Immunoglobulin A is an indicator of humoral immunity. It is determined to assess local immunity, the course of acute infectious processes, kidney diseases, liver diseases, and chronic inflammation. At the Yusupov Hospital, laboratory technicians use high-quality reagents to determine the level of immunoglobulins A. The results of the study are interpreted by professors and doctors of the highest category. Immunologists carry out therapy aimed at normalizing the concentration of immunoglobulins A. Therapists use effective drugs registered in the Russian Federation, which have minimal side effects.
Immunoglobulins A are proteins that provide local immunity. They are presented in the human body in two fractions: serum, which provides local immunity, and secretory. The secretory fraction is contained in milk, respiratory and intestinal secretions, tear fluid and saliva, which, together with nonspecific immune factors, protect the mucous membranes from viruses and bacteria.
Functions
Serum immunoglobulin A is a fraction of gamma globulins. It makes up 10-15% of the total amount of all soluble immunoglobulins. In blood serum, immunoglobulin A is represented mainly by monomeric molecules. The main amount of immunoglobulin A is not found in the blood serum, but on the surface of the mucous membranes. Secretory immunoglobulin facilitates the transport of immunoglobulin A across the epithelium. It protects immunoglobulin molecules from breakdown by digestive tract enzymes.
The main function of serum immunoglobulin A is to provide local immunity, protect the genitourinary, respiratory tract and digestive organs from pathogens of infectious diseases. Secretory antibodies have a pronounced anti-adsorption effect: they prevent the attachment of bacteria to the surface of epithelial cells, prevent the adhesion of microorganisms, without which bacterial damage to the cell becomes impossible. Also, immunoglobulins A, together with nonspecific immune factors, provide protection of mucous membranes from microorganisms. Congenital or acquired deficiency of immunoglobulin IgA can lead to allergies, autoimmune disorders, allergies, and repeated infections.
Immunoglobulin A does not cross the placental barrier. Its level in newborns is about 1% of the concentration in adults. By the first year of a child’s life, this figure is 20% of the adult level. After the baby is born, secretory immunoglobulins enter his body with the mother's colostrum. They protect the child’s gastrointestinal tract and respiratory tract. The age of 3 months is critical. During this period, doctors diagnose congenital or transient deficiency of local immunity. By the age of five, the level of immunoglobulin A reaches the concentration characteristic of an adult.
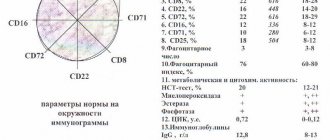
The level of immunoglobulin A in children depends on their age. In children from 3 to 12 months it is 0.02-0.05 g/l, from 12 to 16 years it is in the range of 0.6-3.48 g/l. In adults over 20 years of age, the normal level of immunoglobulin A varies from 0.9 to 4.5 g/l.
Types of diseases
This syndrome can be either primary (genetically determined) or secondary (appears due to external factors or diseases).
Primary immunodeficiency in children - what is it and where does it come from?
Congenital immunodeficiency (ID) in a child is something that develops due to genetic factors; these are primary disorders of the immune system. As a result, severe infections develop that quickly become chronic, and organs and tissues are affected by inflammatory processes. Without treatment, primary immunodeficiency leads to death in children from complications of various infectious diseases.
Symptoms of primary immunodeficiency may not be detected in children because the disease does not have unique features. This may be a simple but often recurring infection, for example of the lungs or ENT organs, or problems with the gastrointestinal tract, inflammation of the joints. Often neither parents nor doctors realize that all these problems are the result of a defect in the child’s immune system. Infectious diseases become chronic, complications appear, and there is no response to a course of antibiotics. Typically, severe forms of immunodeficiency are visible immediately after the birth of the baby or after some time. Source: Doan Thi Mai Recurrent infections in children - the risk of immunodeficiency // Pediatrician, 2021, vol. 8, special issue, pp. 109-110
It is important to distinguish primary immunodeficiency from AIDS. The second is a viral, acquired disease, and the primary form is already “implanted” into the body due to genetic defects.
Why does a child develop secondary immunodeficiency, and what is it?
Such a disease is also a disorder in the functioning of the immune system; it appears in children and adults and is not the result of defects in genes. Secondary immunodeficiency can be caused by a number of factors - external and internal. Any external unfavorable factors that disrupt the metabolic process in the body can lead to the development of such a pathology. The most common of them:
- poor environment, dirty air;
- ionizing radiation, microwave exposure;
- acute poisoning in chronic form;
- long course of certain medications;
- chronic fatigue, stress. Source: M.V. Kudin, S.A. Sergeeva, A.V. Skripkin, Yu.N. Fedorov Prevention of morbidity in children with secondary immunodeficiency in disadvantaged environmental regions // Bulletin of VolSMU, 2009, No. 1(29), pp. 87-95
All these factors have a complex effect on the body and all its systems, including the immune system. And such as ionizing radiation, selectively inhibit the hematopoietic system. People living in conditions of environmental pollution have reduced immunity, they are more likely to suffer infections, and the risk of developing cancer increases. .
Indications
With the help of immunoglobulins A, doctors assess the course of diseases that occur with activation of the immune system:
- acute and chronic infections of bacterial and viral origin; bronchial asthma;
- oncological diseases of the lymphatic system (leukemia, myeloma);
- connective tissue diseases (systemic lupus erythematosus, rheumatoid arthritis).
Immunoglobulin IgA is determined in the presence of the following diseases:
- recurrent bacterial respiratory infections (sinusitis, pneumonia), as well as otitis and meningitis, bronchial asthma;
- chronic diarrhea, malabsorption syndrome;
- anaphylactic post-transfusion reactions;
- Louis-Bar syndrome (ataxia - telangiectasia);
- tumor diseases of the lymphoid system (myeloma, leukemia, reticulosarcoma, lymphoma).
- chronic hepatitis, liver cirrhosis.
Using IgA immunoglobulin testing, doctors at the Yusupov Hospital check the functioning of the liver, stomach, intestines, and lymphatic system.
Immune “army” that will protect the child
The immune system, like a real army, is made up of many components, each of which plays a unique role in protecting the body from attacks by the “enemy.” There are several types of leukocytes that circulate in the blood and, if necessary, penetrate (migrate) into the tissues of the body to perform their protective functions. When these cells detect bacteria or viruses, they produce chemical alarm signals known as cytokines. These chemicals encourage other white blood cells to join the fight against the pathogen, and control other aspects of the immune response, such as fever and increased blood flow to the site of infection, which causes inflammatory responses such as swelling, redness and pain.
Some white blood cells produce antibodies - proteins that bind to a specific part of the infectious agent, leaving a target mark on it for its destruction. When the immune system fights a new infection, it creates antibodies against that specific pathogen. Once the infection is over, the immune system usually continues to produce these antibodies for many years or decades into the future. It is this “memory” function of the immune system that prevents re-infection with diseases such as chicken pox or measles. Preventive immunization through vaccinations is based on the same “immune memory” effect.
Some other infections (most often bacterial or fungal) stimulate only a short-term immune response, as a result of which long-term immunity to infection becomes impossible, and a child who has had such certain diseases may become ill again. In addition, some pathogens have several strains, each of which is so different from the other that acquired immunity to one strain is not able to protect against others. This is why a child may get colds or flu again and again. Just like in a real army, all cells in the human body wear “insignia” that allow the immune system to distinguish them from “invading invaders.” On the outer surfaces of the body's cells there are signs - proteins that help the immune system distinguish between the body's own cells and pathogenic microorganisms that need to be destroyed.
Collection of biomaterial for research
In order to determine the level of immunoglobulin A, venous blood is collected into an empty tube or with gel (to obtain serum). Patients with low levels of immunoglobulins on the eve of the study should take measures to prevent bacterial infection. The venipuncture site is pressed with a cotton ball until the bleeding stops. If a hematoma has formed at the site of the vein puncture. Apply a warm compress.
The patient is advised to refrain from eating for 12-14 hours before the test. He can drink pure still water. Doctors stop medications that may affect the results of the study. 3 days before taking blood, the patient must stop drinking alcohol. Analysis results can be obtained within 4 hours.
Diagnostics of ID
A family history and complaints of the child (if he is not a newborn), an examination, as well as a number of laboratory tests are collected: molecular genetics, clinical blood test, etc.
Important! If the family already has a child with primary immune deficiency, then prenatal diagnosis is extremely important when carrying a second one.
Signs and symptoms of primary immunodeficiency are detected in children already in the first weeks of life. When a doctor collects anamnesis, he pays special attention to the frequent incidence of viruses and bacterial infections, to heredity aggravated by disorders of the immune system, to congenital malformations.
Often such pathology is detected much later and by chance, when other tests are performed.
The main methods for diagnosing both congenital and acquired disorders of the immune system:
- examination of the child, during which special attention is paid to the condition of the skin, as there may be fungal infections, erosions, dystrophy, ulcers, swelling of different parts of the body;
- blood tests - pathology is indicated by a violation of the leukocyte formula;
- special immunological studies;
- molecular genetic analysis.
Reasons for the increase
Immunoglobulins A bind to microorganisms and delay their attachment to the cell surface. A decrease in the content of immunoglobulins A indicates a lack of local and general immunity. Their concentration increases in the following diseases:
- acute and chronic infectious processes (fungal, parasitic, bacterial);
- liver pathologies;
- multiple myeloma;
- systemic lupus erythematosus;
- monoclonal gammopathy.
The level of immunoglobulin A decreases in patients suffering from diseases that deplete the immune system. Immunoglobulin A may be low in a child with an acute viral infection
Treatment methods for secondary ID
Immunotropic therapy is mainly used, which can be of different directions:
- active immunization;
- replacement therapy;
- taking immunotropics.
The choice of immunotropic therapy depends on how acute the inflammatory-infectious process is and what immunological defect is identified. When the symptoms of the disease subside, vaccine therapy can be used for prevention.
Immunoglobulins administered intravenously are used as replacement therapy. Their main active ingredient is special antibodies obtained from donors. Immunoglobulins containing only IgG are often prescribed.
Immunotropic treatment of secondary ID
Using immunomodulators, the effectiveness of antimicrobial therapy can be increased. Immunomodulators should be part of complex therapy together with etiotropic treatment of infection. The doctor calculates the regimen and dosage individually.
Immunological monitoring should be carried out while taking immunomodulators. If the infection is in an acute stage, immunomodulators are used with caution. Otherwise, you can cause a severe general inflammatory response and septic shock as a result. Source: G.A. Samsygina, G.S. Koval Problems of diagnosis and treatment of frequently ill children at the present stage // Pediatrics, 2010, v. 89, no. 2, pp. 137-145
Decrease in indicator
Immunoglobulin A is reduced in patients with neoplasms of the lymphatic system, lymphoproliferative diseases, pernicious anemia, and hemoglobinopathies. The content of immunoglobulin A decreases after splenectomy, in case of protein loss due to enteropathies and nephropathies. Treatment with immunosuppressants, cytostatics, and exposure to ionizing radiation can also reduce the level of immunoglobulin IgA.
Long-term exposure to benzene, toluene, xylene, and taking medications: dextran, estrogens, methylprednisolone, carbamazepine, gold preparations, valproic acid can lower the level of immunoglobulin A. Get a consultation with an immunologist by making an appointment by calling the Yusupov Hospital. The doctor will conduct an examination and prescribe a test for immunoglobulin A levels.
So what to do with “immune yoghurts”? is there or not? Let's summarize:
If your child's immune system is functioning normally - responding properly to infections and not showing signs of overreactivity - then nothing special needs to be done. You just need to stop watching advertising and constantly worry unjustifiably “about immunity”, accepting the fact that no matter how hard we try, children will get sick, and no matter how hard pathogenic microorganisms try, children will get better.
Regarding “yogurts” - the food product is intended for nutrition and nothing more. Naturally, eating is healthy, and not eating is harmful. Yogurt does not cure anything; they are treated with medications correctly prescribed by a doctor and sold in pharmacies.
If you are concerned that your child does have a problem with the immune system, talk to your pediatrician or consult an immunologist.
Instead of looking for a “magic pill” to “strengthen immunity,” teach your child to wash his hands very often, love walks and exercise, and carry out routine vaccinations.
These simple measures will bring much more benefits. Call a doctor at home Make an appointment with a doctor or call +7 (812) 331-17-74
How to prepare your child's immunity for kindergarten

Those who are just planning to go to kindergarten should know the basic rules for strengthening children's immunity:
- Regular ventilation of the children's room. This will help destroy some of the pathogenic bacteria and also enrich the air with oxygen.
- Using humidifiers. This is especially true in the winter season when heating devices are on. The baby's nasal mucosa must remain moist in order to trap some of the viruses that enter the body.
- Hardening. Its essence is to accustom the growing body to sudden changes in temperature. Then your child will not get sick, even if he overheats in kindergarten before going for a walk.
- Compliance with the drinking regime. It's rare that a child will refuse sweet soda, but it is unlikely to benefit his immune system. Try to accustom your baby to vitamin drinks - rosehip decoction, kefir, homemade fruit juice.

If you want to get a full consultation on strengthening children's immunity, as well as determine its current level, we recommend scheduling a consultation with a Rixos PR pediatrician. We will tell you how you can make your baby healthier and prevent a number of diseases. And at the same time we invite you to relax with the whole family in a cozy corner of the Carpathian region!
Causes of decreased immunity in children

The main reasons for a sharp weakening of the immune system in children of preschool and school age are diseases, their complications, as well as severe stress.
Before figuring out how to improve a child’s weak immunity, it is important to establish why it has decreased. This may be due to:
- Physical and mental fatigue. Therefore, before sending your child to a fashionable lyceum, or enrolling in various sections, think about whether he will cope with such a rich program.
- Chronic lack of rest and constant lack of sleep. Unfortunately, gadgets can steal time that kids can use more efficiently: for games and sleep. Only a clear daily routine will help combat this. Please note that babies need to sleep a little more time in winter than in summer. This is due to the length of daylight hours.
- Lack of oxygen. It is observed in children who spend all day indoors and rarely walk outside.
- Physical inactivity. If you are afraid that your baby will get injured during active street games, and he flatly refuses to do morning exercises, offer him an alternative. Dancing is a great way to relieve stress and increase physical activity!
- Poor food. Yes, children love junk foods: chocolate, baked goods, French fries and other fast food. But if you unobtrusively offer them juice or fruit, they will happily gobble it up. When creating a diet, remember that children do not evaluate food based on its usefulness. It is important to them that it is tasty or beautifully decorated.
- Dehydration of the body. Usually children drink water before and after meals, guided by their own desires. But sometimes they are sorely lacking moisture. Therefore, along with plain water and teas, offer your child a herbal decoction (for example, chamomile), compotes and juices, as well as jelly, uzvar, etc. It's both tasty and healthy.

It is important to know : in preschool age (up to 6-7 years), the child’s immune system is actively developing. Therefore, for the cold season, 8-10 cases of colds are considered normal. At school, the number of diseases is reduced by approximately 2-2.5 times. The next “dangerous” period occurs during puberty (13-15 years).
Which children are considered to be frequently ill?
Why was the term “frequently ill children” introduced?
For example: in the UK it is believed that a child can be classified as frequently ill if he gets sick eight times a year.
We have more stringent criteria. A child is considered to be frequently ill if:
- a child under one year old gets sick more than 4 times a year;
- a child from one to three years old gets sick more than six times a year;
- a child from three to seven years old gets sick more than 8 times a year;
- if the child is older than seven or eight years old, and he gets sick more than 4 times a year.
Causes of low immunoglobulin E class
Immunoglobulin E, as previously mentioned, takes part in allergic reactions. However, its second function is no less significant: antibodies of this class provide protection against parasitic infections.
There are two types of deficiency
:
- Selective IgE deficiency
- characterized by a significant decrease in its concentration in plasma: less than 2.5 mU/ml or 8 ng/ml, provided that levels of antibodies of other classes are normal.
- Mixed IgE deficiency
- with a simultaneous decrease in the concentration of other classes of immunoglobulins.
The results of a recent study on the connection between this pathology and Helecobacter infection, which is associated primarily with the development of gastritis and its further more serious complications, are interesting. However, unfortunately, the already proven fact that this type of bacterium, penetrating the gastric mucosa, causes powerful, both local and systemic, production of antibodies and the implementation of protective reactions from cellular immunity, is not so often paid attention to.
This pathogenic microorganism binds to mast cells, causing them to produce multidirectional pro-inflammatory signaling molecules - cytokines. This is partly facilitated by IgE, which continuously activates the previously mentioned connective tissue cells.
Study
: Helicobacter pylori infection in patients with selective immunoglobulin E deficiency
A low concentration of IgE can be a consequence of congenital pathologies caused by a gene or chromosomal mutation ( ataxia-telangiectasia, Bruton's hypogammaglobulinemia
), and accompany acquired diseases:
- chronic fatigue syndrome;
- autoimmune diseases;
- arthralgia.
Treatment and prevention of immunoglobulin deficiency
With a complete deficiency of immunoglobulins, caused by certain congenital mutations that occur in the genes responsible for the regulation of this process, the artificial introduction of donor antibodies does not achieve the desired result, but only aggravates the course of the disease - an allergic reaction occurs
.
Remember about immunological tolerance - the inability of the immune system to produce antibodies against its own antigens (with the exception of barrier organs, of course). This is a kind of condescension on her part, the seeds of which are laid during embryonic development - she encounters various molecules and, in the end, develops a clear rule: “these are our own” and “these are strangers.”

But in the initial absence of antibodies in the body - say, class A - immunocompetent cells are deprived of this opportunity: they have never encountered them before, in their complexly programmed database centers there is no mention of this substance as their own - and, therefore, they begin to the most logical solution to the problem in this situation: the destruction of foreigners.
We recommend
“Metabolic syndrome: causes, symptoms, treatment and prevention” Read more
Yes, it sounds paradoxical: immunoglobulins versus antibodies
- but this is not oil or a play on words, but a real process that occurs for very understandable reasons and mechanisms, on which, by the way, some methods of serological diagnosis of certain diseases are based.
In general, selective immunodeficiency does not always require intervention from doctors, especially if it is asymptomatic. For more severe pathologies of the immune system, which are usually detected in the first years of life, either a thymus gland transplant is performed, or immunoglobulin injections and antibiotics are prescribed as a preventative measure for bacterial diseases.