are diverse:
- increased risk of endocrine and metabolic disorders;
- increased sweating, chills, hot flashes, poor tolerance of high temperatures;
- sleep disturbance;
- increased heart rate;
- numbness in different parts of the body, a feeling of “pins and needles”;
- fatigue, lethargy, decreased performance;
- depression, anxiety, fear of death;
- high blood pressure;
- excess fat deposits in the abdomen and waist;
- increased risk of osteoporosis;
- urinary incontinence, dryness, itching in the vagina, problems with sex life.
In women who have had a hysterectomy, the risk of coronary heart disease doubles, blood pressure begins to rise earlier, and if arterial hypertension already existed, its course worsens.
After a hysterectomy, a woman receives a set of health problems, due to which she cannot live a full active life; to combat them, she has to constantly take medications.
Features of the methodology and progress:
During laparoscopy, instruments and an optical system are inserted through incisions on the anterior abdominal wall up to 1 cm long. During myomectomy, the nodes are removed from their bed, which is then coagulated, after which sutures are applied. The removed tumors are removed in parts using a morcellator through one of three previously made incisions.
Extirpation and supravaginal amputation of the uterus are also performed through 3 incisions. At the same time, the ligaments and vessels approaching the uterus are cut off and coagulated. In case of complete removal of the uterus, it is removed through an opening in the vagina.
At the end of the operation, the incisions are sutured.
With laparotomy (transsection), the surgical technique is not much different. A special feature is careful suturing, since there is no coagulation. At the same time, a more complete, durable scar is formed on the uterus.
Alternative Treatments
So, myomectomy helps to radically solve the problem with myomatous nodes and preserve the uterus. However, surgical treatment has a number of disadvantages:
- High risk of relapse: after 4–5 years, nodes are found again in approximately half of the operated women.
- Scar and adhesions after removal of nodes can cause infertility and lead to complications during pregnancy.
- Any operation and anesthesia is associated with certain risks.
When offering a woman surgical treatment, the doctor must be sure that during the operation there is no risk of opening the uterine cavity, and the organ will not have to be completely removed. Because of the high risk of recurrence, myomectomy is suitable for women who are planning a pregnancy soon, rather than in a few years.
Currently, the indications for surgical removal of fibroids are decreasing because there are other, minimally invasive techniques.
If left untreated, complications may develop:

- chronic anemia - occurs as a result of constant blood loss during menstruation and is manifested by weakness, fatigue, dizziness, pale skin and mucous membranes, hair loss, brittle nails, performance is significantly reduced. In some cases, a blood transfusion is even necessary (for severe anemia).
- node necrosis – most often occurs when the tumor is subperitoneal or atypically located and requires emergency surgical treatment due to the development of peritonitis. In this case, the uterus is removed along with the tumor to avoid septic complications.
- Tumor malignancy is an extremely rare occurrence. As a rule, a malignant tumor in the myometrium occurs primarily, and not as a result of degeneration of fibroids. Uterine sarcoma initially has clinical manifestations similar to fibroids. A distinctive feature is the rapid growth of the tumor (more than 4 weeks in 1 year) or the appearance and/or growth of a node in postmenopause.
- rupture of a uterine fibroid vessel is accompanied by intra-abdominal bleeding and can be life-threatening. This complication requires emergency surgical treatment.
Focused ultrasound ablation (FUS-MRI)
Myomatous nodes are destroyed by heating with intense ultrasound waves under MRI control. Compared to surgery, the procedure is non-invasive, there is no incision, no blood loss, and no long recovery period is required. But there are also disadvantages. Using FUS-MRI, no more than 1–3 small nodes can be removed. Some complications are possible: burns to the skin of the abdomen, damage to healthy tissue around the node, pain due to damage to nearby nerves, risk of deep vein thrombosis of the legs.
Currently, not many studies have been conducted that would prove the effectiveness and safety of the method in the long term, or the possibility of pregnancy after its use.
Why is it better to have myomectomy done at the Swiss University Hospital?
- Surgeons at our clinic were the first in the country to perform SILS surgery and laparoscopic myomectomy. The clinic also performs operations using transvaginal access (NOTES surgery).
- The specialists of our Center have impressive experience in performing myomectomies; our surgeons have performed several thousand successfully performed operations; more than 1,500 unique surgical interventions are performed annually. Moreover, our leading specialists act as experts in many professional organizations.
- The clinic’s surgeons strive to use organ-preserving and minimally invasive techniques that are as gentle as possible during surgical treatment of reproductive organs. Thanks to this approach, our patients can have children in the future.
- If necessary, we perform simultaneous operations; during one intervention, you can get rid of not only fibroids, but also concomitant diseases of the ovaries and fallopian tubes.
- Simultaneously with myomectomy, we can perform reconstructive surgeries on the vagina and rectum for widespread endometriosis.
- We successfully use our own patented laparoscopy technique with temporary occlusion of the uterine arteries, so we are able to remove complex, large myomatous nodes without blood loss.
- Due to excellent visualization of the operation site and the absence of bleeding during the intervention, we are able to reliably suture the myometrium, which affects the formation of a healthy scar. We also use anti-adhesion barriers to prevent the occurrence of adhesions, which is especially important if a woman plans to give birth in the future.
Uterine artery embolization (UAE)
Uterine artery embolization has been performed for several decades, but it has recently begun to be discussed as a promising method for treating uterine fibroids. During this procedure, under X-ray control, the doctor injects an embolic drug into the vessel feeding the node through a catheter. It consists of particles that block the lumen of small blood vessels. The myomatous node is deprived of oxygen and nutrients, dies and is replaced by connective tissue. In fact, a small scar remains in its place. And if the node is inside the uterine cavity, it can separate and exit through the vagina.
At the moment, many studies have been conducted that have shown that UAE is an effective and safe method of treating fibroids, and has advantages over surgical removal of fibroids:
- This is a minimally invasive procedure. It is performed without an incision or anesthesia; the catheter is inserted through a puncture in the upper thigh.
- Short postoperative recovery period, the woman can quickly return to her normal life.
- After embolization of the uterine arteries, it is still possible to become pregnant and give birth to a child.
- The risk of relapse is less than 1%. If uterine fibroids are detected again, UAE can be repeated. This type of treatment is well suited for women who are planning a pregnancy in the long term.
- High efficiency: in 98% of cases after UAE, a woman does not require any additional treatment methods.
It is important to understand that uterine artery embolization and myomectomy are not competing treatments. Everyone has their own testimony. If you want to find out what is suitable for your case and get advice from a competent doctor, contact the European Clinic. We have a doctor who defended the first dissertation in Russia on the treatment of uterine fibroids using UAE, and has many years of experience in using this technique - Dmitry Mikhailovich Lubnin.
+7 (24/7) Expert consultation
Carrying out surgery
Laparoscopy is performed under general anesthesia and lasts from 40 minutes. up to 2 hours. A trocar is inserted into the abdomen, pumping carbon dioxide, lifting the peritoneal wall and improving visibility of the operated area. Then a second trocar is installed, equipped with an LED and a camera. Afterwards, the surgeon inserts 2 more trocar tubes (4 in total). Through them, using an endoscopic instrument, adhesions are dissected, the tissue above the node is cut, the formation is removed, the vessels are sealed, and sutures are applied. The order of manipulations may vary at the discretion of the surgeon. If the fibroids are large and it is impossible to remove them through the tube, a morcellator is used - a grinding device that is inserted instead of a trocar. Thus, the entire operation is performed through 4 punctures without additional incisions. At the end of the intervention, the holes are sutured, disinfected, and isolated with napkins soaked in a sterilizing composition. No drainage needed.
The optimal time for the operation is the period between the 15th and 25th day of the cycle.