Stoparthrosis
» Treatment methods
» Ultrasound of soft tissues of the abdominal wall
Litvinenko A. S.
July 2, 2021 3497
Ultrasound examination of the condition of the soft tissues of the anterior abdominal wall allows not only to identify pathologies and correctly diagnose, but also in some cases save a person’s life.
Diagnostics is simply irreplaceable for acute pain in the abdominal area, detection of a foreign object, injuries to both the peritoneal wall itself and internal organs. Ultrasound of the soft tissues of the abdominal cavity helps to diagnose a huge number of different pathologies and provide timely medical care, including surgery.
Treatment with us is profitable!
- 20 years of experience
in treating diseases of the joints and spine - All in 1 day
— diagnostics, consultation and we will begin treatment
- Doctor's appointment 0 RUB! until August 15th!
when treated with us - PROMOTION
Sign up for an examination
Cost
2000 rub.
Duration
15-20 minutes
Experience of specialists
10-17 years
- 15 years of experience
in treating diseases of the joints and spine - Everything in 1 day
- doctor’s examination, diagnosis and treatment - Doctor's appointment 0 RUB!
during treatment with us
Sign up for an examination
Old price:
duration
— a course of treatment
What will an ultrasound of the soft tissues of the abdominal wall show?
Doctors prescribe an examination using ultrasound when pain appears in the peritoneum, as well as for self-diagnosis of various seals (hernias) and neoplasms. In addition, experts recommend undergoing an ultrasound of the soft tissues of the anterior abdominal wall in case of problems with the intestines and urination, the appearance of bitterness in the mouth, as well as weakness and general poor health.
Diagnostics allows the doctor to study in real time the condition of the peritoneal wall and internal organs (liver, pancreas, spleen, abdominal aorta, gall bladder, etc.). The study helps to identify a defect in the anterior wall and differentiate the contents of the hernial sac, as well as diagnose bruises, injuries, and possible bleeding from internal organs.
Sign up for an ultrasound of the soft tissues of the abdominal wall
Ultrasound of the lower leg: what does the diagnosis show?
Ultrasound examination of the ankle joint is performed in a sitting or lying position in accordance with standard techniques. The joint tissues are scanned in the 4 main projections for this study (anterior, medial, lateral and posterior). A thorough examination of the ankle allows us to identify pathologies such as:
- partial or complete rupture of ligaments or tendons;
- arthrosis;
- arthritis, tendinitis;
- Morton's neuroma;
- heel spur;
- hygroma.
Of course, what an ultrasound of the ankle joint will show depends on the professionalism of the diagnostician, as well as the quality of the equipment. Modern ultrasound machines used for examination at the Stoparthrosis clinic are highly sensitive. They are able to identify the pathological process at an early stage of its development. The clinic’s doctors have extensive experience and understand all the intricacies and nuances of ankle examination. By contacting the Stoparthrosis clinic, you can not only undergo the examination quickly and inexpensively, but also get answers to your questions. Qualified doctors of the clinic, taking into account diagnostic data, tests and the patient’s symptoms, will prescribe effective treatment and monitor its effectiveness.
Author of the article:
Kholikov Timur Vyacheslavovich
Orthopedist
Make an appointment
Recent publications by the author:
- Ultrasound of the thoracic region
- What will an ultrasound of the joints show?
- Radiography
- Ultrasound of joints
Ultrasound of soft tissues of the abdominal cavity: preparation for diagnosis
When conducting a planned examination of the anterior wall of the peritoneum before the procedure, it is necessary to refrain from taking foods that promote gas formation: legumes, soda, baked goods, etc.
In addition, to improve digestion and intestinal function, doctors recommend taking enzymes. Before the procedure, a cleansing enema and fasting are indicated. If X-ray examinations using a contrast agent were carried out several days before the ultrasound examination, ultrasound of soft tissues is not performed.
Author of the article:
Litvinenko Andrey Sergeevich
Orthopedist
Make an appointment
Recent publications by the author:
- Ultrasound diagnostics
- Ultrasound of the nerve
- Radiography
- Cervical osteochondrosis: ultrasound
Indications for ultrasound
Indications for ultrasound examination of the legs are most often prescribed by a phlebologist. The main indications for ultrasound diagnostics are usually:
- Swelling in the area of the feet, legs and other elements of the legs;
- Systemic regular paresthesia - from tingling to numbness;
- Visually visible expansions of venous structures - spider veins, large telangiectasias, and so on;
- Changes in the shade of the epithelium on the lower extremities, cyanotic skin in different locations - from the foot to the calf;
- Very long healing of wounds, cuts and ulcers on the legs;
- A feeling of constant weakness in the legs, a change in their temperature towards a decrease in relation to a similar parameter in other parts of the body;
- Regular pain and cramps in the legs, occurring both during the day and at night;
- Other pathological changes - from the disappearance of hair growth on the legs and unbearable skin itching to a decrease in the volume of the lower leg and lameness.
Our doctors
- LITVINENKO Andrey Sergeevich
Traumatologist orthopedist Sports medicine doctor Experience: 19 yearsSign up
- SKRYPOVA Irina Viktorovna
Physiotherapist rehabilitator Experience: 19 yearsSign up
- MOISEENKO Alexey Yurievich
Traumatologist orthopedist Sports medicine doctor Experience: 17 yearsSign up
- KHOLIKOV Timur Vyacheslavovich
Traumatologist orthopedist Sports medicine doctor Experience: 19 yearsSign up
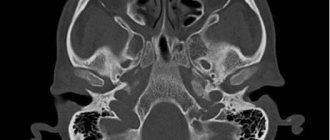
Ultrasound examination of the maxillofacial area
Ultrasound machine RS85
Revolutionary changes in expert diagnostics.
Impeccable image quality, lightning-fast operating speed, a new generation of visualization technologies and quantitative analysis of ultrasound scanning data.
The ultrasound research method has become firmly established in general diagnostic practice; its role can hardly be overestimated. A modern approach to diagnosing diseases in the clinic of internal medicine is unthinkable without ultrasound examination of the abdominal organs (including the retroperitoneum and pelvis), thyroid gland, mammary glands, heart and blood vessels.
Compared to the above-listed areas of application of echography, ultrasound examination of the maxillofacial area is performed much less frequently. This is due, on the one hand, to the clinical isolation of dentistry and maxillofacial surgery, which does not allow general practitioners of ultrasound diagnostics to gain sufficient experience in research in this area, and on the other hand, to some conservatism of dentists and maxillofacial surgeons, who consider the main diagnostic tool for them to be X-ray examination method. Their skepticism regarding ultrasound examination is based on the fact that almost all soft tissue structures of the maxillofacial region are accessible to palpation, and the skin and mucous membranes are accessible to inspection.
However, paying tribute to the history of the development of ultrasound diagnostics, it is necessary to mention that the object of the very first (then still one-dimensional - in A-mode) echographic studies performed by a group of researchers led by D. Howry in 1955 were the parotid glands.
Ultrasound of soft tissues of the face and neck in its modern version does not require the use of any special ultrasound scanners or sensors and can be performed on equipment designed for studying peripheral structures: linear sensors with an oscillation frequency of 5.0-7.5-9 are quite sufficient .0 MHz. Transcutaneous echography is quite informative and generally satisfies the needs of clinicians: almost all parts of the face and neck (including the body and root of the tongue) are accessible to echographic examination using external sensors. Only the upper parts of the peripharyngeal space and the pterygomaxillary space, shielded by the branch of the lower jaw, are inaccessible.
There are no age restrictions or special preparation of the patient for an ultrasound examination.
For an ultrasound diagnostic physician, the maxillofacial area can be of great professional interest, since diseases of all nosological groups are found here (from inflammatory, autoimmune and degenerative-dystrophic to tumor), as well as various malformations (angiodysplasia, lymphangiomas, congenital cysts). Differential diagnostic difficulties increase due to the fact that the maxillofacial area is a zone of massive infection and the existence of primary non-inflammatory diseases is often masked by the addition of an inflammatory process with the entire spectrum (from erased to clinically pronounced) of its signs.
The complexity of the anatomical structure of the maxillofacial region creates additional difficulties for interpreting the results of ultrasound examination. At the same time, anatomical detail is of great importance, since determining the organ affiliation of the pathological process and clarifying the topographic and anatomical features of its distribution are one of the most important diagnostic tasks, along with identifying the nosological form of the disease. This point becomes especially relevant if we take into account that during operations specifically on the maxillofacial area, surgeons are especially faced with the task of finding a compromise between choosing the optimal access to carry out the maximum possible radical intervention and causing the least possible aesthetic damage to the patient’s face.
Particular diagnostic issues
Currently, thanks to the introduction of ultrasound diagnostic technologies into obstetric practice, the maxillofacial area becomes an object of medical interest even before the birth of the child. This makes available the intrauterine detection of clefts and other malformations of the fetal face and neck, a number of syndromes with facial signs (Down syndrome, Turner syndrome, Goldenhar syndrome, etc.), as well as recognition of teratomas, hemangiomas and lymphangiomas of the fetus.
Timely detection of these changes forces in some cases to reconsider the approach to pregnancy management tactics or to provide for the need to carry out certain organizational, tactical and therapeutic measures in the perinatal and neonatal periods. This concerns, in particular, the expansion of the obstetric team with the involvement of maxillofacial surgeons to provide specialized care as early as possible.
Ultrasound examination makes a significant contribution to the diagnosis of diseases of the major salivary glands.
In inflammatory diseases of the parotid glands, echography allows for differential diagnosis of various forms of mumps, identifying sialodochitis - inflammation in the ducts of the salivary glands, recognizing inflammation of the intraglandular lymph nodes (lymphadenitis) and clarifying its stage. All this is essentially a distinction between surgical and non-surgical pathology of the parotid glands (Fig. 1-7).
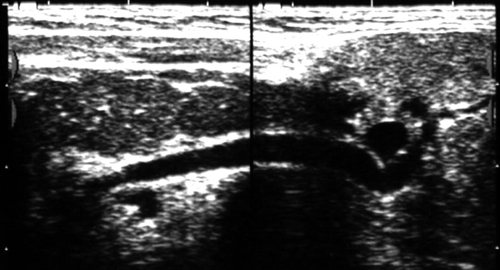
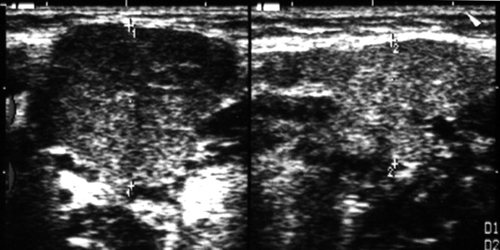
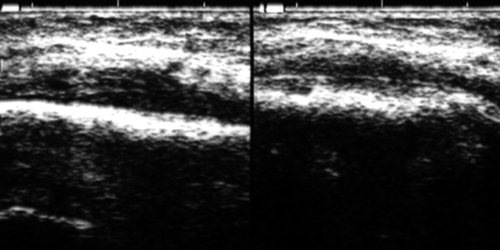
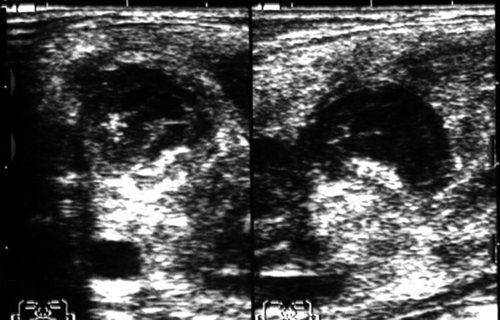
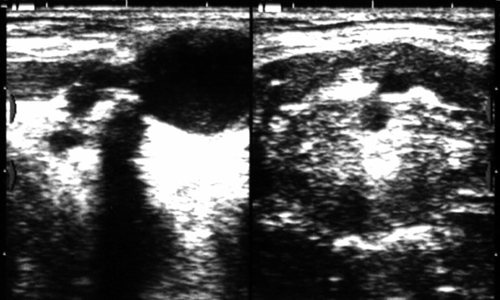
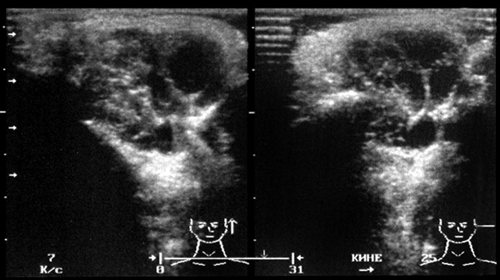
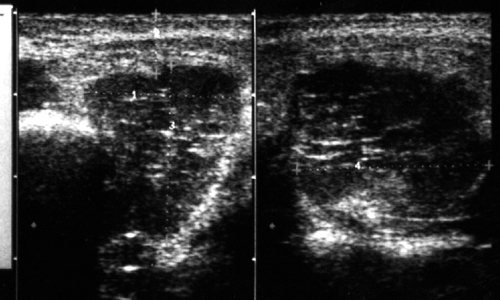
Rice. 1.
Right-sided acute parotitis.
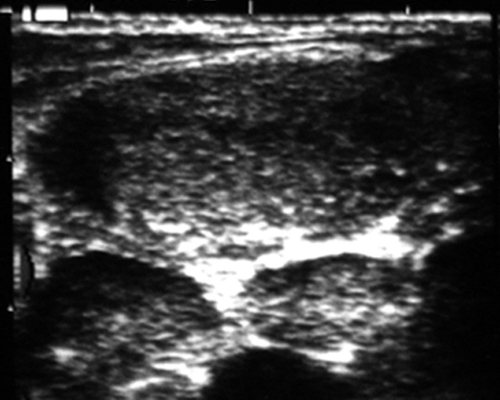
Rice. 2.
Left-sided chronic parenchymal parotitis.
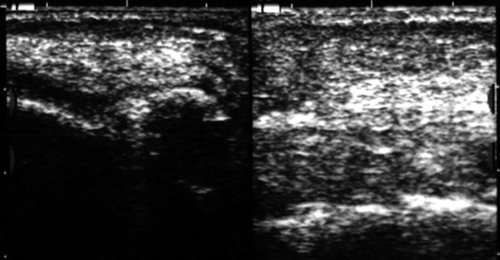
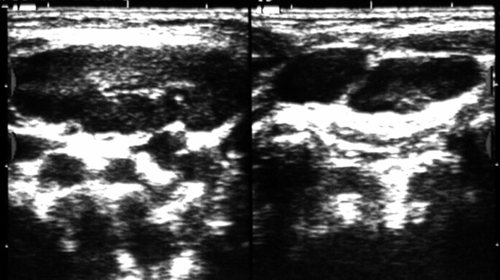
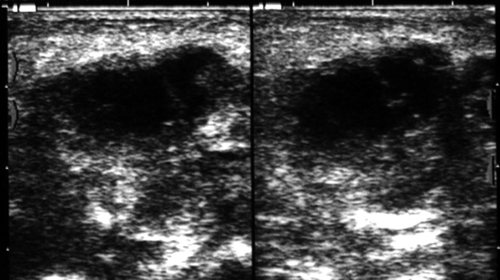
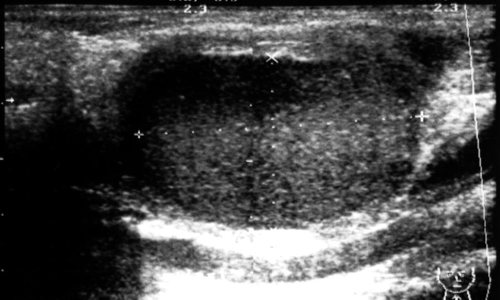
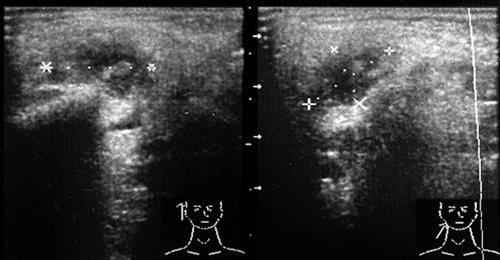
Rice. 3.
Sialodochitis of the left submandibular gland.
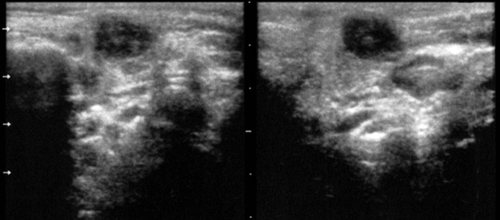
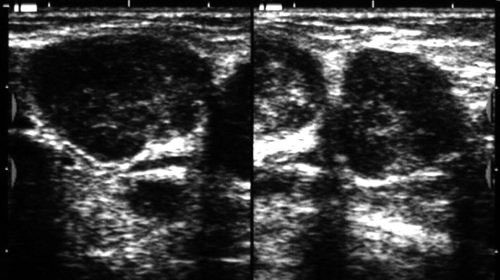
Rice. 4.
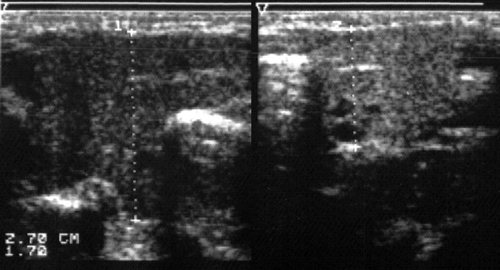
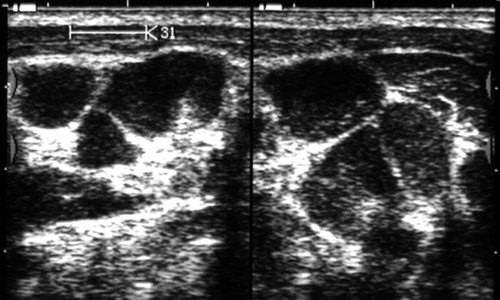
Acute serous lymphadenitis in the left parotid gland (in two scanning planes).
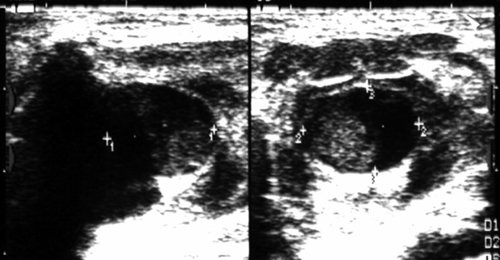
Rice. 5.
Acute serous lymphadenitis in the left parotid gland with limited periadenitis.
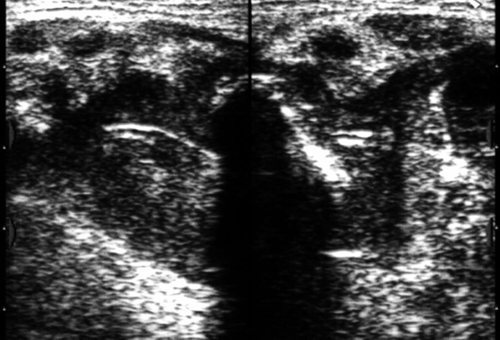
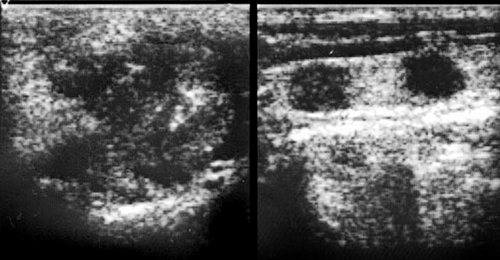
Rice. 6.
Acute serous lymphadenitis with widespread periadenitis (lymphogenous mumps, Herzenberg's mumps) in the left parotid gland.
Rice. 7.
Purulent lymphadenitis in the parotid gland (parotid abscess).
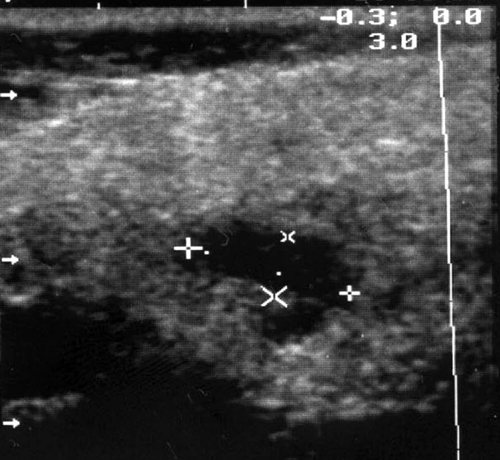
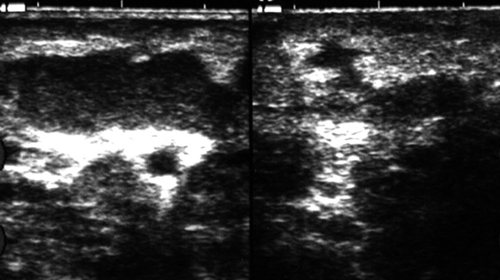
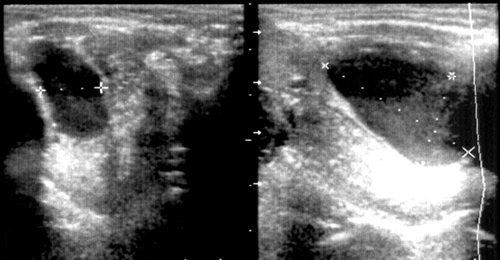
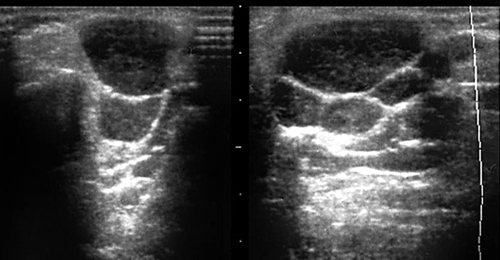
In salivary stone disease, which is most often found in the submandibular glands, ultrasound allows one to identify stones regardless of their location (in the parenchyma of the gland, intraglandular ducts, excretory duct) and the degree of their mineralization, to clarify the presence of sialadenitis - inflammation of the parenchyma of the gland, which can be independent or accompanying salivary stone disease (Fig. 8-11).
Rice. 8.
Salivary stone disease. Calcified calculus in the area of inflection of the excretory duct (typical location) of the left submandibular gland. Associated sialadenitis.
Rice. 9.
Salivary stone disease. Uncalcified calculus in the ampullary part of the excretory duct of the submandibular gland.
Rice. 10.
Salivary stone disease. Calcified stones in the parenchyma of the left submandibular gland. Perifocal edema of the gland parenchyma.
Rice. eleven.
Sialadenitis of the right submandibular gland.
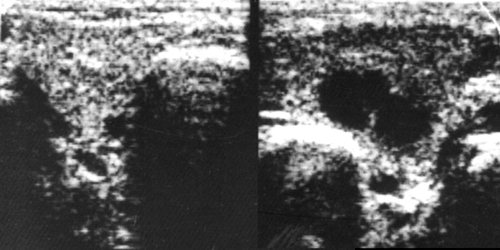
The use of echography in extraorgan inflammatory processes on the face and neck makes it possible to distinguish purulent (abscess, phlegmon) and non-purulent (infiltrate) lesions of soft tissues, and when a purulent lesion is detected, accurately localize accumulations of pus (Fig. 12-14).
Rice. 12.
Infiltration of the left buccal area.
Rice. 13.
Phlegmon of the submandibular region after opening and drainage (drainage is visible).
Rice. 14.
Abscess of the submandibular region.
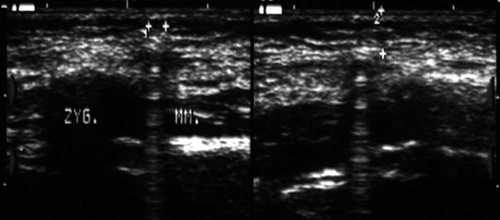
Visualization of the outer (vestibular) surface of the jaw bones makes it possible to establish periostitis, which is one of the most common causes of inflammatory changes in the soft tissues of the face (Fig. 15).
Rice. 15.
Serous periostitis of the lower jaw on the right. Infiltration in the soft tissues of the right cheek.
The exceptionally developed lymphatic system of the face and neck brings significant specificity to the spectrum of diseases in this area. This applies to both inflammatory and non-inflammatory lesions of the lymph nodes. An echo-graphic study allows one to visualize altered lymph nodes and, based on a number of reference signs (the number of altered nodes, their size, shape and proportions, the nature of the contours, the presence or absence of inclusions and their distribution in the node, the degree of decrease in echogenicity) to reconstruct with a high degree of reliability what is happening in the lymphatic node processes.
In the structure of inflammatory diseases of the soft tissues of the maxillofacial region, inflammatory lesions of the lymph nodes occupy one of the first places. An echographic examination allows one to reliably distinguish reactive (inflammatory) hyperplasia of the lymph nodes from their true inflammation - lymphadenitis (Fig. 16-18).
Rice. 16.
Acute reactive (inflammatory) hyperplasia of the lymph node of the neck.
Rice. 17.
Chronic reactive (inflammatory) hyperplasia of the lymph node of the neck.
Rice. 18.
Acute serous lymphadenitis of the neck.
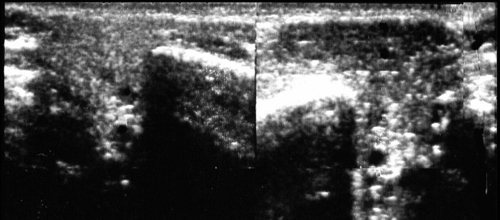
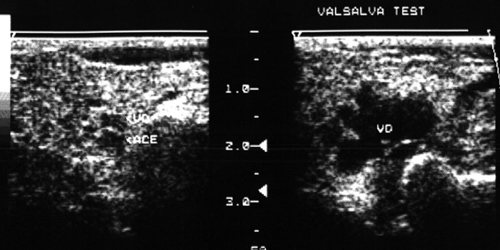
The key point in choosing a treatment method for lymphadenitis is to determine the nature (stage of development) of the inflammatory process: serous or purulent lesion of the lymph node. Ultrasound examination, even in B-mode, makes it possible to resolve this issue with a high degree of reliability, and the use of blood flow visualization techniques (color Doppler mapping, power Doppler mapping) makes it possible to identify the process of purulent melting at its earliest stage (Fig. 18-21).
Rice. 19.
Purulent lymphadenitis of the neck with periadenitis.
Rice. 20.
Purulent lymphadenitis of the submandibular region.
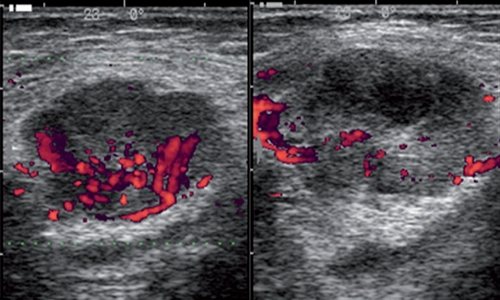
Rice. 21.
Dopplerographic dynamics of the process of purulent melting of the lymph node (over 3 days).
All this makes it possible to rationally approach the combination of methods of conservative therapy and surgical treatment, to choose adequate treatment tactics, avoiding the use of unjustified treatment methods. In everyday practice, metastatic lesions of the lymph nodes of the neck are often encountered, as well as their involvement in the pathological process in lymphoproliferative diseases. An echographic examination makes it possible to distinguish these groups of diseases with a high degree of reliability and differentiate these types of lesions from inflammatory changes in the lymph nodes.
In case of injury from glass, wooden and plastic objects, as well as after gunshot wounds and road traffic accidents, foreign bodies often remain in the soft tissues of the face and neck, the timely detection of which allows for the most effective primary surgical treatment of the wound and reduces the risk of inflammation.
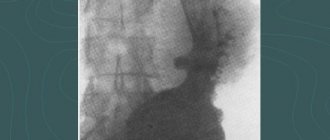
After gunshot wounds, multiple and, as a rule, metallic foreign bodies usually remain in the soft tissues, the high radiopacity of which allows traditional X-ray examination to see even the smallest of them and determine their skeletotopy. In these cases, echography, of course, is inferior to x-ray examination in determining the number and size of foreign bodies, but ultrasound examination is certainly necessary to clarify their organotopy in relation to soft tissue structures - vascular bundle, muscles and fascia.
In cases where there are glass, plastic or wooden foreign bodies in the soft tissues, echography is essentially the only method that allows you to study the infiltration zone, obtain an image of foreign bodies, determine their number, size, location and organotopy (Fig. 22- 26).
Rice. 22.
Foreign body in the soft tissues of the left parotid-masticatory region (metal ball - air gun bullet).
Rice. 23.
A foreign body in the subcutaneous tissue of the left cheek is a glass fragment.
Rice. 24.
A foreign body in the left cheek area is a splinter.
Rice. 25.
Foreign bodies in the keloid scar of the lower lip are small stones and asphalt crumbs (after a traffic accident).
Rice. 26.
A foreign body in the submandibular region is a fragment of a plastic catheter.
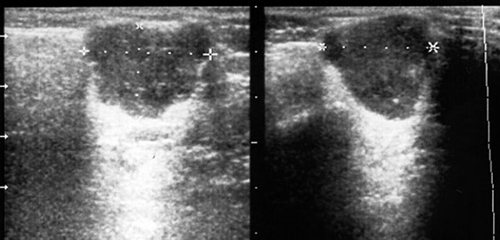
A significant proportion of diseases of the maxillofacial area are congenital cysts of the neck and oral cavity. An echographic examination makes it possible to visualize them, clarify their structure and organotopic characteristics, on the basis of which differential diagnosis is based.
Among congenital cysts of the neck and oral cavity, there are: thyroglossal (middle) and branchial (lateral) cysts and fistulas, retention cysts of the sublingual gland, as well as dermoid cysts.
The urgent need for distinctive recognition of the group affiliation of congenital cysts and fistulas is dictated by the necessity of their radical excision in order to avoid relapse. And if dermoid cysts and retention cysts of the sublingual gland are characterized by a clear demarcation and absence of fistulous tracts, then thyroglossal cysts usually have a connection with the hyoid bone and the root of the tongue, and branchial cysts are often connected by a fistulous tract with the lateral wall of the pharynx (Fig. 27-30).
Rice. 27.
Thyroglossal (median) cyst of the neck. There is a connection with the hyoid bone and the root of the tongue.
Rice. 28.
Branchial (lateral) cyst of the neck. Relationship with the vascular bundle of the neck (compression of the internal jugular vein and displacement of the common carotid artery).
Rice. 29.
Dermoid cyst of the floor of the mouth.
Rice. thirty.
Retention cyst of the right sublingual gland.
Clinicians are well aware of the difficulties in distinguishing between festering cysts and abscessing lymphadenitis. The specificity of the echographic picture makes it possible not only to solve emerging differential diagnostic difficulties, but also to determine the severity of scar changes around the cyst.
Congenital cysts of the neck and oral cavity often have to be differentiated from the cystic form of lymphangioma, which is essentially a malformation of the lymphatic vessels. Cystic lymphangioma is more characterized by multiple chambered cavities or multiple cyst-like formations, as well as significant prevalence. All these signs are clearly identified echographically. In cases of single-chamber and limited prevalence of lymphangioma, differential diagnosis is significantly difficult (Fig. 31).
Rice. 31.
Lymphangioma of the left parotid gland.
In the face and neck area, pathological formations from blood vessels are often found - so-called “hemangiomas”, which in most cases (up to 95-97%) are vascular hyperplasias and vascular malformations (angiodysplasias). True vascular tumors occur only in 3-5% of cases.
In this case, either only the vascular periphery - capillaries, or only larger vessels with the formation of arteriovenous communications (stomachs, fistulas) can be involved in the pathological process; a combination of these options is possible. Dysplastic changes can be localized only in the venous part of the vascular bed; this type of lesion is referred to as “venous dysplasia” (Fig. 32).
Rice. 32.
Venous dysplasia of the right parotid gland.
Vascular formations can have a diffuse distribution in soft tissues or be clearly demarcated, and also have their own hemodynamic characteristics (Fig. 33).
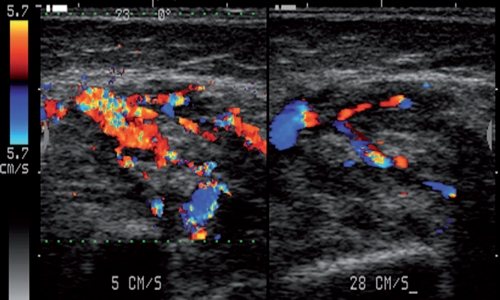
Rice. 33.
Vascular hyperplasia of the right buccal region.
All these factors entail the need for an individual approach to the choice of treatment method and tactics. Ultrasound examination, allowing to determine the main morphological and hemodynamic parameters of vascular formations of the face and neck, is an effective method for their diagnosis.
A very significant role belongs to echography in recognizing tumors of the salivary glands. The possibility of a detailed assessment of the contours of the neoplasm and its internal structure (echostructure) makes it possible to distinguish benign tumors of the salivary glands from malignant tumors with high reliability (Fig. 34-36).
Rice. 34.
Polymorphic adenoma of the left parotid gland.
Rice. 35.
Lipoma of the left parotid gland.
Rice. 36.
Malignant tumor of the right parotid gland (histologically: undifferentiated carcinoma).
Of great importance in clarifying the nature and extent of the tumor process is also the assessment of the condition of the regional lymph nodes, in which echographic examination is a recognized leader (Fig. 37).
Rice. 37.
Malignant tumor of the left parotid gland (histologically: adenoid cystic carcinoma). Metastatic lesions of regional lymph nodes.
The abundance of lymphoid tissue in the parotid glands determines the high frequency of their damage by benign and malignant lymphoproliferative diseases, which also have their own characteristic echographic signs (Fig. 38-39).
Rice. 38.
Damage to the left parotid gland due to lymphoproliferative disease (histologically: lymphogranulomatosis).
Rice. 39.
Damage to the lymph nodes of the neck due to lymphoproliferative disease (histologically: lymphosarcoma).
Without in any way contrasting ultrasound of the maxillofacial area with the traditional clinical examination of the patient, there is every reason to assert that the use of echography is certainly indicated not only in diagnostically unclear cases, but even with an already established diagnosis, when the method allows us to identify individual characteristics of the course of the disease , which can be significant when planning a patient’s treatment.
The non-invasiveness and harmlessness of ultrasound examination makes it possible to carry it out many times to monitor the dynamics of the pathological process and evaluate the effectiveness of treatment measures.
The high information content of an echographic examination (reaching 95-98% in general) makes it possible to limit the use of radiological techniques (traditional radiography, sialography, angiography), significantly less often use invasive diagnostic interventions (soft tissue biopsy) and more rationally approach the use of such expensive studies as computer and magnetic resonance imaging.
Ultrasound machine RS85
Revolutionary changes in expert diagnostics.
Impeccable image quality, lightning-fast operating speed, a new generation of visualization technologies and quantitative analysis of ultrasound scanning data.
Why do they contact us?
- No queues
No need to wait, we work by appointment
- All in one day
Doctor's appointment, diagnosis and treatment on the day of treatment
- Let's relieve the pain
We will help you relieve pain in just 1-2 visits to us
- We guarantee
Professional approach, affordable prices and quality
- Doctor's appointment 0 RUB!
During course treatment all consultations are free
- Three treatment options
We will select several options and offer optimal treatment
FAQ
- Is it painful to have an ultrasound examination?
No, this is a non-invasive and painless diagnostic method.
- Will ultrasound be enough to make a diagnosis?
It all depends on the disease; for some diseases, only an ultrasound is sufficient, while others will require a more in-depth examination, such as magnetic resonance imaging or blood tests.
- Does ultrasound replace radiography of the joint?
No, ultrasound does not make it possible to assess the nature of the bone fracture, the presence of fragments and displacement. Therefore, in case of injuries and suspected fracture, it is better to first conduct an X-ray diagnosis.
- How is ultrasound of joints and soft tissues performed?
Everything is extremely simple: the doctor applies a special gel to the area under study, this gel helps ultrasound penetrate the tissue, and with the help of a sensor examines the tissues and processes occurring under the skin.
- How often can an ultrasound be done?
The ultrasound diagnostic method is absolutely harmless; if necessary, it can be done as many times as necessary.
- Is it possible to consult a specialist after an ultrasound?
Yes, you can get advice from a specialized specialist - a traumatologist, orthopedist, physiotherapist or sports doctor. You can also undergo treatment with us, and you can start on the same day you contact us.
Is preparation necessary?
Before MRI of soft tissues, it is necessary to warn the doctor about possible contraindications and concomitant diseases. The presence of a pacemaker, insulin pump, vascular clips and other medical devices should be reported.
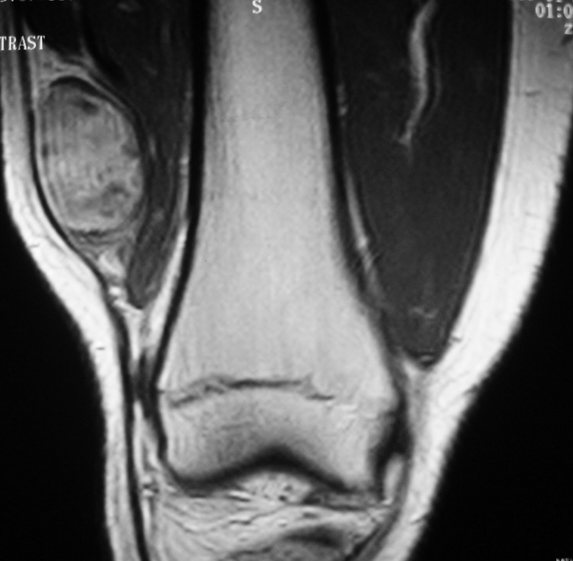
Soft tissue sarcoma of the thigh on MRI
Women who suspect pregnancy undergo additional examination to clarify the condition. The native procedure is contraindicated in the first trimester; contrast MRI is not prescribed during gestation.
Nursing mothers express milk for their baby before undergoing enhanced tomography. After the administration of contrast, it is forbidden to put the baby to the breast for 6-12 hours.
Soft tissue MRI does not require a special diet. The patient is advised to adhere to a normal diet. Restrictions apply to the consumption of alcoholic beverages: alcohol is excluded 2-3 days before the procedure.
An hour before your contrast MRI, you should have a light snack. Before scanning, the patient removes jewelry, accessories, and metal piercings.