Troponin I
Troponin I
- a highly specific cardiac marker.
Its normal content in blood serum is extremely low. Its level increases within 4–6 hours after the onset of pain in the heart, and continues to persist for up to 6–7 days, reaching a maximum by the second day. This makes it possible to diagnose myocardial infarction not only in the first hours, but also at a later date. Troponins
are small proteins involved in the regulation of muscle contraction. There are two types of troponin: troponin-I and troponin-T, which are structurally different in skeletal and cardiac muscle, so the cardiac-specific forms of these types of troponin can be isolated by immunoassays. For troponins, the ratio of the concentration inside muscle cells to the concentration in the blood plasma is much higher than for enzymes and myoglobin, which makes these proteins highly sensitive markers of myocardial damage.
About 5% of troponin-I inside muscle cells is free in the cytoplasm, which explains its appearance in the blood plasma within 3-6 hours after damage to the heart muscle (this is also facilitated by the small size of troponin molecules). The main amount of troponin-I in the cell is associated with muscle filaments and, when the cardiac cell is damaged, is released slowly, as a result of which the increased concentration of troponin in the blood persists for 1–2 weeks after myocardial damage.
Troponins and myocardial damage
The period of increased troponin-I release thus overlaps the diagnostic windows of both creatine kinase-MB and LDH. Troponin-I concentrations peak between 14 and 20 hours after the onset of chest pain; 7 hours after the development of acute myocardial infarction, the concentration of troponin-I is increased in 95% of patients. After successful thrombolysis, there is a greater increase in troponin-I levels compared to patients with persistent occlusion (washout phenomenon).
It is advisable to study troponin-I when examining patients both early and late after the onset of clinical symptoms. This test is useful in deciding the choice of management tactics for patients with acute coronary syndrome, including patients with unstable angina. In acute coronary syndrome, elevated levels of troponin-I are regarded as a sign of myocardial ischemia, caused by activation and aggregation of platelets and leading to necrosis.
An increase in troponin-I concentrations in patients with unstable angina indicates a poor prognosis and the risk of developing myocardial infarction in the next 4–6 weeks. Determination of troponin-I can be used to diagnose myocardial infarction in patients with concomitant skeletal muscle injury (it has been shown that acute and chronic skeletal muscle injury, excessive physical activity, surgery, excluding cardiac surgery, and muscle injuries do not cause an increase in troponin-I levels ). Small elevations in cardiac troponin-I should be interpreted with caution. Potentially, various pathological conditions resulting in damage to myocardial cells can lead to an increase in the level of cardiac-specific troponin-I. An elevated troponin level in isolation cannot serve as a basis for the diagnosis of myocardial infarction. In rare cases, troponin-I levels may increase in renal failure.
Indications:
- diagnosis of myocardial infarction;
- examination of patients with myocardial infarction and unstable angina for prognostic purposes;
- choice of treatment tactics for patients with acute coronary syndrome;
- monitoring the effect of chemotherapy on the myocardium.
Preparation
It is recommended to donate blood in the morning, between 8 and 11 am. Blood is drawn on an empty stomach, after 8–14 hours of fasting. It is allowed to drink water without gas and sugar. On the eve of the examination, food overload should be avoided.
Interpretation of results
Reference values: <0.16 ng/ml;
Level up:
- myocardial infarction;
- heart injury, heart surgery;
- myocardial damage after percutaneous transluminal coronary angiography, defibrillation and other cardiac manipulations;
- recent unstable angina (slight increase in concentration);
- non-ischemic dilated cardiomyopathy;
- drug intoxication (cytostatics);
- myocarditis;
- heart transplant rejection;
- sepsis and other critical (shock) conditions;
- end-stage renal failure;
- Duchenne-Becker muscular dystrophy;
- DIC syndrome.
Attention! The results of troponin-I determination should be used in conjunction with data from clinical observations and studies of other markers of myocardial damage. Serial testing of troponin-I is recommended to identify the rise and fall of its level characteristic of myocardial infarction.
Burning behind the sternum
Gastritis
Ulcer
Pancreatitis
15070 May 28
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Burning sensation behind the sternum: causes of occurrence, what diseases it occurs with, diagnosis and treatment methods.
Definition
A burning sensation behind the sternum is a symptom characteristic of many diseases - this is how patients with pathologies of the cardiovascular system, spine, gastrointestinal tract, respiratory system, neuralgia and panic attacks describe their sensations.
In some cases, this symptom is not dangerous, but some pathological conditions require immediate medical attention.
Types of burning behind the sternum
There is no generally accepted classification of burning behind the sternum. When patients are asked about their sensations, they talk about pressing, pulling, stabbing, burning, and encircling pain.
Thus, the burning sensation is as varied as the causes that cause it.
Possible causes of burning behind the sternum
Burning in the sternum, a feeling of fullness and heaviness, especially in older people, can be a symptom of serious cardiac problems, and all of them equally require seeking medical help.
In diseases of the gastrointestinal tract, the burning sensation is usually diffuse, often radiating to the back. In many patients it occurs during or after eating.
Disruption of the musculoskeletal system often leads to unpleasant sensations in the chest. The burning sensation intensifies when inhaling or exhaling, and changes when changing body position.
Osteochondrosis of the thoracic spine can cause numbness in the hands and decreased sensitivity.
Neuroses and panic attacks are often accompanied by a burning sensation in the chest.
When the neuroendocrine regulation of internal organs is disrupted, patients complain of a burning sensation behind the sternum. The cause may be either insufficient maturity of the body's systems during adolescence, or previous infectious diseases, stress, bad habits, or overwork. Short-term vasospasm directly leads to the appearance of unpleasant sensations in the heart area. The attacks pass at rest and are accompanied by weakness, rapid heartbeat, and cold hands due to deterioration of blood flow.
Diseases leading to a burning sensation behind the sternum
Cardiovascular pathologies:
- Angina pectoris. Impaired blood circulation in the vessels of the heart due to atherosclerosis leads to deterioration in the nutrition of the heart muscle. During physical activity or anxiety, the heart requires more oxygen - if there is not enough oxygen, then the first signal will be discomfort in the chest area. A burning sensation, a feeling of squeezing, a tingling sensation can radiate (radiate) to the left arm, under the shoulder blade, rarely to the lower jaw, lasting no more than 15 minutes and passing with rest and after taking nitroglycerin.
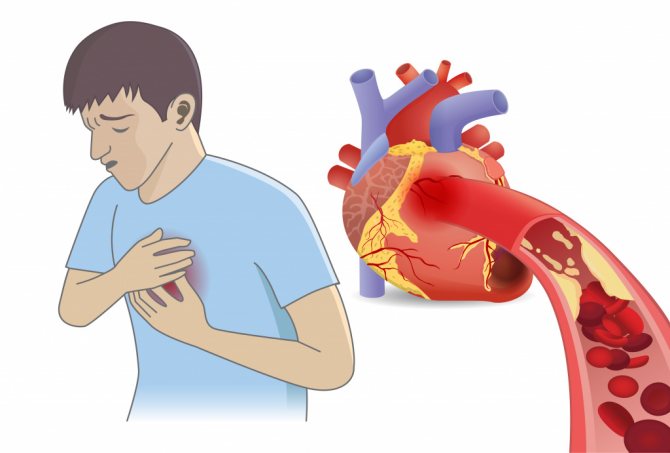
- Myocardial infarction.
During a heart attack, a sharp disruption of the blood supply to the heart muscle occurs due to blockage of most of the lumen of the vessel supplying the heart by thrombotic masses. Most often, intense pain occurs, but a strong burning sensation in the chest may also be present. The attack lasts a long time, is not relieved by nitroglycerin, does not go away with rest, and is accompanied by shortness of breath, severe weakness, and decreased vision. Myocardial infarction is a life-threatening condition, so the patient needs urgent hospitalization. - A sharp rise in blood pressure may occur with a burning sensation in the chest. During a hypertensive crisis, the patient feels weakness, headache, dizziness, nausea, spots appear before the eyes and tinnitus.
- Inflammatory processes in the heart can also be manifested by a burning sensation in the chest. Typically, this condition is preceded by an infectious disease, most often of viral origin, or a severe bruise in the chest area. Unpleasant sensations can spread to the right or left side and intensify with changes in body position.
- A very dangerous condition is pulmonary embolism.
It occurs if blood clots are present in the vessels of the lower extremities - when they break off, they rise up the bloodstream and clog the pulmonary vessels. In addition to a burning sensation behind the sternum, the patient is bothered by severe shortness of breath, coughing (sometimes with blood), and severe cyanosis appears. In such a situation, emergency hospitalization is necessary. At risk are patients with varicose veins, smokers, and patients on the first day after surgery.
Diseases of the gastrointestinal tract:
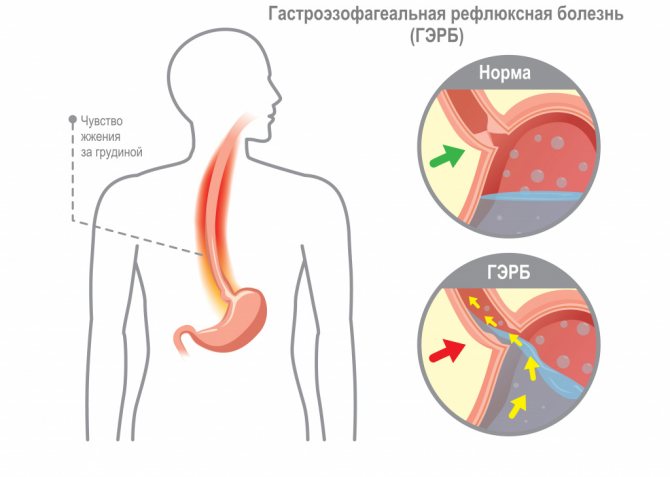
- Esophageal pathology is considered perhaps the most common cause of burning in the chest. It occurs as a result of the reflux of acidic gastric contents into the esophagus, which leads to damage to its mucous membrane. A burning sensation appears after eating food (especially spicy, fatty, smoked and fried), when wearing tight belts and taking a horizontal position immediately after eating.
- Inflammatory processes in the pancreas and gall bladder are often accompanied by a burning sensation in the chest. This symptom appears a couple of hours after eating and may be accompanied by nausea and heaviness in the stomach.
Respiratory diseases:
In case of inflammation of the bronchi or lungs (bronchitis, pneumonia, pleurisy), in addition to coughing and fever, the patient may be bothered by a burning sensation in the chest.
In addition, diseases characterized by a burning sensation behind the sternum include intercostal neuralgia, osteochondrosis, intercostal myositis, and vegetative-vascular dystonia.
Which doctors should I contact if I have a burning sensation in the chest?
If a burning sensation behind the sternum is accompanied by a sharp deterioration in condition, weakness, an increase in pain, shortness of breath, coughing, or dizziness, you must immediately call an ambulance.
In other cases, you should also not postpone your visit to the doctor. Since this symptom has many causes, it is advisable to first turn to. He will prescribe examinations and, if necessary, refer to other specialists: a cardiologist; gastroenterologist; pulmonologist; neurologist.
Diagnosis and examinations for burning sensation behind the sternum
Making a diagnosis begins with a thorough history taking into account all the patient’s complaints and a physical examination.
To exclude cardiovascular pathology, first of all, a chest x-ray or CT scan of the chest and mediastinum is performed, as well as an electrocardiographic study (ECG) or echocardiography (EchoCG).