Bundle branch block - what is it, why is this condition dangerous?
Bundle branch block is characterized by incomplete or complete blocking of one or two branches simultaneously. The latter is a complete block of the bundle branch, the first is partial.
This conduction disorder is intermittent or permanent. The bundle of His consists of the left and right bundle branches. The first is divided into 2 branches: posterior and anterior. Impulses pass through them to the ventricles, after which the latter contract. Any blocking of excitation impulses leads to the development of various types of arrhythmia.
RBBB is not a separate independent disease, but a consequence and electrocardiological manifestation of the underlying cardiac pathology. In patients with age, the detection rate of this disorder increases.
Reasons for the blockade
Bundle branch block can be caused by various reasons.
| Right bundle branch block | occurs in diseases accompanied by overload and hypertrophy of the right ventricle - mitral stenosis, atrial septal defect, tricuspid valve insufficiency, coronary artery disease, cor pulmonale, arterial hypertension, acute myocardial infarction (posterior phrenic or apical), etc. |
| Left bundle branch block | include atherosclerotic cardiosclerosis, aortic valve defects, cardiomyopathy, myocardial infarction, myocarditis, bacterial endocarditis, myocardial dystrophy. Less commonly, bundle branch block develops against the background of pulmonary embolism, hyperkalemia and intoxication with cardiac glycosides. |
The causes of double-bundle blocks are usually aortic defects (aortic insufficiency, aortic stenosis) and coarctation of the aorta.
Causes
Diseases such as:
- congenital and acquired heart defects - stenosis of the aortic and mitral valves, pulmonary artery stenosis, stenosis and coarctation of the aortic mouth, aortic valve insufficiency, atrial septal defect;
- cardiomyopathy, myocardial dystrophy of various origins - endocrine (thyrotoxicosis, diabetes mellitus), metabolic (anemia), nutritional (alcoholism, obesity), autoimmune (systemic lupus erythematosus, rheumatoid arthritis);
- cardiac ischemia;
- cardiosclerosis, as the outcome of many cardiac diseases, leads to the replacement of part of the muscle fibers with scar tissue, including atypical muscle fibers;
- myocarditis of viral or bacterial origin;
- heart damage due to rheumatism - endocarditis, myocarditis;
- myocardial infarction;
- long-term arterial hypertension, leading to myocardial hypertrophy;
- intoxication with cardiac glycosides;
- pulmonary embolism;
- chronic lung diseases (chronic obstructive bronchitis, pulmonary emphysema, severe bronchial asthma), leading to the formation of cor pulmonale - stagnation of blood in the right atrium and ventricle with their hypertrophy and expansion.
In young children and adolescents, incomplete single-fascicle right blockade may accompany minor anomalies in cardiac development, and in the absence of organic heart damage is considered a normal variant. One- or two-fascicular left blockade is almost always associated with acquired rather than congenital heart diseases and cannot be regarded as a normal variant.
Classification
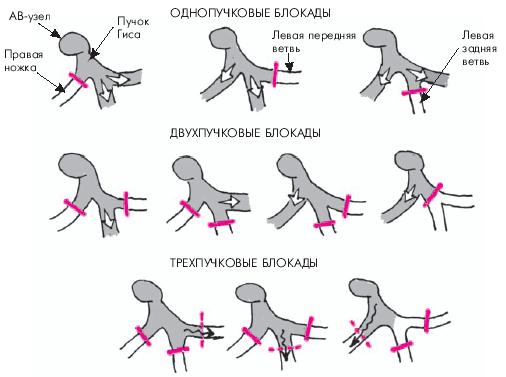
Depending on the number of elements of the His bundle, in which a violation of the impulse conduction is observed, the blockade occurs:
Single-bundle, when impulse conduction through one element of the His bundle is impaired with blockade:
- right bundle branch;
- anterior branch of the left bundle branch;
- posterior branch of the left bundle branch.
Double-bundle, when the conduction of cardiac impulses along two elements of the His bundle is impaired with blockade:
- anterior and posterior branches of the left bundle branch;
- right leg and anterior branch of the left bundle branch;
- the right bundle and the posterior branch of the left bundle branch.
- Three-bundle with blockade along all elements of the His bundle.
The blockade can be complete or incomplete, constant or intermittent (appears and disappears when recording one ECG), transient (not recorded in the ECG), or alternating (when different legs are blocked when recording one ECG).
1.General information
The His bundle, as well as blocks of its structural elements, are very often mentioned by cardiologists, especially when interpreting jagged ECG curves. Of course, it would take many years of study of anatomy, neurology, histology, electrochemistry and other complex sciences to thoroughly understand the structure of this intracardiac formation and the features of this or that blockade. However, it is possible and necessary to get a general idea.
If we use standard comparisons of the heart with a “motor” and a “pump,” then this motor is electric (at least with electrical control, since it is the electrical impulses that cause different groups of myocardial muscle fibers to contract in turn).
The clock frequency and sequence of phases (contraction-relaxation, depolarization-repolarization) in each cycle must be strictly observed, and any desynchronization is fraught with an emergency stop - and clinical death. Therefore, the critical pacemaker function, i.e. setting the step and rhythm is carried out with multi-stage security for uninterrupted operation. If the main “clock generator” (sinoatrial node, Kis-Flyak sinus node) fails, its role is taken over by the hierarchically located lower atrioventricular node (atrioventricular), which, in turn, gives rise to a switching “harness” consisting of the same atypical electrically conductive cells and branching into two parts.
In case of failure, even at this level, the individual terminal fibers of this cord (Purkinje fibers) try to take on the pacemaker role - in a word, the conduction system of the heart is built by evolution with the expectation of maximum automatism. And yet, mortality from sudden arrhythmias and fibrillations (chaotic, uncoordinated contractions of myocardial elements) remains very high.
The bundle of His is the same “multi-core cable” that comes out of the atrioventricular node, is located in the interventricular septum and conducts control electrical impulses to the ventricles of the myocardium.
One of its legs, the back one, continues the “main vein” and goes down; the other two legs, right and left, represent a paired branching. However, they are located and arranged much less symmetrically than other paired structures of the body (eyes, kidneys, lungs, etc.). Thus, the right bundle branch is a complete “power line” going to the muscle fibers of the right ventricle, and the left bundle is further divided into anterior and posterior branches. A blockade is a decrease or absence of electrical conductivity in one or more segments of this conductive network. This blockage can occur:
- in the anterior branch of the left bundle branch;
- in the posterior branch of the left bundle branch;
- in one of the above branches plus the right leg;
- in both branches of the left leg (complete blockade of the left bundle branch);
- in the right leg in the absence of other blockades;
- in all of the listed legs and branches simultaneously (atrioventricular block).
A must read! Help with treatment and hospitalization!
Symptoms
Right bundle branch block is asymptomatic and is an incidental finding detected based on the results of an ECG study during a routine medical examination, medical examination or treatment for other diseases. Single-bundle (anterior or posterior) left blockades also do not have clinically significant manifestations.
Left bundle branch block has symptoms of the disease that caused it, most often these are:
- decreased exercise tolerance;
- shortness of breath with slight physical exertion;
- interruptions in heart function;
- palpitations;
- pain in the heart area;
- change in heart sounds during auscultation [weakened or prolonged 1st tone (in 70% of cases), less often (16% of cases) - its splitting, splitting of the 2nd tone (80%)].
Three-fascicle blockade has the most severe clinical manifestations:
- extremely low heart rate – 20–40 beats/min;
- severe shortness of breath at rest;
- interruptions in heart function;
- heart rhythm disturbances;
- dizziness;
- short-term episodes of loss of consciousness;
- cyanosis of the skin.
3. Symptoms and diagnosis
The possible clinical picture of the blockade varies over a wide range and is determined, firstly, by the localization of the conduction disorder, and secondly, by the degree of its reduction.
Thus, blockade of the right bundle branch is usually detected by chance, on a preventive or “commission” ECG, and is not accompanied by any symptoms. This phenomenon occurs both in absolutely healthy people and in well-trained athletes, but also in people who have suffered a serious cardiac disease in the past.
About the same can be said about partial blockades of one of the branches of the left bundle branch. However, a complete blockade of the left leg is much more often than a blockade of the right one, and is based on a serious pathology.
Finally, combined variants of blockade, especially complete atrioventricular block of the third degree (maximum severity) pose a real risk of developing life-threatening conditions - for example, ventricular and/or atrial fibrillation with sudden cardiac arrest and death within a few minutes in the absence of specialized emergency resuscitation.
The most common symptoms of clinically significant blockades are heart pain of varying nature and intensity, attacks of dizziness, arrhythmias, tachycardia, and syncope.
One of the diagnostic problems is that the presence of left bundle branch block makes it impossible to reliably diagnose (ascertain or exclude) myocardial infarction using an ECG. Blockade of the right bundle branch does not interfere with electrocardiographic diagnosis of a heart attack, but may itself be a symptom of a heart attack, or a symptom of thromboembolism, or simply an epiphenomenon that does not mean anything clinically.
In general, identifying any type of blockade in the structures of the His bundle automatically (regardless of the absence or presence of subjective complaints, their intensity, etc.) requires a more in-depth examination of the condition of the heart muscle and its functioning. For this purpose, various methodological modifications of ECG and EchoCG are prescribed, according to indications - MRI, MSCT, laboratory tests, etc.
About our clinic Chistye Prudy metro station Medintercom page!
What does bundle branch block look like on an ECG?
ECG signs characterizing a complete block of the right bundle branch include:
- An increase in the duration of the QRS complex beyond 0.120 seconds.
- The presence of a deformed long S wave in leads V4-V6.
- The presence of a three-phase (similar to the letter “M”) QRS in leads V1-V3.
Speaking about the signs of incomplete blockade of the right bundle branch, it is worth noting the absence of a pathologically long QRS complex on the ECG (its length is either normal or is at the upper limit of normal in the range from 0.090 to 0.110 seconds), but the presence of triphasicity when visually assessing the shape of the ventricular complexes.
Visual signs of complete (affecting both branches) blockade of the left leg on the ECG include:
- There may be a prolongation of the ventricular complex beyond 0.120 seconds.
- The presence of deep long S waves in leads V4-V6.
- The presence of long and deformed R waves in leads I, aVL and V5-V6.
- Absence of Q on graphs I, V5-V6.
The blockade of the anterior branch of the left bundle branch of His looks like this:
- A pronounced deviation of the heart axis to the left side (from -30 to -90 degrees).
- Ventricular complex of normal duration.
- Small R waves combined with deep S waves in II, III and aVF.
- Small Q waves in I and aVL.
Blockade of the posterior branch of the left leg of His looks like:
- A pronounced deviation of the heart axis to the right side (from +120 to +180 degrees).
- Ventricular complex of normal duration.
- Small Q waves in combination with high-amplitude R waves in II, III and aVF.
- Small R waves in I and aVL.
If the above-mentioned signs that fit the description of a blockade of the legs are detected on the ECG, the doctor must identify the root cause of this rhythm disturbance and make a diagnosis in accordance with government recommendations, and consider the blockade itself to be a manifestation of the disease.
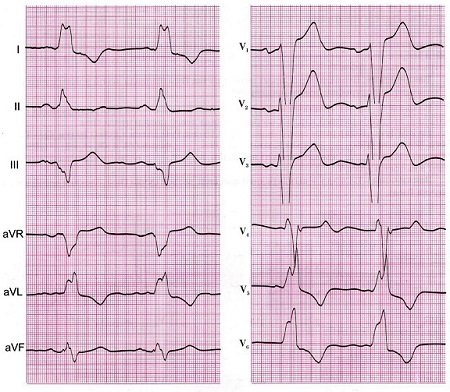
Left bundle branch block
Right bundle branch block
Blockade of the right leg together with the left posterior branch of the His bundle
Left bundle branch block
LBP blockade also causes widening of the QRSr complex, but its shape is not similar to PNPG blockade. The main reason for the difference is that RBBB block affects mainly the final stage of ventricular excitation, while LBB block affects the initial stage .
Remember that the first stage of ventricular excitation is depolarization of the left side of the interventricular septum. Blockade of LBP disrupts this process, and its depolarization occurs from right to left, and not vice versa, as is normal. Thus, the main change in the electrocardiogram with LBP block is the absence of the normal septal r wave in lead V1 and the septal q wave in lead V6 (Fig. 7-4, A).
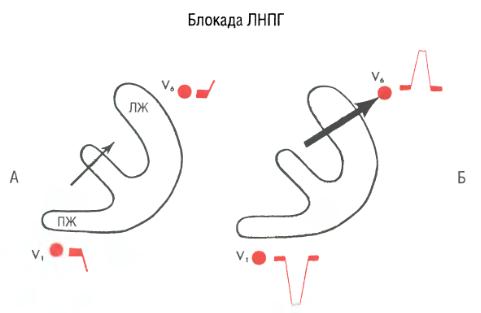
Rice. 7-4. Left bundle branch block. The sequence of ventricular depolarization results in a wide QS complex in lead V1 and a wide R wave in lead V6.
In addition, the total time of LV depolarization is prolonged. As a result, the QRS complex becomes very wide. In lead V6, a wide, completely positive R wave is formed (Fig. 7-4, B). The right precordial leads (eg, lead V1) have a negative QRS complex (QS) because the LV is still electrically dominant and its potentials are greater than the RV.
| With LBP blockade, the entire process of ventricular excitation is directed to the left precordial leads: depolarization of the interventricular septum occurs from right to left, the time of excitation of the electrically predominant LV is prolonged. | |
The sequence of ventricular excitation during LAP block is shown in Fig. 7-4.
With LBP block, a QS complex with a small notch at the apex is sometimes recorded in lead V1, giving it a W-shape . The R wave in lead V6 may also have a notch, acquiring an M- shape (Fig. 7-5).
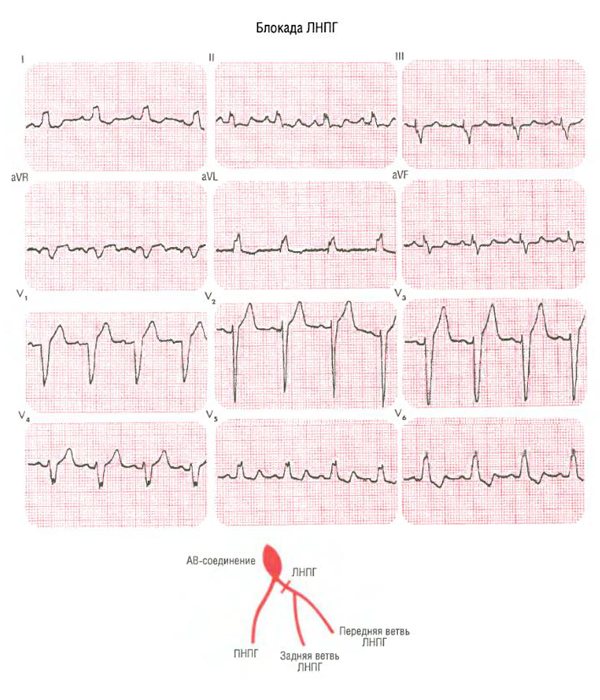
Rice. 7-5. Note the typical wide QS complex in lead V1 and the wide R wave with a slight notch at the apex in lead V6. Negative T waves in leads V5 and V6 are also typical.
Secondary T wave inversion occurs when not only the right but also the left bundle branch is blocked. T waves in leads with high R waves (eg, left chest) are negative, which is typical for LBB block (see Fig. 7-5). However, T wave inversion in the right precordial leads cannot be explained by LBP block alone. There, negative T waves reflect not secondary, but primary changes, for example, myocardial ischemia, see Fig. 8-21.
So, complete blockade of LBP can be diagnosed by leads V1 and V6:
- in lead V1, a wide, completely negative QS complex is usually formed (less often, a wide rS complex);
- in lead V6 there is a high, wide R wave without a q wave.
It is easy to distinguish between LBP block and PNPG block (Fig. 7-6).
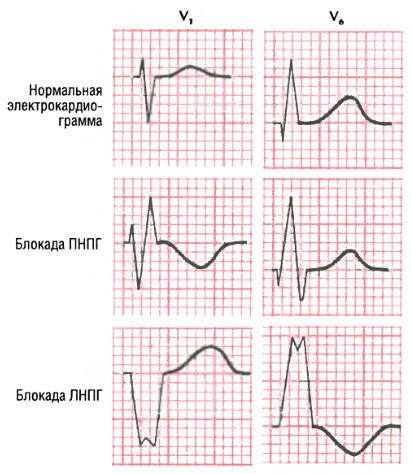
Rice. 7-6. Comparison of leads V1 and V6 with normal conduction, right and left bundle branch block. Normally, the rS complex is formed in lead V1, and the qR complex is formed in lead V6; with blockade of PNPG in lead V1 – a wide rSR' complex, in lead V6 – a qRS complex; with LBP blockade, in lead V1 there is a wide QS complex, in lead V6 there is a wide R wave.
However, sometimes wide QRS complexes are recorded on the electrocardiogram, which are not typical for any of the blockades. In such cases, the term “ intraventricular conduction delay ” is used (Fig. 7-7).
Rice. 7-7. Nonspecific disturbance of intraventricular conduction with a wide QRS complex (0.11 s), not typical for blockade of PNPG or LBP. In this case, the changes occurred against the background of myocardial infarction of the anterolateral wall of the left ventricle.
Consequences
Bundle branch block requires timely diagnosis, since if left untreated, the disease causes serious consequences, sometimes incompatible with the patient’s life. Among them are:
- tachycardia;
- ventricular fibrillation;
- thromboembolism;
- heart failure;
- heart attack;
- stroke;
- sudden death.
To prevent these complications, it is recommended to undergo regular preventive medical examinations. If heart pain, shortness of breath and other signs of the disease appear, you should contact a specialist immediately.
Treatment for bundle branch block
Treatment of the pathology depends on the type and electrocardiographic indicators at the time of diagnosis. Special treatment for damage to the right bundle branch is most often not required. In this case, the patient is recommended to follow measures aimed at preventing complications of the pathology.
To do this, the patient should adhere to the following rules:
- harden, douse yourself with cold water;
- respond adequately to stress;
- introduce teas into the diet, including soothing herbs (valerian, motherwort, elderberry, linden, nettle, oregano);
- give up heavy physical work and strength sports;
- maintain proper nutrition, avoid foods that increase cholesterol levels in the blood;
- exclude fatty, spicy, fried, smoked foods, mayonnaise, sauces, marinades, ketchups.
There is no specific drug treatment for this conduction disorder. Patients with right bundle branch block in the absence of an underlying disease do not require treatment. For patients with single- or double-fascicular blockade, the following groups of drugs can be prescribed for the treatment of the underlying disease:
- antioxidants – ubiquinone, carnitine, mexidol, preductal;
- vitamins – thiamine (vitamin B1) with lipoic acid, riboflavin (vitamin B2), nicotinic acid (vitamin PP);
- sedatives of plant origin (St. John's wort, motherwort, valerian, sage);
- antiplatelet agents to prevent thrombus formation in the heart and blood vessels - aspirin, cardiomagnyl, thrombo Ass;
- lipid-lowering drugs to normalize cholesterol levels - statins (rosuvastatin, atorvastatin, simvastatin);
- ananginal drugs for the treatment of coronary heart disease - short- and long-acting nitrates (nitroglycerin, isoket, cardiquet, monocinque);
- drugs for the treatment of diseases of the bronchopulmonary system that have caused the development of pulmonary heart disease - inhaled adrenomimetics and glucocorticosteroids (Berotec, Berodual, Spiriva, Beclazone);
- antihypertensive drugs for the treatment of arterial hypertension - ACE inhibitors (perindopril, lisinopril), angiotensinogen II receptor antagonists (losartan, valsartan), beta blockers (bisoprolol, atenolol), calcium channel antagonists (amlodipine, verapamil). The last two groups should be prescribed with caution, as they reduce the heart rate;
- antibiotics, non-steroidal anti-inflammatory drugs for inflammation of the membranes of the heart - penicillin; nimesulide, diclofenac;
- diuretics and cardiac glycosides in the development of chronic heart failure - indapamide, diuver, lasix; strophanthin, digoxin.
In addition to medication, a surgical method of blockade treatment is used, which consists of installing a pacemaker (pacemaker) in the patient. Complete right blockade, especially in combination with left hemiblockade (blockade of one branch of the left leg), and complete left blockade, developed in the acute period of myocardial infarction (10 - 14 days), are an indication for temporary cardiac pacing by introducing an electrode through the central vein into the right ventricle
Three-fascicle blockade with complete atrioventricular block, a rare rhythm of ventricular contractions and with Morgagni-Edams-Stokes attacks (attacks of loss of consciousness) is an indication for permanent cardiac pacing (implantation of an artificial pacemaker or cardioverter-defibrillator).
Right bundle branch block
N.B. Familiarize yourself with the lesson content and get a general idea of the topic. Don't try to remember all the details right away. It will be more convenient to do this when further performing step-by-step exercises for the lesson. The link to the exercises is at the bottom of the page.
Right bundle branch block is a blockade of the normal conduction of the excitation impulse to the right ventricle along the right bundle branch. In this situation, activation of the right ventricle occurs through a “bypass” through the left ventricle.
Scheme 1. Right bundle branch block
Diagram 2. Shape of the QRS complex in V1 and V6 with right bundle branch block
Schema source.
In Diagram 1, the blue arrow shows the location of the right bundle branch block. The yellow arrow shows the spread of excitation from the left ventricle.
This changes the shape of the QRS complexes, as shown in Diagram 2.
In the right precordial leads (V1, V2), the QRS complex takes the form of two R waves separated by an S wave. In V1, the QRS takes the form of an rSR (small r wave, regular S and then large R) or rsR (small r wave, small s and then big R). Moreover, in V1 the first R wave is less than the second in amplitude. In V2, the R waves may become equal in amplitude, or even the first R wave may become larger than the second.
In other cases, with blockade of the right leg in leads V1, V2, the QRS complex can take the form qR and R, i.e. be in the form of a tall, wide R wave with or without a small q wave.
In the left leads (V5, V6) the expansion of the S wave is recorded.
The ventricular complex expands. The duration of the QRS complex is equal to or greater than 0.12 s (more than 3 mm at an ECG recording speed of 25 mm/s). If a moderate increase in the duration of the QRS complex to 0.11-0.12 s is recorded, then they speak of incomplete blockade.
Look at the cardiograms below.
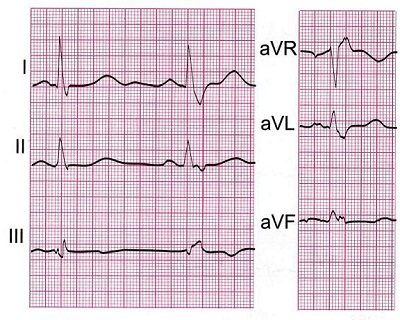
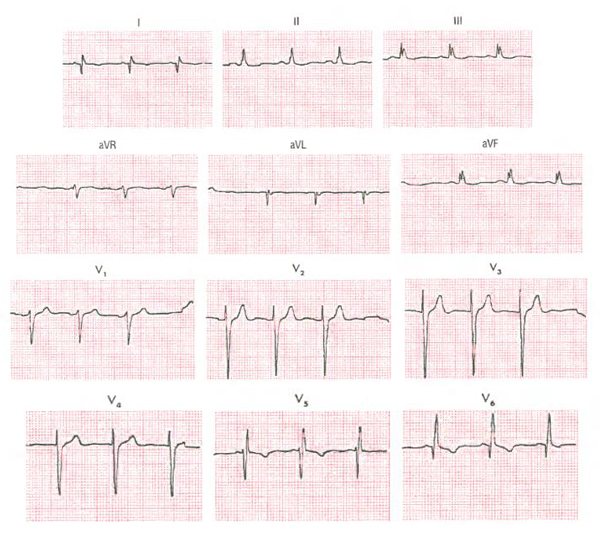
ECG 1. Cardiogram without deviations from the norm
ECG source.
ECG 1 shows no right bundle branch block. The QRS complex is not widened. The shape of the QRS complex in V1 is RS, the S wave in V6 is not widened.
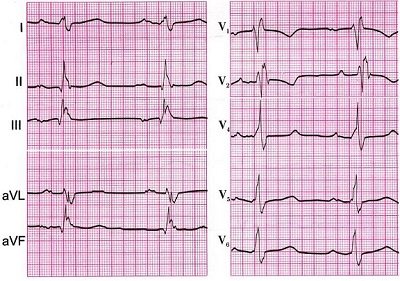
ECG 2. Right bundle branch block
ECG source.
ECG shows right bundle branch block. The QRS complex is widened and is 0.16 s (width 4 mm). The QRS shape in lead V1 looks like rSR: two R waves separated by an S wave. In this case, the first R wave is smaller than the second in V1. In V2 the tooth height ratio changes frequently, as in this case. In leads V5 and V6, the S wave is widened.
In addition, in the right chest leads V1, V2, oblique depression of the ST segment and a negative T wave are recorded, which is also characteristic of right bundle branch block.
Check out another cardiogram below.
ECG 3. Incomplete right bundle branch block
ECG source.
ECG 3 shows incomplete blockade of the right bundle branch. The shape of the QRS complex in lead V1 is rSR, but the width is less than 0.12 s (about 0.11 s). The main difference in incomplete blockade, visible on the ECG, is that the QRS width is from 0.11 to 0.12 s.
The main signs of right bundle branch block are:
- In leads V1, V2 (less often in leads III and aVF), the QRS complex takes the form of rSR, rsR, as well as qR or monophasic R.
- A widened S wave is recorded in leads V5, V6, as well as I and aVL.
- The duration of the QRS complex is equal to or greater than 0.12 s (3 mm) with complete blockade.
- With incomplete blockade, the QRS duration ranges from 0.11 s to 0.12 s.
- In lead V1, a downward-sloping depression of the ST segment and a negative T wave appear.
Go to exercises
Forecast
In conclusion, it should be said that bundle branch block is not a disease, but symptoms of heart disease that can manifest themselves clinically or be detected on an ECG. It is necessary to take into account the causes of the blockade, prescribe adequate treatment, and in this case it is possible to assume the consequences of a particular blockade.
If the patient has a single-fascicle right block and there are no pathologies of the heart and lungs, we can talk about a favorable prognosis.
An unfavorable prognosis in the case of a complete block of the left leg due to myocardial infarction, since in this case the mortality rate is 40-50 cases out of 100. In cases where the block is three-fascicle, there is a high probability of developing asystole and the prognosis is also unfavorable.
Prevention
Preventive measures include:
- avoidance of stressful situations;
- giving up alcohol and smoking;
- daily routine, full and restful sleep;
- refusal of fried, canned and spicy foods;
- taking medications only prescribed by a doctor and under his supervision;
- consumption of foods with a significant fiber content: fresh fruits and vegetables, herbs;
- timely diagnosis and treatment of diseases of all organs, not just the heart;
- mandatory consultation with a doctor if symptoms of the disease appear.
If an operation has been performed to install a pacemaker, a person should exclude the influence of electrical devices and a mobile phone on him. If you become ill, it is important to visit your doctor in a timely manner to assess the condition of the heart and the general well-being of the patient.