Blood gas studies and pulse oximetry
Pulse oximetry and blood gas testing procedure
Among the most accurate methods for determining how well the body is supplied with oxygen, a special place is occupied by the study of blood gases and pulse oximetry.
Basic task
Blood gas testing is used for diseases of the cardiovascular and respiratory systems. This is done to determine the oxygen saturation of the body. Carrying out the research is quite simple. To do this, a puncture method is used, in which blood is taken directly from the artery. Due to this, the method belongs to the category of invasive. After the artery is punctured, a bandage should be applied to it for about 10-15 minutes. This is necessary to prevent bleeding. The sample obtained during the sampling process is immediately sent to the laboratory for testing. At this stage, the amount of gas in the blood is determined. Here, the determination of carbon dioxide, partial pressure, pH indicators, the quantitative composition of bicarbonates and how saturated hemoglobin in red blood cells necessarily occurs. The following are considered normal values:
- PaCO2 - 34-45 mm Hg;
- PaO2 - 75-100 mm Hg;
- SaO2 - 94-100%;
- pH of 7.35-7.45;
- HCO3 - 22-26 mEq/liter.
Pulse oximetry method and its information content
The most accurate method to recognize respiratory failure and assess the general condition of the respiratory system is to study blood gases. As soon as a person begins to experience respiratory failure, the process of developing hypoxia (decreased oxygen levels) and hypercapnia immediately occurs - an increase in the amount of carbon dioxide in the composition.
The presented research method is used to recognize restrictive and obstructive pulmonary diseases in a chronic form. These include diseases such as sarcoidosis, bronchial asthma, tuberculosis, and occupational lung diseases. The research procedure takes place only on the hospital premises.
To conduct the study, the patient does not require special preparation. If a person uses anticoagulants, anti-inflammatory drugs and aspirin, you need to warn the doctor about this. As for the dangers of this procedure, this includes the possibility of bleeding after the puncture.
Features of pulse oximetry
Pulse oximetry is a method that can be used to determine the oxygen saturation of hemoglobin in the blood. For this, a special device called a pulse oximeter is used. Depending on the amount of oxygen, the change in blood color allows you to determine the necessary parameters. The convenience of this method is that there is no need to collect venous blood.
Conducting the research and its informativeness
During the procedure, a special sensor is placed on the patient’s finger, in which the main source is light. Passing through the phalanx and capillaries, the process of recording the change in blood color occurs depending on how saturated it is with oxygen. The data is recorded on the device screen in the form of saturation curves. To get the most accurate result, it is necessary to ensure complete immobility of the finger. The normal rate should be 95-98%. To recognize respiratory failure and other problems with the respiratory system, the blood saturation method is informative. If the quantity is insufficient, the indicator drops below 95%. This method is often used by anesthesiologists during surgical interventions. No special preparation is needed for the procedure. The method does not lead to complications and is safe for the human body.
Pulse oximetry: principle of operation
Pulse oximetry is an extremely accessible method of patient monitoring. This is especially important when there is limited funding for a medical institution. Allows you to monitor several parameters of the patient’s condition at once. Initially, the use of the most accurate pulse oximeters was required in intensive care units, then everywhere. But proper use of pulse oximetry requires special skills. If used incorrectly in a general therapy department, there may be a threat to the life and health of the patient. Let's consider the operating principle of a pulse oximeter, the features of the modern method, and possible limitations. And also, what alternatives to this method exist.
Principle of operation
A pulse oximeter is a high-precision device that measures the degree of oxygen saturation of arterial hemoglobin. The technology is based on 2 principles: absorption of light by hemoglobin and pulsation of the light signal as it passes through tissue, which occurs due to changes in the arterial bed. This component can be separated from the non-pulsating component using a special microprocessor. When used correctly, oximetry becomes the most useful method for monitoring the state of the cardiorespiratory system. As a result, 2 indicators are displayed on the monitor:
- hemoglobin oxygen saturation of arterial blood;
- heart rate (measured over 5 - 20 seconds).
Several factors influence the correct operation of the device. These include external light, pulse frequency and rhythm, hand tremors, and pathological hemoglobin. Reliability can also be affected by vasoconstriction, pathological hemoglobin, and characteristics of the heart.
The pulse oximeter only shows the level of ventilation of the blood, but not the level of ventilation. With low qualifications of the medical worker, this often creates a false picture when inhaling oxygen. In such a situation, there is a risk of missing the initial symptoms of hypoxia, which occurs with airway obstruction.
What does a pulse oximeter measure?
A pulse oximeter consists of several elements:
- sensor for collecting indicators (attached to a finger, earlobe or nose);
- microprocessor for processing results;
- display for processing the results.
The device shows the average amount of oxygen that is associated with each hemoglobin molecule. Data is displayed on the monitor simultaneously with an audio signal. Its height varies depending on the level of saturation. Pulse rate is measured based on the number of beats per minute. The pulse oximeter does not provide information on the following indicators:
- blood oxygen level;
- amount of dissolved oxygen;
- tidal volume;
- breathing rate;
- cardiac output value;
- arterial pressure.
Systolic pressure is determined by the appearance of a wave on plethysmography during cuff deflation.
Principles of modern pulse oximetry
The principle of modern pulse oximetry is the relationship between partial pressure of oxygen and saturation. This indicator is reflected in the hemoglobin dissociation curve. Under different conditions, it can move to the right or left. For example, this can occur during blood transfusion.
Operating principle of a pulse oximeter:
Oxygen is transported through the bloodstream mainly in the form of hemoglobin. One molecule of hemoglobin can carry 4 molecules of oxygen and in this case it will be 100% saturated. The average percentage of saturation of the population of hemoglobin molecules in a certain volume of blood is the oxygen saturation of the blood.
The sensor contains two LEDs, one of which emits visible light in the red spectrum (660 nm), the other in the infrared spectrum (940 nm). The light passes through the tissue to the photodetector, and part of the radiation is absorbed by the blood and soft tissues, depending on the concentration of hemoglobin in them. The amount of absorbed light of each wavelength depends on the degree of oxygenation of hemoglobin in the tissues.
- The microprocessor is able to isolate the pulse component of blood from the absorption spectrum, i.e. separate the arterial blood component from the permanent venous or capillary blood component. The latest generation microprocessors are able to reduce the effect of light scattering on the operation of the pulse oximeter.
Multiple divisions of the signal over time are accomplished by cycling the LEDs: red turns on, then infrared, then both turn off, and so on many times per second. This eliminates random background noise.
A new feature of microprocessors was quadratic multiple division. The red and infrared signals are phase-separated and then recombined. With this option, interference from motion or electromagnetic radiation can be eliminated, since they cannot occur in the same phase of the two LED signals.
Like heart rate, saturation is calculated on average in 5-20 seconds. The first indicator is calculated by the number of LED cycles and strong pulsating signals over a certain period of time. Based on the proportion of absorbed light of each frequency, the microprocessor calculates their coefficient. The pulse oximeter memory contains a series of oxygen saturation values obtained in experiments on volunteers with a hypoxic gas mixture. The microprocessor compares the resulting absorption coefficient of the two wavelengths of light with the values stored in memory. It is unethical to reduce oxygen saturation in volunteers below 70% in clinical studies. Because of this, a saturation value below 70% obtained from a pulse oximeter is not reliable. Reflected pulse oximetry uses this type of light. Can be used proximally, for example on the forearm or anterior abdominal wall. The operating principle is the same as that of a transmission pulse oximeter. A significant drawback is the difficulty of attaching to the body.
Reasons for reducing the saturation index
Insufficient oxygen saturation in the blood can occur for various reasons. The most common ones are:
- insufficient amount of hemoglobin in the blood or decreased sensitivity to oxygen;
- impaired ventilation of the lungs, such as edema;
- respiratory mechanics are impaired: apnea or dyspnea;
- lack of blood entering the pulmonary circulation;
- heart defects;
- stay in high mountains;
- disturbance of circulation in the large circle.
Due to the reasons for the decrease in blood saturation, symptoms of this condition appear:
- dizziness;
- weakness, lethargy;
- dyspnea;
- decrease in blood pressure.
The presence of such signs may indicate a significant lack of oxygen in the blood and possible pathological processes beginning in the body. With advanced forms of saturation, hemorrhagic shock may occur. The consequences of this condition can be very serious for the body.
Blood gas composition
The main stream of inhaled air contains approximately 21% oxygen, 0.04% carbon dioxide and 78% nitrogen. As it moves through the respiratory tract, the air becomes warmed and humidified. The human bronchi reduce the pressure of incoming air.
The human body eliminates carbon dioxide - gas and bicarbonate. A small part of the gas in dissolved form is transferred by plasma to the respiratory organs. A significant part of the gas, together with water, produces carbonic acid. Blood cells contain an enzyme called carbonic anhydrase. Due to it, the formation of carbonic acid is accelerated. Some carbon dioxide reacts with hemoglobin.
In the human body, carbon dioxide is available in a free state, a chemical compound with water, as well as hemoglobin and plasma proteins. The normal pressure is 40 mmHg in the venous and 46 mmHg in the venous. The level of carbon dioxide in the blood is 50 ml/dl. An increase in gas concentration occurs as blood moves through tissue. Its fall is observed as blood moves through the respiratory organs.
By combining with protein, oxygen displaces carbon dioxide from the blood. This phenomenon is called the Holdlein effect.
Interpretation of the law
The scientist Dalton in 1801 formed the law of partial pressures: Pa of a mixture of ideal gases is equal to the sum of pi of its components. The equation has the following form: Рcm=n (sum pi), where n is the number of shares of the mixture.
To determine partial pressure in chemistry, a separate component from atmospheric air is used. The calculation takes into account the value of each individual substance, their number, temperatures and volumes. If necessary, you can find the overall indicator by adding the pressure of each component separately.
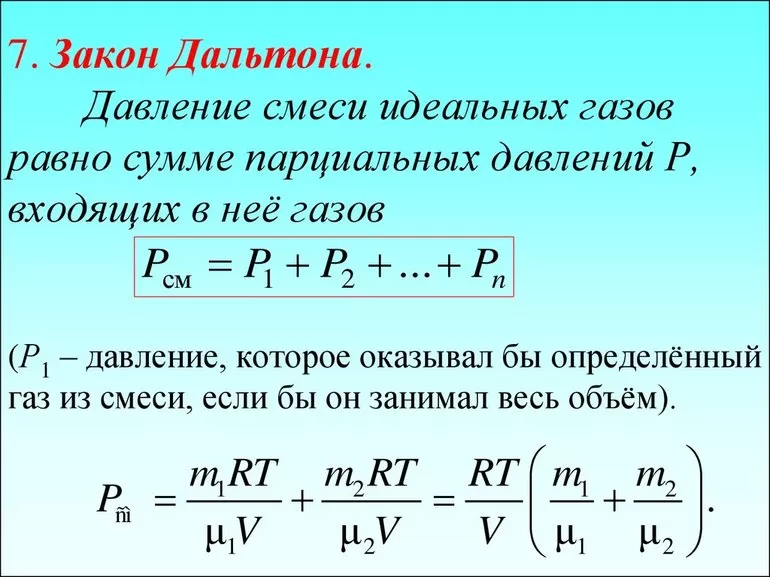
Each gas in the vessel must be designated as “ideal”. Under normal conditions, they interact with carbon dioxide, hydrogen, water, nitrogen, water vapor, oxygen, blood components and other components from the periodic table. In this case, no connections are formed. Individual molecules are able to collide with each other, repelling, but not deforming.
Physical and chemical problems are solved using the partial pressure formula (the law was discovered by scientists Boyle and Marriott): (k = P x V). In addition to the full version, the equation is written abbreviated k = PV, where:
- k is equal to a constant value;
- P—pressure;
- V—volume.
Increase - partial pressure
The increase in partial pressure of CO2 with increasing temperature is caused by a decrease in the pH of the solution. Below are the pH values for 28% ammonia water.
An increase in the partial pressure of D or E, one of the reaction products, causes the reaction to proceed in the opposite direction, which leads to a decrease in the partial pressure of this reaction product, which tends to reach its original value.
Increasing the partial pressure of carbon monoxide has a beneficial effect on the yield of linear products. The partial pressure of hydrogen has little effect on the yield of the linear product.
Due to an increase in the partial pressure of ammonia, its release into the gas phase increases during the evaporation of solutions containing diammonium phosphate.
As the partial pressure of CO2 increases, the corrosion rate increases. As the temperature of the environment increases, the intensity of corrosion also increases significantly.
| Equilibrium of sulfuric anhydride with oxygen and sulfur dioxide depending on temperature and oxygen content in gases and at different pressures.| Dependence of sulfate dissociation pressure on PPSO temperature. |
With an increase in the partial pressure of SO3 in gases, sulfates are formed, and with a decrease, they decompose.
| Dependence of speed ab. |
With an increase in the partial pressure N0, starting from a certain value, the relative increase in the absorption rate slows down.
As the partial pressure of CO2 increases, the corrosion rate increases. As temperature increases, the corrosion rate also increases significantly. During development, the partial pressure of CO2 decreases, and the volume of water condensate increases, and therefore the intensity of corrosion decreases.
As the partial pressure of CO2 increases, the corrosion rate increases. As the temperature of the environment increases, the intensity of corrosion also increases significantly.
With an increase in the partial pressure of propylene and oxygen, the yield of AC increased, and with an increase in the partial pressure of HCI to certain values, a saturation phenomenon was observed, which indicates a relatively strong connection between the catalyst and chlorine.
How does an increase in the partial pressure of hydrogen iodide affect the rate of non-catalytic and catalytic reactions.
| Gas purification from H2S and CO2 with MEA solution. |
Therefore, when the partial pressure of the removed acid gases increases above 0 2 kgf/cm2, a corresponding increase in the amount of circulating solution is required. MEA solutions are prone to foaming, which is intensified by the condensation of hydrocarbons in the absorption column. Careful removal of droplet hydrocarbons before gas purification and supply of the regenerated solution at a temperature 5 - 15 C above the incoming gas temperature can significantly reduce the risk of foaming and loss of MEA.








