Text: Tatyana Neeshpapa.
This article was published on the website “Rumyantseva, MD”, 10/21/18.
Has anyone ever had a situation where there was a need to have an X-ray of any part of the body during pregnancy?
Unfortunately, none of us are immune. Including during pregnancy.
A pregnant woman may develop pneumonia, tuberculosis, break a leg, or suffer other injuries. She may need dental care.
Features of dental x-ray
Dental radiography has several types. The choice of a specific type of dental x-ray during pregnancy, as well as without it, is influenced by the purpose of the study (whether it is possible to do x-rays in principle is decided by the doctor).
If you need to see the structure of the jaw, examine the entire upper and lower dentition, assess the condition of the gums and bone tissue, it is best to do orthopantomography. In another way, such an X-ray is called a “panoramic image.”
If the doctor is only interested in one specific tooth (or several adjacent ones) and its features, it is better to take a targeted picture using a computer visiograph.
Both of these X-ray diagnostic methods are characterized by minimal radiation exposure, so if there is an urgent need, one of them can be prescribed to a pregnant woman (preferably in the second trimester).
Security measures
Before X-rays are taken, the patient must wear a protective vest or apron. Inside it is a lead plate that blocks the X-rays and prevents them from affecting areas that are not being diagnosed.
Before any type of x-ray, the patient should remove metal objects from himself, as they can interfere with the passage of x-rays, which will negatively affect the quality of the image.
Contraindications
It is generally accepted that the first trimester of pregnancy is a contraindication for dental x-rays. It is in the initial period that all the organs and systems of the child are formed, and in no case should you interfere with this process or interfere with it. Even if a woman has a certain pathology of the oral cavity that requires detailed diagnosis, x-rays are usually postponed until the second trimester.
When can you do without a photo?
When dental caries is visible to the naked eye or gum pathology is clearly visible, the dentist can begin treatment without an x-ray.
If the patient is diagnosed with cementoma, an abscess has developed, or multiple cysts have formed, the x-ray may turn out dark and uninformative. In this case, there is no point in going through such a procedure.
Features of the influence of x-rays in the early stages
X-rays are most dangerous during the first 2 months of pregnancy. According to medical research, after the 16th week of pregnancy, rays are not able to provoke developmental defects in the developing baby, but this does not mean that after this time a woman can be exposed to radiation uncontrollably.

In general, radiography can be classified into 3 main hazard groups. Information regarding these points is given in the following table.
Table. Classification of radiography by degree of danger
| Group | Description |
| The most dangerous x-ray examinations | The greatest harm to the expectant mother and the child developing inside her comes from x-ray examinations of the abdominal cavity and spine, as well as the pelvis. Under these conditions, the rays pass directly through the child. |
| Medium risk examinations | Less dangerous compared to the examinations described above, but still requiring caution and maximum attention, are x-ray examinations of the lungs, limbs, head, and chest. There is no direct irradiation of the fetus, but the mother herself is exposed to fairly strong radiation, and the image covers a fairly large area. |
| Low risk examinations | The following examinations are classified as minimally dangerous: x-rays of the nose and teeth. To carry out such manipulations, special equipment is used, covering a much smaller area compared to standard images. |
In general, doctors always refrain from prescribing X-ray examinations for pregnant patients. The only exception is made in situations where, without an x-ray, the woman’s health and life are at serious risk, or an artificial termination of pregnancy is planned in the future.
Photo of teeth at different times
In early pregnancy (1st trimester)
Why pregnant women should not have dental x-rays done in the first trimester of pregnancy was stated earlier. If a woman had an X-ray examination of her teeth at a time when she did not yet know about her situation, she should not worry too much about this, much less think about what pathologies this will cause in the fetus. In any case, a routine ultrasound will be performed in each trimester of pregnancy, which will show how the child is developing.
In the 2nd trimester
The second trimester has always been considered the safest period of pregnancy. The baby’s organs and internal systems have already formed, and now they are gradually developing and growing. It is during this period that women can be prescribed x-rays (but choose methods with minimal radiation) if there are certain indications.
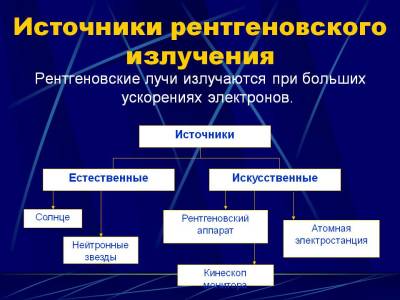
X-ray during pregnancy: basic information
The mechanism of action of such radiation on the body of a pregnant woman has long been carefully studied to the smallest detail. It has been established that a child developing inside a woman is very vulnerable, which is why x-rays, which, as noted, are not entirely safe for adults, can negatively affect the processes of fetal formation.
When X-rays interact with body tissues, the process of water ionization occurs, during which various active radicals are formed. Under the influence of the latter, cell division disorders are observed. The result of such processes is disastrous - chromosomal pathologies appear, as a result of which the cells can either die completely or mutate, turning into genetically inferior or cancerous.
Under the influence of X-ray radiation, tumors, various malformations and other genetic disorders can form in the fetus. The most serious damage occurs when radiation is delivered with a power of more than 1 mSv - in this case, the woman is likely to either have a miscarriage or have a seriously ill child.
In support of the situation described above, experts cite the results of experiments on animals and medical cases recorded after the bombing of the Japanese cities of Hiroshima and Nagasaki - of the women who managed to survive and maintain pregnancy, about 20% gave birth to children with various types of developmental disorders. The most frequently reported defects were the nervous system.
Are there alternatives to MRI?
Is it necessary to do an MRI of the head, neck, pelvis and other parts of the body during pregnancy, or can you use other hardware diagnostic options? In some cases, it is quite possible to choose. For example, if there is a suspicion of diseases of the internal organs, a woman can resort to the already classic ultrasound - it is cheaper, and, like tomography, does not pose any danger. However, there are a number of situations when MRI cannot be done, and the patient must take a risk by choosing radiography.
X-ray or MRI?
Can pregnant women have an X-ray of the brain or pelvis instead of an MRI? When answering this question, you need to carefully weigh all possible consequences. It is no secret that X-ray radiation, having a long-term effect on the body, destroys soft tissues and changes the structure of DNA. However, if you wear metal prostheses or pacemakers, then radiography becomes the only possible option. It is this method, due to its efficiency, that is prescribed for internal bleeding. MRI is not so quick, which can significantly worsen the situation.
Decoding the results
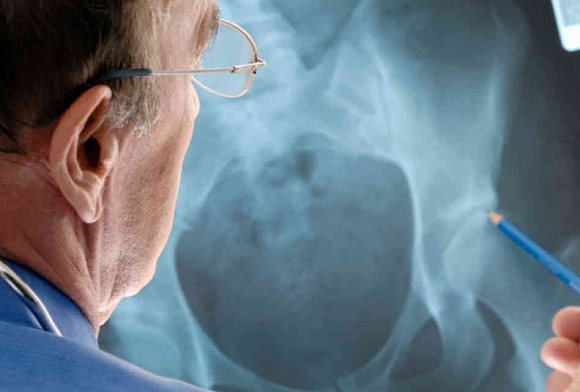
Immediately after the x-ray, the radiologist begins interpreting and describing the images. To do this, he needs to assess the following qualitative and quantitative indicators:
- size of the neck-shaft angle;
- the magnitude of the Wiberg angle and the degree of change;
- the angle of the femoral neck (to identify antetorsion, inclination);
- value of the width of the sacroiliac joint;
- the width of the gap between the bones of the hip joint.
The following additional pathological signs are also accepted for analysis:
- deformation of the femoral head;
- dislocations and subluxations of the hip joint
; - rotation of joint bone fragments;
- displacement of the femur in width or length;
- expansion/constriction of the symphysis.
When interpreting, the radiologist does not make a specific diagnosis. He describes the pathological signs that are visualized in the images, and the attending physician correlates them with other pronounced clinical signs and makes a conclusion about the presence of a particular disease.
Normal indicators
The X-ray image should show a symmetrical image of the two halves of the pelvis, the sacrum, the intervertebral foramina of the sacrum, as well as the branches of the pubic and ischial bones. The bone substance should be clearly visible, the contours of the two acetabulums and the neck of the femur should be visible.
There are certain indicators of the normal condition and structure of the hip joint, with which the actual data are compared when deciphered. For example, the Wiberg angle should normally be located between the line of the center of the femoral head and the superior-outer edge of the acetabulum. The normal angle is approximately 30 degrees. The angle of inclination of the entrance to the acetabulum is also normal - 31-42 degrees. The neck-shaft angle should normally be from 115 to 140 degrees.
x-ray during pregnancy
Tryam, hello! My name is Dasha. I am in my 9th week of pregnancy (according to the date of ovulation) and the 11th obstetric, today I went to the second ultrasound (as part of registration in the residential complex of the Moscow Region city of Klin), the results did not please me at all: they scared me terribly, I sit and I'm shedding tears. Maybe someone had such a situation?
And the situation is as follows:
My last period was on May 20th. On June 15, my jaw hurt terribly and the dentist forced me to take an x-ray. I didn’t know about pregnancy (I started taking tests only on 24 DC, 25 DC and 1 DC - on June 18, 19 and 20), there were no signs at all, so I calmly went for diagnostics. They put me on a protective apron, a photo was successfully taken in two projections, the doctor made a diagnosis and prescribed treatment (anti-inflammatory drugs and procedures with a surgeon). Before I had time to cure my long-suffering teeth, early toxicosis began and my chest began to hurt alarmingly. I did the tests: they, of course, turned out to be positive. I was, of course, incredibly happy (they had planned it since March, but it didn’t work out) and at the same time unpleasantly shocked: after all, I had an x-ray done, endured anesthesia (ultracaine), and took serious medications. What kind of hedgehog will be born now?..
The Internet, oddly enough, reassured me: everything will be fine, blah blah blah. I had my first ultrasound at 4.3 weeks at the Center: I explained my problem to the doctor, who reassured me, saying that the fertilized egg was on time, of the correct shape, in the uterus, the yolk sac was in place - everything was OK! They prescribed me folic acid and lots and lots of fresh vegetables/fruits. I calmed down. Today I came to register at the Klin residential complex, they sent me for an ultrasound:
— Embryo with CTE at exactly 8.5 weeks and SB (heart rate 150 beats/min)
— There are no threats, there is one fertilized egg in the uterus
— Bicornuate uterus (fetus in the right “horn”)
Without explanation or analysis for progesterone, I am prescribed duphaston (1 tablet 3 times a day - a horse dose) and referred to the district gynecologist. She sets up an exchange for me based on the ultrasound (attention, without examination and measurements), asks questions. Asks if there have been any illnesses/x-rays/antibiotics taken in the last 3-4 months. I tell her about the tooth. What begins! She yells that this is 100% 3D, that there will be severe pathologies, that in my case, only for an abortion. I'm crying. Writes me a referral for cleaning! Naturally, I won’t go anywhere: there is a person, there is a heart beating! What, kill him? No!
Please reassure me, girls! Maybe someone had similar cases? How did the pregnancy develop? What to tune in to?
And my Lyalya is such a sweetheart! Look, what kind of abortion is this?.. Photo:
Contraindications for
X-rays of the pelvis and other organs, bones and joints, as numerous studies show, can have a negative impact on the human body. Although, of course, there are very few practical cases of identifying pathologies caused by x-rays. However, there are several contraindications to pelvic x-rays that must be taken into account when prescribing this procedure:
- pregnancy (all trimesters);
- children under 15 years of age;
- serious condition of the patient.
If an x-ray is not advisable, doctors may choose another diagnostic technique that can also be used to assess the condition of the hip joint. For example, MRI or CT.
What is the tactic for referring a pregnant woman for an x-ray?
I want you, as patients, to understand the entire logical chain of a doctor making such a decision.
1. We make a presumptive diagnosis and understand that in this case an x-ray is needed.
2. We make sure that in a particular situation we cannot replace x-rays with another research method (for example, ultrasound).
3. We weigh the risk-benefit ratio for mother and fetus during X-ray examination. We calculate all possible options for the development of the disease and complications.
4. Once again we are convinced that an x-ray is still needed.
5. We send the pregnant woman for an x-ray according to vital indications. During x-rays, we use protection (lead apron) for maximum protection of the fetus - this is called shielding.
6. If a woman refuses an x-ray, we take a written refusal. We explain all possible consequences, complications and variants of the course of the disease if you refuse this study.
7. We draw up a treatment and examination plan in such a way as if our fears, which an x-ray could show, were confirmed. Or we choose a wait-and-see approach (observe), if possible.
7. We use all other research methods to maximally confirm the diagnosis and prescribe correct and adequate treatment!
X-ray examination of the pelvic bones

To most accurately determine pathologies of the pelvic bones, radiography is most often used. This is a simple technique, the result of which is highly informative and accurate. The main advantages of x-rays are:
- accessibility – there is an X-ray machine in almost every clinic;
- painlessness;
- relative safety;
- efficiency - together with decoding, this diagnostic procedure lasts approximately 10 minutes;
- simple preparation for a pelvic x-ray (how to do it will be described below).
Indications for radiography
Indications for pelvic radiography
are:
- traumatic injuries of the hip joint;
- suspicion of a tumor of the hip bones;
- inflammatory diseases of the hip joint;
- suspected pathology of the pelvic ring;
- dislocations of the hip joint.
What does a pelvic x-ray show?
Let's take a closer look at what a pelvic x-ray can show. X-ray of the pelvis and hip joint
may show the following pathologies:
- osteoporosis;
- dislocation and subluxation of the hip;
- fractures of the pelvis, hip joint of various locations and complexity;
- arthritis or arthrosis;
- Perthes disease (osteochondropathy of the femoral head);
- tumor-like neoplasms.
Features of the event
X-ray of the pelvis in men
For men, a pelvic x-ray, as practice shows, can be prescribed as the main procedure for diagnosing prostatitis. In this case, the pathology can be of any type - acute, chronic, bacterial or non-bacterial. The main symptoms of this disease are: pain in the scrotum and perineum, problems with urination, deterioration in sex life, changes in seminal fluid and difficulty in ejaculation.
X-ray of the pelvis in women
For women, a pelvic x-ray can be prescribed as an additional diagnosis of infertility and to identify the causes of disturbances in the functioning of the organs of the reproductive system.
How often should pregnant women have x-rays?
If there is no indication for an x-ray, it should not be done. Even with a fluorographic examination, you can wait if the time has come for a new screening.
Therefore, the issue of the frequency of imaging during pregnancy should be considered from the point of view of extreme necessity and a possible reduction in dosage.
Pregnant women should not be afraid of single images, for example, if a woman breaks her arm, an X-ray of the arm is indispensable. Radiation diagnostics in dental treatment will also be safe.
At the same time, if there is an alternative to x-rays, it is better to use such research methods. Radiation sessions for the treatment of oncological pathologies are prohibited.











