Complexes with this research
Miscarriage Identification of the main causes of miscarriage 40,070 R Composition
Female infertility Analysis of the state of women's reproductive health 16,210 R Composition
Coagulogram Study of the functional state of hemostasis 2,020 R Composition
IN OTHER COMPLEXES
- Examination during pregnancy. 3rd trimester 9,620 RUR
- Examination during pregnancy. 1st trimester 16,690 RUR
- Extended coagulogram RUB 4,150
- Entry into IVF RUB 23,020
- Pregnancy planning. Clinical indicators 6,630 R
Deficiency and excess of antithrombin III during pregnancy
From the very moment of conception, the body of a pregnant woman begins to prepare for childbirth. In this case, preparation occurs throughout the hemostatic system, which affects the state of the anticoagulant factor. To a greater extent, these changes are noticeable during the third trimester of pregnancy.
The body strives to prevent bleeding during labor, so it increases the level of clotting factors in the blood. Fibrinolytic activity of plasma decreases, the level of coagulation inhibitors, including antithrombin III, decreases. This becomes noticeable precisely towards the end of the third trimester. However, normally, the level of antithrombin III should not decrease to less than 65%.
Sometimes with hereditary deficiency of antithrombin III, its fall is erased, which cannot be determined in the laboratory. This is especially common during pregnancy, which is accompanied by severe toxicosis. This condition is dangerous because an artificial termination of pregnancy is possible, and after childbirth a woman may develop venous or arterial thrombosis, an infarction of internal organs or pulmonary embolism. Therefore, if a patient is at risk for this condition, she should be under special supervision by a doctor.
An increase in antithrombin III during pregnancy threatens the development of bleeding. This happens against the background of severe pathologies, for example with cholestasis or acute hepatitis.
Detailed description of the study
During bleeding, platelets circulating in the blood plasma, with the participation of many clotting factors, form a clot. Along with this, under the influence of thrombin, the fibrin protein is formed, which stabilizes the formed blood clot, after which the bleeding stops.
Antithrombin III is a protein that regulates blood clotting. This protein prevents the formation of blood clots, which is necessary to maintain balance between the coagulation and anticoagulation systems. To this end, antithrombin III binds to enzymes called serine proteases, as well as thrombin, factor IXa and Xa, and inhibits their activity. Sufficient amounts of clotting factors and antithrombin III allow bleeding to be stopped without excessive clot formation.
Antithrombin III deficiency is associated with an increased risk of thrombosis and thromboembolism. It may be hereditary or acquired. According to various estimates, the prevalence of hereditary antithrombin III deficiency ranges from 1 in 2000 to 1 in 5000 cases.
Hereditary antithrombin deficiency is divided into type I and type II. Type I leads to the complete absence of this protein in the blood due to the absence of genes that ensure normal synthesis of antithrombin III. Type II deficiency is characterized by the production of altered protein, which impairs its function. The overall activity of antithrombin III decreases.
Lack of production or incomplete activity of antithrombin III most often manifests itself in the form of deep vein thrombosis. However, there is a risk of repeated sudden thrombosis of atypical vessels, for example, veins of the brain or intestines. The first occurrence of thrombosis occurs at a relatively young age, with the risk of blood clots peaking between the ages of 15 and 40 years. This is especially important against the background of concomitant factors that increase the risk of thrombosis, for example, during pregnancy.
Acquired deficiency of antithrombin III is usually associated with either a decrease in its production in the liver in the case of liver failure, cirrhosis, malnutrition, or with loss of protein by the body in nephrotic syndrome and some other conditions. A decrease in the concentration of antithrombin III is observed in coagulopathies, including disseminated intravascular coagulation syndrome, microangiopathy with thrombosis. In many malignant neoplasms, its production is also disrupted. The use of the anticoagulant heparin significantly increases the activity of antithrombin III, which makes it possible to prevent thrombosis.
The influence of antithrombin III on the body is extensive, so determining the level of this indicator in the blood allows you to avoid the negative consequences of its deficiency and select treatment.
Antithrombin III
Antithrombin III is a specific protein of the blood coagulation system. Its main function is to inactivate several major clotting factors, including thrombin, and prevent increased formation of blood clots (thrombi).
Synonyms Russian
AT III, AT3.
English synonyms
Antithrombin (Activity and Antigen), Functional Antithrombin III, AT III.
Research method
Colorimetric method.
Units
% (percent).
What biomaterial can be used for research?
Venous blood.
How to properly prepare for research?
- Do not eat for 12 hours before the test.
- Avoid physical and emotional stress 30 minutes before the test.
- Do not smoke for 30 minutes before donating blood.
General information about the study
Antithrombin III is synthesized mainly in the vascular endothelium and liver.
The blood is thin due to anticoagulants, one of which is antithrombin III, which blocks clotting factors.
Typically, when a vessel is damaged, the body activates a series of coagulative factors (coagulative cascade) to form a blood clot and prevent further blood loss. Antithrombin III helps regulate this process - it slows down the action of several coagulation factors, including thrombin, as well as factors Xa, IXa and Xia, designed to prevent the formation of excess blood clots.
Patients with antithrombin III deficiency are at risk for thrombosis. Inherited deficiency is rare (1 case in 5000 patients). If the patient has a genetic predisposition, thrombotic episodes usually make themselves felt already in 20-30 years.
There are two types of antithrombin III deficiency. In the first, normal antithrombin III is produced, but in insufficient quantities. In the second type, it is produced in sufficient quantities, but is dysfunctional. A decrease in antithrombin III levels can be caused by the following reasons:
- congenital antithrombin III deficiency,
- liver diseases with impairment of its functions (cirrhosis, cancer),
- nephrotic syndrome (diseases that occur with significant loss of protein in the urine),
- massive thrombosis (for example, pulmonary embolism),
- extensive surgical interventions,
- using large doses of oral contraceptives,
- long-term administration of heparin,
- DIC syndrome (severe disruption of all blood coagulation processes, which can occur in many critical conditions: shock, severe trauma, burns, massive thrombosis, etc.),
- extensive thrombosis,
- blood loss,
- oncological disease.
Regardless of the reasons for insufficient antithrombin III levels, its main manifestation is recurrent arterial and venous thrombosis.
Hereditary deficiency of antithrombin III is especially characterized by frequent myocardial infarctions and strokes at a young age.
What is the research used for?
- To determine whether the amount of functional antithrombin III in the blood is normal (before the antigen test).
- To evaluate patients whose body does not respond normally to heparin.
When is the study scheduled?
- Together with tests for protein C and protein S and for lupus anticoagulant.
- When a patient has venous thrombosis.
- After removal of the blood clot.
- When examining patients whose body does not respond normally to heparin, when it is necessary to use large doses of this drug to achieve the desired level of anticoagulation.
What the results mean ?
Reference values
| Age | Reference values |
| Less than 3 days | 58 — 90 % |
| 3 days – 1 month | 60 — 89 % |
| 1 month – year | 72 — 134 % |
| 1-6 years | 101 — 131 % |
| 6-11 years | 95 — 134 % |
| 11-16 years old | 96 — 126 % |
| More than 16 years | 66 — 124 % |
| Week of pregnancy | Reference values |
| 13-21st | 74 — 115 % |
| 21st-29th | 73 — 114 % |
| 29-35th | 76 — 112 % |
| 35-42nd | 70 — 116 % |
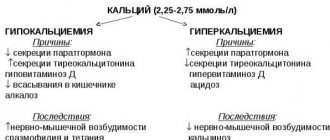
Increased antithrombin III levels are associated with an increased risk of bleeding.
Reasons for increased antithrombin III levels:
- long-term use of indirect anticoagulants (warfarin, phenylin),
- vitamin K deficiency,
- liver diseases,
- acute viral hepatitis,
- inflammatory process,
- menstruation.
Reasons for decreased antithrombin III levels:
- activation of the blood coagulation system - tendency to thrombotic complications,
- late stages of pregnancy,
- mid-menstrual cycle.
General information
Antithrombin III (glycoprotein, plasma protein) is the main anticoagulant of the blood system, which blocks coagulation factors and promotes its natural thinning. Its main function is to regulate the formation of blood clots during bleeding, that is, to deactivate excessive thrombus formation.
Analysis for antithrombin III as part of a coagulogram allows you to evaluate its quantity (antigen test) and quality (activity).
As a result of injury, impact, compression or surgery, the integrity of the tissue and, as a result, the vessels located in it are damaged. The body's response to damage is the release of coagulative components, which contribute to the formation of a blood clot that stops bleeding in the vessel. Antithrombin III regulates the process of thrombus formation, since an excessive number of such clots leads to complete blockage of the lumen of the vessel, which prevents blood from entering a certain area.
The glycoprotein antithrombin III is produced by the inner layer of blood vessels - the endothelium - and liver cells with the participation of vitamin K. After synthesis, it is released into the bloodstream, where it inhibits the coagulation factor thrombin, as well as IXA, XA, XIA, XIIA factors. The natural process proceeds quite slowly, but in the presence of heparin it accelerates sharply. If the level of antithrombin decreases critically, then heparin loses its biological activity - there is a risk of vascular blockage (thrombosis).
Plasma protein deficiency can be acquired and hereditary (1:5000 cases). If the patient is at risk, thrombosis can develop after 20 years.
Experts define 2 types of deficiency. In the first case, antithrombin is biologically active, but is produced in insufficient quantities. The second type is characterized by normal secretion of defective antithrombin, which is not capable of performing an anticoagulation function.
Regardless of the reasons for the decrease in the concentration of this protein, the main manifestation of deficiency is thrombosis of the veins and arteries, which periodically recur. In pregnant women, insufficient production of antithrombin increases the likelihood of spontaneous abortion.
Congenital deficiency manifests itself as strokes or myocardial infarctions in young patients, thrombosis in infants (rarely). The condition is also aggravated by pregnancy and childbirth, surgical interventions, infectious and inflammatory processes, and the use of oral contraceptives.
Normally, antithrombin decreases with age in men, and in women after menopause.
Indications
Antithrombin III testing is most often carried out as part of a coagulogram in the following cases:
- Screening of patients at risk (there were cases of antithrombin deficiency in the family history, thrombosis of veins or arteries was observed before the age of 50);
- Estimation of the amount of functionally useful antithrombin III;
- Thromboembolic pathologies: thrombosis of deep veins or mesenteric vessels;
- myocardial infarction;
- pulmonary embolism;
- stroke;
- thrombophlebitis;
- miscarriage (history);