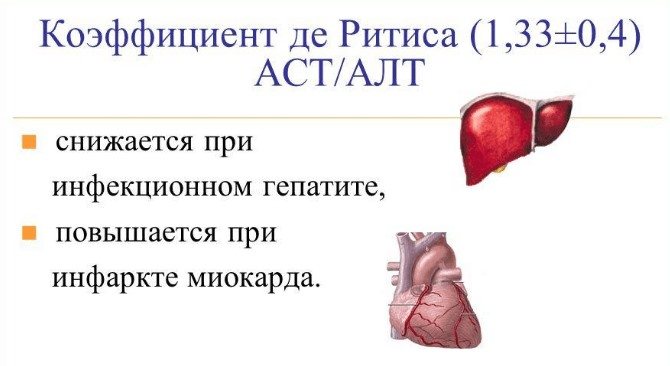
The de Ritis coefficient was discovered by an Italian scientist, after whom it was named. He determined that an important indicator of the state of the human body is not only the level of aspartaminotransferase (AST) and alanine aminotransferase (ALT) in the blood separately, but also their ratio. It was called the de Ritis coefficient.
What is the de Ritis ratio?
The coefficient is important in diagnosing liver and kidney pathologies
The coefficient is the ratio of AST and ALT. This indicator is determined if there are deviations from the norm in one or two of its components. It is important for diagnosing a number of pathologies.
This is due to the organ-specific nature of the enzymes, which means they are related to the proper functioning of the liver, heart, pancreas and, to some extent, the kidneys.
If a deviation from the norm is detected, a full examination is required to determine what pathology is occurring.
Ratio norms
For the indicator, the normal limits are determined, within which it is found in the absence of pathologies in a person. This value ranges from 1 to 1.75 U/l, regardless of the age and gender of the patient.
When AST increases in the body, the coefficient also increases. If the volume of ALT increases, then the coefficient decreases. This feature allows you to more accurately and efficiently diagnose liver and kidney diseases.
Thus, it is known that with a de Ritis index of less than 1, the patient is most likely to have chronic liver pathologies, and with a value of 2 or more and an increased volume of albumin, severe liver disorders are most likely.
A value of 2 with normal albumin indicates heart disease and primarily myocardial infarction.
How is the de Ritis coefficient calculated?

The coefficient is the result of calculating indicators
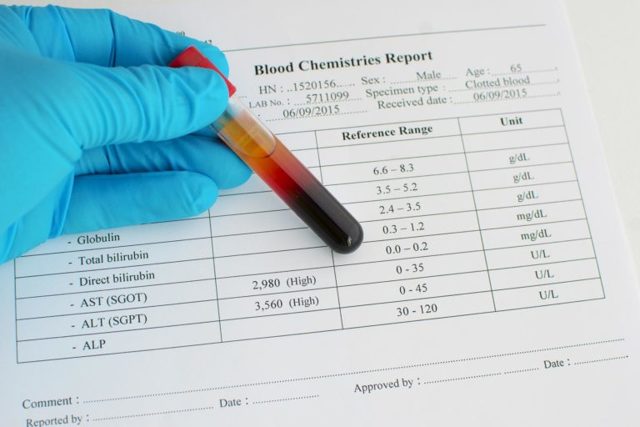
The indicator is calculated using a formula. For its use in blood biochemistry, AST and ALT indicators are determined. Next, the AST level is divided by the ALT level. The resulting number will be an indicator of the de Ritis coefficient. The coefficient is determined only if the patient’s blood test shows a deviation from the norm in AST and ALT.
If they are normal (neither increased nor decreased), then their ratio is not of interest.
The role of the coefficient in the diagnosis of liver diseases
When diagnosing liver diseases and monitoring the effectiveness of therapy, the coefficient is of great importance. The activity of the ALT enzyme in blood serum during hepatitis increases significantly - up to 8-10 times. At the same time, the AST indicator rises only 2-4 times.
In this case, the de Ritis coefficient drops to 0.6. If the decrease in value turns out to be even greater, then this is regarded as an unfavorable indicator of the development of the disease.
In the event of necrotic changes in the liver tissue, the coefficient increases due to the fact that AST and ALT are released into the blood in increased quantities.
What analysis allows you to calculate the coefficient

To calculate the coefficient, a biochemical study is required
To identify the de Ritis coefficient, it is necessary to identify the AST and ALT indicators. To do this, a biochemical blood test is carried out, during which its other parameters are also determined.
Such an analysis most fully shows the general condition of the body, allowing one to assess the correct functioning of most systems and organs.
The values of only aspartaminotransferase and alanine aminotransferase are rarely determined, since in diseases for diagnostic purposes it is important to obtain a complete blood picture.
There are no differences in the study for children and adults. It requires venous blood, which is donated on an empty stomach. Afterwards, in the laboratory, it is placed in a centrifuge and serum is obtained, in which enzymes are determined.
Indications and preparation for analysis

Pathology of the gastrointestinal tract - indication for analysis
Indications for a blood test, which will determine the coefficient, are conditions that cause changes in the levels of AST and ALT. These are the following diseases:
- hepatitis of various nature;
- malignant neoplasms of the liver, primary or secondary;
- liver cirrhosis and suspicions of its presence;
- pancreatitis;
- severe poisoning that can lead to liver damage;
- infectious form of mononucleosis;
- myocardial infarction.
Also, a biochemical blood test is performed during routine examinations in pregnant women. In this case, the coefficient is determined only if there are deviations in AST and ALT.

Preparation is required for reliable results.
To obtain reliable analysis results, proper preparation is required. Its basic rules are:
- avoiding fatty and spicy foods 3 days before donating blood;
- abstinence from alcohol 2 days before donating blood;
- the fasting period before collecting material is 12 hours;
- drink water for the last time before the study no later than 4 hours;
- reducing stress and physical activity on the eve of the analysis.
If you are taking medications, you must inform your doctor about this. If necessary, he will inform you how long before donating blood you need to refuse them.
Decoding the analysis results

The test results are interpreted by the doctor
The result of the study is deciphered by the doctor who gave the referral. At the same time, the data cannot be independently regarded as the final diagnosis, since a complete examination of the patient is necessary to determine the pathology that caused the violation of the de Ritis coefficient.
When is an examination necessary?
These enzymes are determined during a biochemical blood test, among other parameters that can indicate the presence of pathological processes in the relevant organs. It is also important to evaluate blood components such as bilirubin and GGT - gamma-glutamyl transpeptidase, an enzyme whose activity increases in liver diseases and alcoholism.
Both venous and capillary biomaterial can be taken for research. The research method is a unified kinetic test. To obtain the most reliable picture of blood composition, the patient must follow several rules, including:
- reduction in physical activity the day before blood sampling;
- refusal to eat for 12 hours before the procedure;
- abstain from smoking for at least 30 minutes before submitting the biomaterial.
An analysis to study the level of transaminase in the blood is prescribed in the presence of certain symptoms characterizing a functional liver disorder, namely:
- yellowness of the skin and mucous membranes;
- decreased or lack of appetite;
- pain in the epigastrium;
- causeless bloating;
- change in color of stool;
- nausea, vomiting, itching;
- darkening of urine;
- general weakness.
In addition to pronounced signs of the disease, biochemistry analysis is carried out in a fairly significant number of situations, such as:
What does alkaline phosphatase show in a blood test?
- hereditary predisposition to liver diseases;
- taking medications that can harm the liver;
- alcohol abuse;
- ambiguous diagnosis of hepatitis;
- condition after hepatitis;
- obesity, diabetes mellitus;
- assessment of the effectiveness of therapy for hepatitis, cirrhosis, etc.
To establish an accurate diagnosis, it is necessary not only to determine the enzymes of the transaminase group, but also to compare them with other analysis indicators, which also undergo changes to one degree or another. AST values in the blood, in addition to the above additional indicators, are often assessed in parallel with the results of examinations for alkaline phosphatase and total protein.
This comparison helps determine the specific form of liver pathology. It is equally important to determine the level of aspartate aminotransferase when taking potentially toxic drugs for the liver, which is why, if the enzyme level is elevated during therapy, the patient may be transferred to another drug.
The ratio of ALT and AST: the norm of analysis indicators
ALT (alanine aminotransferase, Alt) and AST (aspartate aminotransferase, Ast) are marker enzymes that are found in the cells of various organs and enter the blood only when they are destroyed.
The levels of these transferases also increase during pregnancy, with liver pathology, after a course of certain medications or after physical exercise.

The level of Alt and Ast transferases in the blood is determined by biochemical analysis, which is considered the most informative for identifying liver diseases at the initial stage. This is due to the fact that at the initial stage, liver diseases develop painlessly.
The liver does not hurt because it has no nerve endings. Pain in the right hypochondrium, after which a person usually goes to the doctor for the first time, is caused by pathologies of the gallbladder.
Therefore, only regular donation of blood biochemistry makes it possible to identify liver pathologies at a stage before they have reached the point of irreversibility.
Norms of ALT and AST in the blood (tables by age)
Among women
Normal levels of ALT and AST in the blood of women:
- for ALT - from 0 to 35 U/l;
- for AST - from 0 to 31 U/l.
Alt and Ast are normal in the blood of women by age - table:
| Age | ALT | AST |
| newborns | 48 | 25-75 |
| 4-6 months | 55 | 15-60 |
| 3 years | 32 | 15-60 |
| 6 years | 28 | 15-60 |
| 11 years | 38 | 15-60 |
| from 18 | up to 35 | up to 31 |

With age, the level of transferases in women gradually decreases. For example, the upper limit of ALT in healthy women after 50 reaches 28 U/l, and by old age it varies from 5 to 24 U/l.
There are some factors that can affect the transferases of a healthy woman, causing them to fluctuate within 30%. These are the factors:
- 1st trimester of pregnancy;
- excess body mass index;
- alcohol and drug use;
- taking certain medications;
- physical activity, overwork, lack of sleep;
- stress, emotional arousal.
In men
Due to the fact that the percentage of muscle mass in men is higher than in women, then, accordingly, the proportion of ALT and AST enzymes entering the circulatory system in a man who does not suffer from any pathologies will be slightly higher.
Hepatitis C virus RNA: quantitative and qualitative analysis
Approximate norms of ALT and AST in the blood of men, which are guided by when decoding tests:
| Age | AST (units/l) | ALT (units/l) |
| less than a year | up to 58 | up to 56 |
| 1-60 years | up to 40 | 10-40 |
| 60-90 years | up to 40 | 13-40 |

In men over 90 years of age, ALT levels gradually decrease.
Reasons for increased blood levels of ALT and AST
Isolated increase in ALT
ALT is increased when released from destructively altered cells. Typically, an increase in ALT is caused by:
- liver diseases - viral and alcoholic hepatitis, fatty hepatosis, cirrhosis, cancer;
- heart disease - minor myocarditis, and other diseases that occur with the destruction of myocardial cells;
- severe poisoning and extensive burns, as well as injuries with damage to muscle tissue;
- acute pancreatitis;
- autoimmune thyroiditis;
- intrahepatic cholestasis:
- myositis.
What can you find out when determining the level of aspartate aminotransferase in the blood?
If AST in the blood is slightly increased (about 5 times), then this may be due to fatty hepatosis, taking certain medications (barbiturates, statins, antibiotics, drugs, chemotherapy drugs, etc.).
A moderate, average increase in the enzyme (up to ten times higher than normal) can be caused by chronic liver diseases, cirrhosis, myocardial infarction, myocardiostrophy, processes occurring with damage to kidney and lung cells, mononucleosis, cancer.
If AST in the blood is greatly increased (10 times or more), this tells the doctor that the patient may have viral hepatitis in the acute stage, toxic damage to the liver structures, drug-induced hepatitis (acute), and this may also indicate a disease in the body processes accompanied by tissue necrosis (for example, with tumors).

At the beginning of the disease, in its acute stage, when the process of tissue destruction is fastest, the highest level of aspartate aminotransferase is observed. A decrease in AST in the blood serum means the beginning of restoration processes in organ cells and the patient’s recovery. Slight excesses of the norm are not a sign of tissue destruction.
De Ritis coefficient: Indications for Prescription, Norms
Timely diagnosis is the key to successful treatment. At the moment, there are many types of research, including laboratory research. It is noteworthy that it is with the tests that the patient’s path to identifying pathology begins.
At the moment, there are a number of biochemical blood tests that can identify existing abnormalities and set further direction for effective treatment. This includes the determination of the quantitative composition and ratio of the enzymes AST and ALT.
In medicine, this analysis is referred to as the de Ritis coefficient. And it is named after the Italian scientist Fernando de Ritis, who introduced it into medical practice, proving its extensive diagnostic significance.

Blood test - de Ritis coefficient
Enzymes AST and ALT: what is their functional role in the body
Before we begin to understand these two concepts, let's decipher their abbreviation. ALT is ALanine aminotransferase, AST is ASpartate aminotransferase. These enzymes take part in the metabolism of carbohydrates and amino acids. They accelerate intracellular reactions, and vitamin B6, a coenzyme of pyrodoxine, helps them in their catalytic activity.
Their work is contained in every living cell. Natural cell death involves the release of a small amount of its contents into the hemorrhagic fluid.
Massive cell death leads to a significant appearance of intracellular enzymes in the blood and, accordingly, a high level of their levels. This will indicate the presence of some pathological process that leads to cellular destruction and tissue necrosis.

ALT
ALT is found in many human tissues and organs. It can be found in the heart muscle, spleen, pancreas, lungs, kidneys, skeletal muscles, liver, etc.
Moreover, in the latter case, the concentration of its content qualifies as the highest, which is why ALT is often called the liver enzyme. Alanine aminotransferase is involved in amino acid metabolism. It is a kind of catalyst for the transfer of alanine from an amino acid, resulting in the production of pyruvic and glutamic acid.
The need for alanine in body tissues is expressed in the rapid conversion of this amino acid into glucose. And, as we know, glucose is the energy that powers the central nervous system and the brain. In addition, one of the functions of alanine is considered to be participation in the synthesis of lymphocytes, strengthening the immune system and the regulatory ability in the metabolism of sugars and acids.
AST
Aspartate aminotransferase is found to a greater extent in the myocardium, liver tissue, muscles, and neurons.
This is explained by the high need to maintain metabolic processes there and the ability to maintain cellular structure at a normal level.
Like ALT, this enzyme is involved in the daily synthesis and metabolism of amino acids, and, in particular, in the breakdown of aspartic amino acid.
Based on the above, we can conclude that ALT indicators are more important in the diagnosis of acute liver conditions, and AST will indicate the destruction of the heart muscle - myocardium or liver.
What is AST
Aspartate aminotransferase, or AST for short, is the name of an enzyme that is part of absolutely all cellular structures of our body. But the largest amount of aspartate aminotransferase is found in the myocardium and skeletal muscles, then in liver cells, in nervous tissue, and in the kidneys. If the body is normal, then the levels of AST activity in the blood are quite low.

But when various organs or systems of the body are damaged, the enzyme begins to be released and enter the bloodstream. Thus, with a biochemical analysis, it becomes clear that AST in the blood is increased - this gives the doctor reason to suspect the beginning of destructive processes in the cells. The enzyme aspartate aminotransferase is necessary for proper cell function. It performs transport functions, delivering groups of atoms to various amino acids.
ALT and AST indicators in blood biochemistry | University Clinic
When a patient receives a referral for a blood test from a vein, in most cases it contains two abbreviations ALT (AlaT) and AST (AST). Why are these indicators so important for making a correct diagnosis?
What do ALT and AST have in common and in what cases are their concentrations determined?
These substances - alanine aminotransferase (AlAt) and aspartate aminotransferase (ASAT) - belong to the group of transaminases - enzymes found in the liver, heart, muscles and some other organs. Both enzymes take an active part in protein, carbohydrate and energy metabolism, i.e. necessary to maintain basic body functions.
Normally, transaminases are found in organ cells, practically not entering the bloodstream. But if cells die, they end up in the bloodstream, and their concentration in the body increases. Therefore, these substances are called damage markers.
By the amount of these substances one can judge the degree of the pathological process. The more severe the disease, the higher the level of transaminases. For example, with myocardial infarction or severe hepatitis, the levels of these substances can increase 20-40 times or more.
A decrease in transaminase level indicates subsidence of the disease and correctly chosen treatment, an increase indicates a worsening of the disease. Therefore, biochemistry is taken several times during the treatment process.
What is the difference between AlAt and AsAt
Despite the great similarities, these two substances also have significant differences:
- The bulk of alanine aminotransferase is located in liver cells. The heart, kidneys, pancreas, and skeletal muscles contain less of it. Therefore, an increase in the level of this substance most often indicates the death of liver cells - hepatocytes.
- The test allows you to diagnose hepatitis before the appearance of jaundice. Moreover, using an analysis for alanine aminotransferase, it is possible to identify anicteric, erased, latent forms of the disease. An increase in transaminase is also observed in cirrhosis and organ cancer.
Main indications for determining AlAt:
- Signs of liver damage are heaviness on the right side under the ribs, yellowing of the skin and corneas of the eyes, itching of the skin, the appearance of light-colored feces and dark urine.
- Changes in liver ultrasound, included in the abdominal ultrasound complex, indicating liver pathologies.
- Positive test results for hepatitis.
- Taking medications that have a negative effect on organ cells.
To obtain a large amount of information about the state of liver function, determination of ALT concentration is prescribed in conjunction with a biochemical study of other indicators.
ACaT is concentrated mainly in the heart - there is less of it in other organs. Therefore, the level of this transaminase increases with myocardial infarction, angina pectoris, and heart failure. In liver disease, the enzyme level is less elevated.
Aspartate aminotransferase concentrations increase when skeletal muscle is damaged by trauma. Its content is also increased during inflammatory processes in the muscles (myositis) and genetic diseases manifested by muscle weakness (myopathy).
The main indications for prescribing biochemistry for AST:
- Pain in the heart and behind the sternum.
- Heart attacks accompanied by shortness of breath and increased heart rate.
- Pain in the heart area that has arisen after a recent sore throat or scarlet fever. This condition indicates the possible development of cardiac rheumatism.
- Muscle weakness, unsteadiness of gait, pain in the limbs.
- Trauma with extensive muscle damage.
An aspartate aminotransferase test is prescribed for patients who have undergone surgery on the heart and coronary vessels. A decrease in transaminase concentration indicates a healing process and gives a good prognosis.
De Ritis coefficient - how to calculate a diseased organ
To determine which organ is associated with an increase in transaminase levels, you need to calculate the de Ritis coefficient - the ratio of AlAt and AsAt, which is normally equal to AST/ALT = 1.3 ± 0.4. With heart damage, the coefficient increases, and with liver disease, it decreases.
However, the correct ratio of indicators does not mean the absence of diseases. Other biochemical indicators are also important to determine the condition of the liver and heart:
- Gamma-glutamyl transpeptidase (GGTP) and alkaline phosphatase (ALP) are markers of cholestasis - stagnation of bile in the hepatic ducts. An increase in these enzymes with an AST/ALT ratio>2 indicates alcohol abuse.
- An increase in the concentration of GGTP and alkaline phosphatase with a high level of ALT is observed with biliary dyskinesia and other pathologies that impede the outflow of bile.
- A significant excess of ALT, leading to a decrease in the De Ritis coefficient, in combination with a high level of the liver enzyme bilirubin, is an unfavorable sign indicating severe liver disease.
In heart disease, the concentration of aspartate aminotransferase increases, so the De Ritis coefficient increases. To clarify the nature of cardiac pathology, patients are tested for other indicators:
- Lipid profile - an analysis of cholesterol, lipoproteins and triglycerides, showing the likelihood of atherosclerosis, leading to angina and heart attacks.
- Creatine kinase (CPK) is another enzyme whose elevated fractions indicate myocardial damage.
- Lactate dehydrogenase (LDH) is a substance whose concentration increases several hours after myocardial infarction.
An increase in AlAt and AsAt, combined with a significant excess in CPK, is characteristic of muscle pathologies. In these diseases, the level of creatine kinase can be increased tenfold.
Isolated determination of alanine aminotransferase or aspartate aminotransferase is not very informative. Such an analysis can be recommended as a preventive diagnostic to make sure that everything is fine in the body.
In case of liver and heart diseases, it is more advisable to donate blood for biochemistry with the determination of a large number of indicators. Such an examination allows not only to assess the condition of the organs, but also to make a diagnosis.
What can distort the analysis results
Sometimes a doctor, seeing that AST in the blood is elevated, but not finding any visible signs of illness in the patient, recommends that he donate blood again, and this additional test shows normal levels of the enzyme. Upon detailed questioning, it turns out that the patient was taking medications on the eve of the first blood donation, which affected the correctness of the indicators. To avoid such situations, you need to know what can distort the result:
- Taking certain pharmaceuticals. It is important to inform your doctor about all medications you are taking. The doctor may prohibit taking certain medications a few days before donating blood.
- Use of herbal remedies: echinacea or valerian.
- Intake of large doses of vitamin A into the body.
- Pregnancy.
- Severe allergy.
- Catheterization or recent heart surgery.

If AST in the blood is elevated, the reasons may be different, sometimes even unexpected. In order not to worry unnecessarily because of incorrect results, it is not recommended to donate blood for testing for several hours after undergoing the following procedures:
- fluorography;
- rectal examination;
- Ultrasound;
- physiotherapy;
- radiography.
De Ritis coefficient as an indicator of enzyme levels: how to calculate it and determine the disease
Early diagnosis of any disease is the key to successful treatment. However, trying to identify all possible diseases in oneself, a person will stop leaving medical offices and research laboratories, eventually earning a nervous breakdown.
There are a number of biochemical blood tests that can detect abnormalities in the body and set the direction for further examination.
These include the determination in the blood of the quantitative composition of the enzymes ALT, AST and their ratio, called the de Ritis coefficient.
It was named in honor of the Italian scientist who showed its diagnostic significance in blood tests and introduced it into widespread medical practice.
De Ritis coefficient
How to calculate?
In order to calculate the de Ritis coefficient, it is necessary to know the concentrations of AST and ALT. The measurement of these values is included in the blood chemistry results. Screening is carried out in the laboratory with blood taken from the antecubital vein. To obtain the correct concentration of enzymes, you must adhere to the following rules:
- Avoid shocks to the body that threaten the functioning of the nervous system.
- Do not smoke at least 2 hours before donating blood.
- Blood collection must be done on an empty stomach.
- Do not drink alcohol-containing drinks at least 7 days before the test.
The ALT and AST results help determine whether a ratio needs to be calculated. When the levels of these substances in a person’s blood do not deviate from the norm, it is not advisable to calculate the de Ritis coefficient. Enzyme concentration standards:
The analysis is carried out if liver disease is suspected.
Due to the fact that AST and ALT are produced by the building blocks of the liver and heart, respectively, the coefficient is used when there is a risk of damage to these two organs. Indications for calculating the ratio:
- cirrhosis of the liver;
- viral, chronic hepatitis;
- pancreatitis;
- liver cancer;
- alcohol poisoning;
- myocardial infarction;
- pregnancy;
- poisoning with mercury and other metals;
- drug overdose;
- jaundice;
- Infectious mononucleosis.
The above diseases occur with a number of pronounced symptoms:
- darkening or lightening of urine/stool;
- yellowness of the skin, sclera of the eyes;
- deterioration in performance;
- nausea;
- vomit.
Preparing for the test
The result of any biochemical test, including a blood test for AST and ALT, largely depends on how to prepare for it.
Rules that will help you avoid false research results:
- Tests must be taken strictly on an empty stomach, at least after an 8-hour fast. You can drink clean water in any quantity. It is recommended to exclude coffee, carbonated drinks, juices and teas during the preparation period. As for alcoholic beverages, it is not recommended to consume them a week before blood sampling for AST and ALT.
- For 3 days, eliminate foods rich in animal fats from your diet. Eat food that is steamed, baked or boiled. Fried foods must be strictly limited, or better yet, completely excluded.
- Three days before the expected analysis, you need to stop intense physical activity.
- Blood sampling should be carried out in the morning, from 7 to 11 am.
- If you are taking medications, it is advisable to stop them 3 days before the test. But before doing this, it is important to consult a doctor.
- Try to get tested in the same laboratory.
- Once you receive the result, be sure to contact your doctor to correctly interpret the results and, if necessary, continue the examination.
Why is bilirubin elevated when transaminases are normal?
If total bilirubin in the blood exceeds the normal value, it is necessary to determine its direct and indirect components. This examination and the readings of other liver tests will help identify the causes of the disease.
An increased level of indirect (free) pigment indicates that the liver is unable to remove it. At the same time, normal values of the direct fraction, ALT and AST are noted. This indicates the rapid destruction of red blood cells, characteristic of such pathologies:
- infectious diseases (malaria, typhoid fever);
- hemolytic anemia (congenital, toxic, autoimmune);
- internal extensive hematomas;
- vitamin B12 deficiency.
Such conditions are characterized by general weakness, pale skin, dizziness, pain in the left side due to an enlarged spleen, tachycardia
An increase in the amount of indirect bilirubin in the blood with a slightly increased or normal level of direct bilirubin indicates a decrease in the level of enzymes in the liver that transform free pigment into bound pigment. Characteristic features:
- heaviness in the right hypochondrium;
- a feeling of bitterness in the mouth, especially after eating fatty, fried, spicy foods;
- white feces, urine the color of strong tea;
- fatigue, weakness.
With stagnation of bile in the liver, the formation of stones in the biliary tract, a high level of direct liver pigment is detected. Blood values of free pigment, ALT and AST are normal or slightly elevated. This condition is manifested primarily by jaundice, but it is also characterized by other symptoms:
- pain in the liver area, possible hepatic colic;
- stool disorders;
- darkening of urine;
- light or completely white feces;
- skin itching;
- hypovitaminosis;
- general weakness.

In the third trimester, due to the enlargement of the uterus and hormonal changes, stagnation of bile in the liver is observed. The woman suffers from unbearable skin itching, digestion is disrupted, and the color of urine and feces changes. Although this condition goes away after childbirth, if left untreated it has a detrimental effect on the fetus.
Reasons for increased ALT
An increase in ALT levels may be due to:
- myositis;
- intrahepatic cholestasis;
- burns, severe intoxication, muscle injuries;
- autoimmune thyroiditis;
- liver pathologies (hepatitis caused by viruses and alcohol, fatty hepatosis, cancer, cirrhosis);
- heart diseases (myocarditis and other pathologies that are accompanied by damage to myocardial cells);
- acute pancreatitis.
Also, the amount of ALT can be increased in cancer, progressive leukemia and obesity of III-IV degree. During a heart attack, this indicator practically does not change.
Indications
- Symptoms characteristic of liver diseases: fatigue, weakness;
- dyspeptic symptoms: loss of appetite, nausea, vomiting, abdominal pain, bloating;
- heaviness and/or pain in the right hypochondrium;
- yellowness of the skin and mucous membranes, sclera;
- discoloration of feces, darkening of urine;
- itching and dry skin;
Mandatory examination of the following categories of citizens:
- donors;
- those who have had hepatitis or have been in contact with the source of infection;
- alcohol abusers;
- suffering from diabetes and/or obesity;
- having a genetic predisposition to the disease.
Objectives of the study
- Diagnostics of damage to cells of the liver, heart and other parenchymal organs (together with ALT);
- Differential diagnosis of myocardial infarction and other diseases of the heart muscle;
- Determining the specific form of liver disease by conducting additional studies: bilirubin, alkaline phosphatase, total protein;
- Monitoring the effectiveness of the current course of treatment;
- Monitoring the health status of patients receiving treatment with hepatotoxic drugs (statins, barbiturates).
The results of a biochemical blood test are interpreted by specialists:
- narrow (cardiologist, gastroenterologist, hepatologist, hematologist, surgeon)
- general practitioner (therapist, pediatrician, general practitioner).
Preparation
Preparatory activities for the study are fully consistent with the preparation program for a standard biochemical blood test. You can see more details here.