Problems with breastfeeding
It often happens that a woman has a desire to breastfeed her baby, and she conscientiously listened to lectures at prenatal training courses on feeding a child, and her relatives are all in with both hands, and life makes its own adjustments. In this article we will focus on the most common problems that arise during breastfeeding, which can occur in any woman. But we will not touch upon complex cases that require professional pediatric care. So, the following problems may arise in the maternity hospital.
Inflammation, bruising, cracked nipples occur when:
- incorrect attachment of the child to the breast: from the very beginning, it is necessary to ensure that the child opens his mouth wide, grasps the areola completely, lips are turned outward, and the chin is pressed to the chest. If the baby sucks on the breast only by the nipple, then the mother experiences pain during feeding. Such sucking always injures the nipple. Therefore, you don’t have to endure it, as many women do. You need to carefully place your little finger in the corner of the child’s mouth, open the mouth and take out the nipple. Then, wait until the baby opens his mouth wide and give him the breast correctly. And remember, proper breast latch is a skill that your baby will learn with your help;
- The use of breast simulators contributes to the baby's pacifier and pacifier confusion. And as a result, improper breast grip. Therefore, remember the rule - until the child has learned to grasp the breast correctly, he should not see the nipple and pacifiers;
- improper breast care: washing the breast with soap before each feeding, using disinfectants (for example, brilliant green) leads to washing off the protective fat layer from the surface of the nipple, and it remains defenseless. Sometimes inflammatory changes occur in women who use waterproof breast pads. Therefore, let us recall the rules of breast care: you need to wash your breasts during a hygienic shower, that is, once a day; After feeding, you can treat the nipple with hind milk and leave the breast open to air dry; use underwear and breast pads made of cotton fabric, preferably without seams.
If abrasions or inflammation of the nipple occur, it is often enough to correct the position of the baby at the breast and follow the rules of breast care. The frequency of feedings is not limited. If nipple inflammation does not go away within 7 days or is wavy in nature, you should consult a doctor. There may be a fungal infection and special treatment is required. A nipple crack can be quite deep and bleed after feeding. During feeding, pain is noted. To treat a fissure, you will need to temporarily, for 12 hours, wean the child from feeding the problematic breast. She needs to be expressed at least 3 times a day and the baby needs to be fed expressed milk from a spoon if he doesn’t have enough milk from the healthy one. To treat a crack, a wound-healing ointment without a specific unpleasant odor is suitable.
Dry breast skin
It may occur 2-5 days after birth and be accompanied by pain. The breasts increase in size and become hot, firm and shiny due to swelling. There is a complication of milk outflow. The most common reasons for this are:
- delayed breastfeeding;
- limiting the duration of breastfeeding;
- improper attachment of the baby to the breast;
- rare breastfeeding.
Therefore, the main prevention of dry breast skin is to put the baby to the breast as early and correctly as possible and to ensure that the baby is fed upon his first request, without limiting either the frequency or duration of sucking.
Delayed breastfeeding most often occurs in the case of a cesarean section or health problems in the child. Of course, these are special cases that require special attention from the maternity hospital staff and relatives. If the birth occurred by cesarean section, you must:
- attach the baby as early as possible, preferably while still in the operating room, even if the mother is still under the influence of sedatives;
- the child must be in the same room with the mother to ensure that the child is fed as required. Of course, a woman will need help in caring for a child;
- if for some reason the baby cannot be temporarily put to the breast, it is necessary to establish pumping of both mammary glands as soon as possible after birth (at least within the first 12 hours). It is necessary to express milk for 15-20 minutes, 6-8 times a day in sterile jars so that it can be used to feed the baby. You can read more about this in our article on expressing breast milk.
Changes in the breasts during pregnancy and lactation. The structure of the nursing breast
One of the first changes that most women notice with the onset of pregnancy is the metamorphosis that occurs with the breasts. As a rule, it becomes very sensitive to touch and increases in size. Why is this happening?
The fact is that with the onset of pregnancy, a woman’s hormonal levels begin to change. In particular, the levels of the hormones estrogen, progesterone and prolactin increase. Under their influence, intensive development begins, the growth of glandular tissue (a special structure in which milk will be produced), the system of milk ducts.
This is interesting! The average weight of the mammary gland in an adult woman is 150-200 g, and during lactation - 400-500 g!
Figure 1. Breast changes during pregnancy.
Figure 2. The main structural elements of the lactating (nursing) breast.

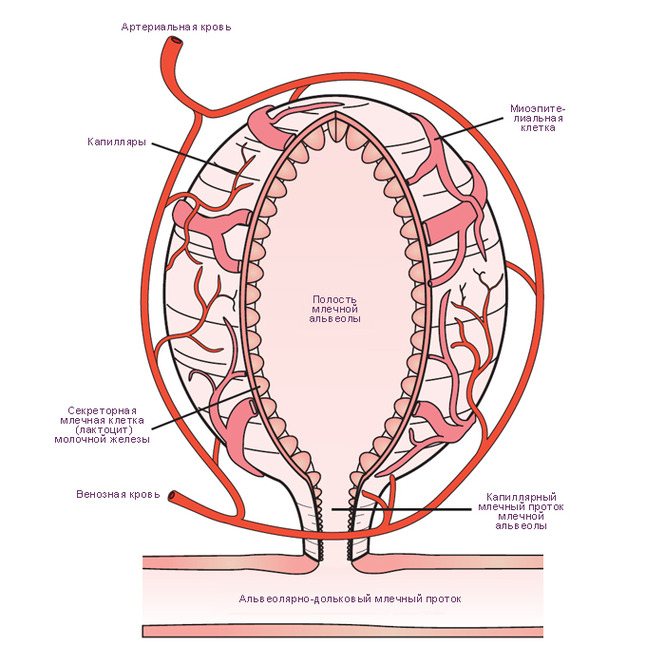
- The mammary gland consists of 15-20 lobes (according to other sources - 7-10).
- Each lobe consists of 30-80 lobules.
- Each lobule contains 150-200 alveoli (special “bags” in which milk is stored).
- The inner surface of each alveoli is “lined” with lactocytes - cells that produce milk (see Figure 3).
- At the top of the nipple, 8 to 15 milk pores open. There are cases where women even had 1 excretory duct, but, as a rule, the number of ducts is equal to the number of lobes.
Figure 3. Structure of the alveoli
Thus, literally from the first weeks of pregnancy, the mother’s body begins to prepare for the next stage after childbirth - feeding the newborn. This process occurs unevenly, with significant individual fluctuations.
The initial period (about 10 weeks) is characterized by a rapid increase in breast size. Hidden stage (2-4 weeks), when practically no external changes occur. Next, the development of the glands resumes and gradually increases until the beginning of lactation.
The processes of growth and strengthening of excretory capacity continue in the postpartum period, reaching a maximum in the first two weeks of lactation.
IMPORTANT! These time frames are very arbitrary. They can vary greatly for each individual woman. Sometimes it happens that a woman feels virtually no changes in her breasts during pregnancy, but this does not prevent her from successfully feeding her baby in the future... And yet, if absolutely no changes have occurred in the breasts during the entire period of pregnancy, this can be alarming signal. Be sure to tell your doctor or lactation consultant if you have any difficulties breastfeeding. This information will allow the specialist to give more accurate recommendations.
The next noticeable change for the mother occurs around 3 months after birth. The breasts no longer become full between feedings and remain soft almost all the time (unless the mother is forced to take a longer than usual interval between feedings). It happens that the mother is disturbed by these sensations, it seems that “the milk has disappeared.” But in fact, the mother’s body has perfectly adapted to the needs of a particular child; milk is produced exactly as much as the child needs. From this time on, lactation is considered “mature” and established.
But as time goes on, the baby grows, breastfeeding becomes less and less, and the baby begins to suck out less milk, gradually, very smoothly replacing it with food from the family table (normally, this process takes from several months to several years). In the process of completing breastfeeding, reverse transformations occur in the breast (involution of the mammary gland): with a reduction in the number of breastfeedings, the amount of glandular tissue gradually decreases, being replaced by fatty tissue.
A bit of mythology 

Myth. Breastfeeding greatly damages the shape of your breasts.
In fact. The most dramatic changes occur in the breasts during pregnancy and the arrival of milk. These changes do not depend on whether the woman breastfeeds or not. However, if a woman has fed and completed feeding smoothly within a physiological time frame*, then there is a high probability of restoring breast shape. The extent to which the breasts will restore their shape after completion of lactation depends to the greatest extent on the characteristics of the individual woman and the extensibility of the connective tissue.
*WHO calls the physiological end of lactation no earlier than 1.5 years.
Myth. The breasts need to be prepared for feeding (massage, put hard cloth in the underwear “to make the nipples harden”, smear something “for elasticity”, etc.).
In fact. There is no need to prepare the breast for feeding; it is designed in such a way by nature that by the time of birth it is completely ready to feed the baby. The above actions may cause skin irritation and nipple injury. Regular long-term manipulation of the nipple at the end of pregnancy can provoke premature onset of labor.
Myth. The smaller the breast, the less milk it contains.
In fact. Breast size does NOT affect your milk supply. Breast size mainly depends on the amount of fatty tissue, and milk is produced in the glandular tissue, which is located deep inside.
Myth. I have flat (inverted) nipples and will not be able to breastfeed.
In fact. When the breast is latched correctly, the baby sucks not the nipple, but the areola. The nipple is located deep in the baby's mouth, on the border of the hard and soft palate and, in fact, it is just a point from which milk flows. The shape of the nipple does NOT affect a woman's ability to breastfeed.
You can read more about exactly how milk is produced here.
Melnikova Rada, breastfeeding consultant
Sources:
1. Materials of the training course for breastfeeding consultants under the WHO/UNICEF “Progv” program https://progv.ru/
2. WHO “Counseling on infant and young child feeding”, 2006 https://apps.who.int/iris/bitstream/10665/43567/9/9789241594752_rus.pdf
3. Materials of the advanced training course “New Level” https://www.new-degree.ru/
4. A. Edgar. Anatomy of the breast of a nursing mother https://www.llli.org/russian/nb/anatomy.html
5. Inside the nursing breast: latest anatomy research https://gvinfo.ru/node/144
Basic recommendations for the treatment of hardening of the mammary glands:
- Put your baby to the breast often if he can breastfeed. To make it easier for your baby to grasp the hard areola, you can pump your breasts a little before feeding. If the baby cannot suckle, then it is necessary to express the breast manually or with a breast pump;
- stimulate the oxytocin reflex before feeding or pumping;
- drink warm tea or herbal decoction (not coffee);
- take a warm shower or apply a warm compress to the mammary gland for 10-15 minutes;
- massage your back and neck;
- lightly massage your breasts;
- stimulate the skin of the nipple;
- relax;
- After feeding, to reduce swelling, apply a cold compress for 15 minutes.
Dangerous consequences of lumps in the mammary gland during breastfeeding
Mastitis is the most hated consequence of stagnation. And if mastitis is not treated in time, purulent formations may appear in the mammary gland, which will require surgical intervention.
This means the end of natural feeding. That is why everything must be done to prevent the formation of mastitis. A spontaneous feeling of heat (temperature up to 40 °C) should alert you. The main thing is not to panic and consult a doctor in a timely manner. With the help of physiotherapeutic and ultrasound procedures it will be possible to clear the ducts.
ONLINE REGISTRATION at the DIANA clinic
You can sign up by calling the toll-free phone number 8-800-707-15-60 or filling out the contact form. In this case, we will contact you ourselves.
If you find an error, please select a piece of text and press Ctrl+Enter
Blockage of the milk ducts (lactostasis) and mastitis most often result from:
- violation of the rules of feeding a child: restrictions on the duration and frequency of sucking, improper attachment to the breast, pressing with fingers on the chest during feeding;
- wearing thick underwear;
- stress and excessive stress: lead to a decrease in the frequency of the baby’s attachment to the breast and a decrease in immunity;
- fissure of the nipple - are an entry point for infections;
- Breast trauma - leads to damage to breast tissue. This makes it difficult to release milk. Accumulated milk causes dry skin and pain on palpation. Blocked milk ducts can cause milk to leak into the breast tissue and cause further non-infectious inflammation called non-infectious mastitis. The skin over the inflamed area turns red and becomes hot to the touch. In this case, the body temperature may even rise to 40ºС.
If you take the necessary measures in time, relief can occur within 24 hours:
- determine the cause of milk stagnation and eliminate it;
- before attaching the baby, stimulate the oxytocin reflex as described above;
- pump the sore breast before feeding the baby, and then put him to the breast at the moment when he really wants to eat;
- try to put the baby on the sore breast as often as possible;
- change positions when breastfeeding. It is known that a baby sucks milk better from the part to which the lower lip faces.
Remember, treatment for a blocked duct is best done under the supervision of a doctor or breastfeeding specialist.
Chest pain during breastfeeding

Probably the most common problem that lactation specialists encounter is breast pain. Depending on the nature of the pain and its location, there can be a great variety of reasons. Let's look at the main ones.

If your nipple hurts, the most common reason is improper attachment to the breast. With a superficial latch, the baby injures the nipple with the gums, which leads to cracks, calluses and abrasions. The sensations during feeding are unpleasant and painful. The main way to solve this problem is to work on proper attachment and select comfortable positions for feeding.
If the pain in the nipples is accompanied by a burning sensation that remains between feedings, periodically painful shootings appear in the chest, and the areola and nipple turn red, then you may need to consult a doctor (dermatologist, gynecologist), since such unpleasant sensations may be symptoms of thrush.
Postpartum engorgement is another common reason why breasts may hurt during breastfeeding. The arrival of milk on days 3-5 can be quite noticeable for a woman - the breasts become full, sore, and may become red and hot. In this situation, it is important to put the baby to the breast frequently. If the baby is not comfortable sucking on the engorged breast, then you can first do a light massage and pump a little at the nipple so that the areola area becomes softer. Cold compresses after feedings will also help make the woman feel better. If the mother is unable to cope on her own, or the engorgement is too severe, you can always seek help from the maternity hospital staff or our breastfeeding specialists.
Unlike postpartum engorgement, which is physiological, lactostasis is usually provoked by some kind of flaws in the organization of breastfeeding. With lactostasis, the entire breast or some area may hurt. A fever often appears and the woman’s general condition resembles an illness. The most common causes of lactostasis are long breaks between feedings, ineffective emptying of the breast due to improper latching, injury, and unsuitable underwear. If lactostasis occurs, it is important not only to deal with it in a timely manner in order to prevent the development of mastitis, but also to determine its cause in order to avoid relapses. If you need help, our consultants are always in touch.
Flat or inverted nipple
Sometimes this becomes a reason for a woman’s anxiety and uncertainty about breastfeeding. Speaking about the importance of correctly attaching a baby to the breast, we pointed out that the baby should suck not from the nipple, but from the breast. That is, he needs to completely capture the areola. Therefore, in most cases, a flat nipple does not become an obstacle to latching on to the breast if the mother attaches the baby to the breast correctly.
It is very important to latch on to your baby correctly from day one, until the milk arrives and the breasts become firmer. You can experiment with baby positions at the breast, for example, try feeding in the “soccer ball” position, that is, from under your arm. Try stretching the nipple before feeding using a breast pump or syringe. During the sucking process, the baby will stretch the nipple more and more each time and adapt to the specifics of the mother's nipple. If, nevertheless, the child cannot suckle effectively within a week or two, then it is necessary to express milk and feed the child from a cup. At the same time, be patient and offer your baby the breast every time.
Insufficient milk supply
Let's first determine by what criteria we can say that the baby really does not have enough milk. Here are reliable signs of milk deficiency:
- infrequent urination of the child: less than 6-8 times per day;
- poor weight gain (less than 450-500 grams per month).
That's all! Neither frequent and prolonged feedings, nor the child's frequent crying, nor the child's refusal to suckle at the breast, nor the volume of milk “eaten” by the child at one time (control weighing), nor soft breasts are true signs of a lack of milk. If you find out for yourself that there is really little milk, then you need to find the real reason for the deficiency. And remember, there are many ways to improve lactation. Check yourself whether you are doing everything according to the rules of natural feeding. Because, most often, hypogalactia is caused precisely by factors associated with violation of these rules:
- Rare feedings.
- Incorrect attachment of the baby to the breast.
- No night feedings.
- Using pacifiers or pacifiers.
- Supplementation with water or additional feeding.
- Short feedings.
- Poor breast emptying with lactostasis.
- Incorrect introduction of complementary foods.
In these cases, there is only one piece of advice - correct all the mistakes, and the milk will not take long to arrive. It is possible that you will need professional help. In particular, if the amount of supplementary feeding is already quite large. But in any case, be patient and you will succeed! Some people advise the mother to eat and drink more, get more rest, or take medication to increase milk production. Understand that you can sleep around the clock and drink liters of lactation teas. But if you do not put your baby to your breast as expected, milk will not increase.
Remember, the main stimulator of lactation is the child.
Carry your baby in your arms more often, provide skin-to-skin contact, latch on to the breast more often and let the baby suckle as much as he wants, feed at night, take every opportunity for sleep and rest, drink so as not to feel thirsty and eat enough. Let someone else go to the store for groceries, and you can rest. After all, only you can give your baby the most valuable nutrition for him - breast milk. Sometimes, at the stage of the maternity hospital, delayed lactation is observed, due to severe stress, traumatic birth, fatigue and the mother’s lack of self-confidence. In such cases, the support of loved ones and medical personnel is very necessary. Taking certain medications (such as diuretics) can lead to milk deficiency. Consult your doctor and find an adequate replacement for this drug. Cases when a child really needs supplemental feeding are very rare. The volume and type of supplementary feeding must be selected individually, under the supervision of a doctor. But in any case, try to put your baby to your breast as often as possible, give milk replacer from a cup or spoon, and continue breastfeeding for as long as possible. After 6 months, with the gradual introduction of complementary foods, you will eliminate the milk replacer. The baby will eat purees, cereals and continue to breastfeed.
Why did my breasts become soft?
Soft breasts during feeding are normal and should not be alarmed. The leakage of milk and the feeling of fullness will subside over time. These signs are characteristic of the early stage of lactation, when the body has not yet decided how much milk the baby needs and gives it in excess.
This situation lasts for about 2 months. After all, the baby is still small, it is difficult for him to suckle, so the milk is nearby and practically pours into his mouth. This stage is called cumulative. Later, by 2 or 3 months, lactation changes tactics and becomes tidal: that is, milk is located in the posterior lobes and flows in when the baby latches on and begins to suck.
Therefore, it only seems that the breast is empty, but there is no less milk in it, this indicates that lactation has moved into a new phase and has become mature. The timing of this period is purely individual; for some, this time comes in the third month of lactation, for others, when the child turns 5 months old.
The feeling of fullness goes away completely, provided that there are no long breaks in feeding. But this should not be done, because the amount of milk secreted will definitely not increase. Some young mothers do not know this and begin to feed their baby formula, which helps reduce lactation.
If, when expressing with a breast pump, too little milk comes out, or no milk at all, this is also not an indicator of its absence. You will never be able to express the volume that your baby will suck.