One of the methods for assessing external respiratory function (RFF) is spirometry (spirography). This study has several objectives:
- Identify existing pathologies
- Monitor the patient's condition
- Assess the effectiveness of treatment
- Teach the patient proper breathing techniques
This study can be carried out for both adults and children. There are some nuances to performing this procedure for children, which we will discuss below.
When should you get diagnosed?
You should undergo a spirometry test if you have the following symptoms:
- Cough, including chronic
- Frequent respiratory diseases
- Attacks of suffocation
- Shortness of breath both during physical exertion and at rest (in the absence of pathologies of the cardiovascular system)
- Chronic rhinitis
- Pain in the chest
It is also necessary to carry out this procedure if:
- You have been smoking for a long time
- At work, you constantly interact with dust or paint materials
- You have bronchial asthma and you need to assess its severity
- It is necessary to establish the degree of ability to work
- Some medical conditions need to be monitored, such as heart failure, if you are taking bronchodilators
- It is necessary to undergo a medical examination before surgery
Methodology
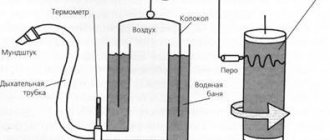
To carry out measurements, a special device is used - a spirometer. Its functional part consists of a mouthpiece, an air tube and a sensor. The device records the volume and speed of air that enters and exits the lungs. All indicators are calculated by a computer, which already contains data on the patient’s age, height, weight and gender. All data is processed by the doctor at the end of the study.
The examination algorithm is as follows:
- You need to sit or stand comfortably
- A special mouthpiece is put on the tube, after which it is placed in the oral cavity
- A special clip is attached to the nose
- The doctor asks the patient to breathe a certain way into the tube
- During the procedure, the spirograph itself analyzes the data and builds graphs
You are asked to breathe several times so that the computer calculates the best value and minimizes the error.
There is a procedure using a bronchodilator (bronchodilator test). It helps to assess the degree of bronchial obstruction, distinguish asthma from COPD, accurately determine the stage of development of the pathology, and evaluate the effectiveness of treatment.
How to prepare for the procedure
- Do not take antihistamines 48 hours before
- No smoking for 2 hours
- Avoid caffeinated drinks and medications 8 hours in advance
- Quit alcoholic beverages a few days in advance
- Avoid physical activity
- Remove lipstick
- Before the procedure, remove your tie and unbutton your collar so that nothing interferes with free breathing.
- No need to worry
Following the recommendations is very important because careful preparation will ensure the most accurate results. The consequence of incorrect implementation of the preparation rules can be a high measurement error and, as a result, poor results.
Preparation for pulmonary function assessment
To obtain a reliable and most accurate result, it is necessary to prepare for the study. The training rules are based on creating conditions for maximum free breathing:
- The assessment is carried out on an empty stomach. It is allowed to eat light food, but no later than two hours before testing;
- Stop smoking 4-6 hours before the respiratory system assessment;
- Avoid drinking alcohol, strong coffee or tea during the day;
- The day before testing, you must avoid physical activity (cancel training, jogging);
- Do not use medications that affect the respiratory system. Be sure to consult a doctor when taking any medications;
- During the study, avoid tight-fitting clothing. Movements must be free;
- Immediately before testing, sit in a quiet environment for at least half an hour.
What indicators are recorded during the research process?
| Abbreviation | Decoding | Description |
| vital capacity | Vital capacity of the lungs | Shows the maximum volume of air that a person is able to inhale after exhaling as deeply as possible. Shows how much air fits in the lungs and participates in the gas exchange process |
| FVC | Forced vital capacity | Shows the maximum volume of air that a person is able to forcefully exhale after taking the deepest breath possible. This indicator indicates the degree of elasticity of lung tissue |
| FEV1 | Forced expiratory volume in the first second | Reflects the speed at which air passes through the bronchi per second |
| POSvyd. and POSvd. | Peak expiratory and inspiratory flow rates | Maximum speed values during inhalation and exhalation |
| FEV1/VC | Tiffno index | Allows you to distinguish obstructive disorders from restrictive ones |
| MOS 25, 50, 75 | Maximum flow rates at 25, 50 and 75% FVC levels | Indicators of the speed of air passage through bronchi of various calibers |
| SOS 25 – 75 | Average forced expiratory flow rate | The average air flow rate during forced expiration, measured during the period when expiration was between 25% and 75% of FVC. These data show the condition of the bronchioles and small bronchi. |
How the research is carried out
The patient's height and weight are recorded. The doctor explains how to breathe and in what order. The spirometer constantly records the amount of air exhaled and inhaled. The patient's nose is pinched and asked to perform several actions.
1. To determine indicators during normal breathing, you need:
- Take a deep breath;
- Hold the breath;
- Exhale evenly and calmly.
2. The actions are repeated, exhaling with effort - the reserve volume of exhalation is obtained for calculating the vital capacity of the lungs.
3. The patient inhales forcefully (to obtain an indicator of forced vital capacity).
Each of these actions is performed several times. The allergist analyzes the information received and draws up a conclusion.
How is spirometry performed for children?
The study of external respiration functions for children is carried out from the age of five. It is not recommended to carry out this examination at an earlier age, since in children the structure of the respiratory system has its own characteristics and there is a high probability of obtaining unreliable data.
Children over 5 years old can undergo practical research like adults, with the exception of some psychological nuances. In order for the child to correctly follow all the doctor’s recommendations during the procedure, various playful approaches are used. The child is asked to blow out the candles on a birthday cake or inflate a large balloon on the monitor screen.
During the entire study, a doctor is with the child, who monitors the correctness of all actions, and then gives a conclusion.
What the study shows
The analysis makes it possible:
- Determine the causes, degree and types of dysfunction of the respiratory system;
- Prescribe a course of treatment measures;
- Assess the effectiveness of treatment;
- To identify the possibility of reversibility of pathology while taking bronchodilators;
- Track the dynamics of changes.
- Spirography is the recording of changes in the amount of inhaled and exhaled air.
- Pneumotachography is a continuous recording of the volume and speed of air flow under different breathing modes. The most indicative is the graph constructed during the formed exhalation.
Pulmonary function testing is the most informative method for diagnosing lung diseases, which includes two main procedures.
The combination of the two methods listed above is called spirometry.
Frequency of procedure
Regardless of age, gender and field of activity, it is recommended to undergo diagnostics of external respiratory function (RFF) at least once a year. Even if you do not notice symptoms of any diseases, this does not mean that the procedure will not be useful. A number of diseases, for example, bronchial asthma or obstructive pulmonary diseases, can develop over time. Therefore, it is better to find out about them at an early stage, when it is possible to cure them quickly.
If you are aware of your health problems, the frequency of this procedure is determined by the attending physician individually in each specific case. General recommendations are as follows:
- If the disease is in remission - at least 2 times a year
- Before prescribing treatment for respiratory function disorders
- 14 days after starting treatment
- Periodically during the course of taking medications to adjust treatment
Are there errors in the results?
The computer program used to determine the results reads and processes the data quickly and without errors. The only thing that can cause inaccurate results is a violation of research methods.
Therefore, it is very important to follow all the doctor’s instructions during the process. If the specialist suspects inaccuracies in the results, he will suggest the patient to undergo the procedure again.
At the AllergoCity clinic, you can undergo an examination of external respiration functions (ERF) using one of the best equipment in Novosibirsk - an expert-class spirograph. The whole process will take a little time, and the results will be analyzed by qualified doctors with extensive experience.
FAQ
Questions related to spirometry are answered by a medical specialist - pulmonologist, functional diagnostics doctor, Candidate of Medical Sciences, assistant of the Department of Pediatrics of the Faculty of Pediatrics and PPV of NSMU Lyubov Vadimovna Stepanova.
- Can I eat before the procedure or do I need to come on an empty stomach?
- Why is spirometry performed only from 5 years of age?
There is no need to come for the procedure on an empty stomach. You eat as usual. The main thing is not to overeat immediately before spirometry. This is because if the stomach is full, it can put pressure on the lungs. In addition, the process of digesting food, in particular its movement through the esophagus, reflexively affects the breathing process, it becomes more frequent. All this can affect the results.
There are two main reasons for this:
- Firstly, the structure of the respiratory system in young children has its own characteristics, so it is difficult to get an accurate result
- Secondly, due to psychological characteristics, children under five years old find it difficult to clearly follow the doctor’s commands and regulate their breathing
Both of these factors can affect the measurement results. Therefore, in order to obtain the most reliable information, we recommend conducting research for children starting from 5 years old.
- Why is a patient’s weight and height measured before the procedure?
- Do I need to bring a bronchodilator with me to my spirometry procedure?
There is no need to bring a bronchodilator with you. The functional diagnostics doctor individually uses a bronchodilator drug available in the clinic. At the same time, he focuses on the patient’s complaints or diagnosis
Data on weight and height are entered into a computer program, which uses special formulas to calculate the norms of external respiration function. All data that we receive from the examination results is calculated individually for each patient, taking into account his parameters.
Research: spirography and spirometry
This information cannot be used for self-medication! Consultation with a specialist is required!
What is spirometry?
Spirometry is a research method that allows you to assess the function of external respiration and includes the measurement of volume and velocity indicators. Using spirometry, the following indicators are usually measured: respiratory rate, tidal volume, vital capacity, forced expiratory volume, etc.
The term “spirography” refers to the graphical recording of measurements taken.
How is spirometry performed?
Spirometry is now usually carried out using a computer spirometer, which converts the sensor readings into digital format and automatically makes all the necessary calculations.
The subject's nose is pinched with a special clamp. He has to breathe exclusively through his mouth through a special mouthpiece.
The procedure begins by measuring breathing characteristics at rest. Next, breathing is studied during forced exhalation. The patient then breathes very quickly and deeply to test the maximum possible ventilation of the lungs.
Often at the end of the study, functional tests are performed, for example, a test with drugs that dilate the bronchi.
A repeat study is carried out 3-5 minutes after their use. If external respiration parameters improve or are restored completely, they speak of reversible bronchospasm.
Another functional test is called provocative. The patient is inhaled with histamine, which can lead to bronchospasm and thereby confirm or refute the diagnosis of bronchial asthma.
Where is spirometry performed?
This examination can be completed on an outpatient basis.
Spirometry is carried out by a nurse or a functional diagnostics doctor in a clinic, diagnostic center or any other medical institution that has a spirograph.
What diseases does spirometry detect?
Spirometry reveals diseases that are accompanied by bronchial obstruction (impaired patency of the bronchial tree), namely: bronchial asthma, chronic obstructive pulmonary disease, bronchiectasis.
Deviations from the norm of the indicators obtained as a result of the examination make it possible to judge the absence or presence of a respiratory system disease in a person, the degree of its severity and the reversibility of the condition.
Who needs spirometry?
Patients with bronchial asthma, obstructive bronchitis, bronchiectasis, and long-term smokers need to undergo spirometry. The study is recommended not only to identify these diseases, but also to evaluate the effectiveness of treatment.
Preparing for the study
The study should be carried out strictly on an empty stomach, it is advisable not to drink a lot of liquid.
You should refrain from smoking. If the patient uses inhalers, he should inform the doctor about it. The method is absolutely painless and does not cause any discomfort.
Contraindications to the procedure
There are no absolute contraindications to spirometry.