The main method of primary diagnosis in vertebrology is radiography, magnetic resonance imaging (MRI) and computed tomography (CT) are used to clarify the diagnosis, as they are the most informative.
Using x-rays, the cause of pain and the nature of spinal damage are determined. This method is indispensable in emergencies and when first seeing a doctor. MRI makes it possible to obtain a spatial, detailed image of an organ. To decide whether it is better to perform an X-ray or an MRI of the spine for diagnostic purposes, you need to know what pathology needs to be excluded.
Principle of X-ray diagnostics
X-ray diagnostics in medicine is a study based on the work of electromagnetic ionizing radiation, which occurs with strong acceleration of charged particles and is characterized by high frequency and long wavelength. Using this examination method, images of three-dimensional objects with low density are obtained in two projections.
Radiography allows you to examine the internal structure using x-rays and special film. Passing through tissues of varying densities, the rays are scattered unevenly, and the resulting image of anatomical formations of varying degrees of intensity is recorded on film.
Basically, it is used to diagnose traumatic injuries of bones, spine, diseases of the lungs and paranasal sinuses. Modern devices record the image on a special film cassette or on an electronic matrix. The research time is limited to seconds.
Differences between CT and MRI of the spine
The main difference between diagnostic methods lies in the principle of their operation, hence the difference in results. In CT and MRI images, specialists see completely different things, although the same area is depicted. Let's take a closer look at how hardware research methods work:

MRI of the spine. The foundation of the operation of a tomographic MR installation is the generation of a high-frequency natural magnetic field. Once in the zone of influence of such a field, biological tissues begin to emit a resonating signature at the molecular level. The smallest particles of cells resonate with the magnetic field, which is detected by the equipment. These signals are processed by a computer program and transmitted to the monitor in the form of high quality and resolution images. MRI of the spine resonates best with particles that make up soft and dense tissues, as well as formations with a liquid substance in their composition (for example, the brain). The images clearly show muscles, tendons, cartilage, nerve fibers and the vascular network. The magnetic field does not have a damaging effect on the living fibers of the body, therefore, if necessary, the tomography procedure using nuclear resonance can be prescribed as many times as desired to a wide range of patients, including pregnant women and children from the first days of life.
CT scan of the spine. This type of scanning is the modern successor to classical radiography, since the operating principle of computer equipment is based on the use of ionizing radiation. Small doses of X-rays have the ability to penetrate any human tissue. The denser the tissue, the more clearly it is visible in the photographs, since adjacent soft and liquid fibers and substances transmit x-rays almost unhindered. Therefore, a CT scan of the spine shows bone structures much better and more clearly in photographic images. Also, the images show contrasting internal cavities filled with air or liquid. Since the human body is capable of accumulating radiation, the number of possible examinations using computer screening is possible no more than twice a year.
Principle of magnetic resonance imaging
Images of anatomical organs can be obtained using nuclear magnetic resonance. In this case, the object is placed in an area of high-intensity constant magnetic field. In such a field, with the help of electromagnetic waves, hydrogen atoms are influenced (the tissues of the body are saturated with it by 90%), under the influence of electromagnetic radiation, the protons of hydrogen atoms give a signal. The sensors measure the level of response of the cores by the energy released.
Tomographs collect this data and convert it into a three-dimensional, detailed image, recording it on electronic media and film. An MRI image of the spine allows you to examine bone structures, the structure of the spinal cord, intervertebral discs, cartilage and ligaments, and cerebrospinal fluid in three dimensions. MRI procedure time depends on the area being examined and can last up to 90 minutes.
How do MRI images differ from X-rays?
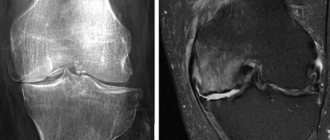
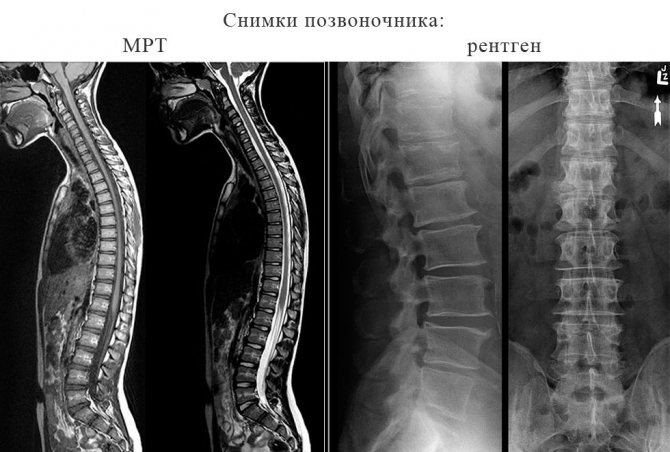
On MRI, black and white images provide a clear layer-by-layer image of the spine; they show the condition of the discs, cartilage tissue, spinal cord structures, nerve endings and soft tissues. Images are first taken in a plane dividing the human body into right and left halves.
If a pathology is found, this area is examined in two other planes - frontal (facing the camera) and transverse (as if cutting the body into parts in a horizontal plane). The spinal cord is best visualized with MRI on T1-VI: the structure, white and gray matter, cerebrospinal fluid, and bone marrow of the vertebral bodies are visible.
For a number of diseases, it is necessary to do magnetic resonance imaging with contrast: a paramagnetic contrast agent is injected intravenously, which is distributed throughout the vessels. The difference in blood supply and accumulation of contrast agent distinguishes healthy tissue from tumors and inflammation.
X-ray of the spine (spondylography) is performed in frontal, posterior and lateral projections, to display intervertebral joints - in oblique ones. You can receive pictures in 20-40 minutes. To determine the condition of the intervertebral discs, the examination is done during maximum flexion and extension of the spine, thus identifying the displacement of the overlying vertebrae relative to the underlying ones.
On spondylograms in the lateral projection, the spine is examined along its entire length: the vertebral bodies, their structure and shape, spinous processes, intervertebral discs, joints, and foramina. Using images, fractures and destructive changes in the vertebrae, inflammation and developmental anomalies, pathology of bone tissue are identified and the feasibility of MRI is determined.
What determines the choice of examination method?
Both diagnostic methods have their own indications for research. Damage to bones is best determined using radiography, soft tissue - MRI.
Indications for magnetic resonance imaging
This diagnostic method accurately determines the location, size, boundaries of neoplasms, foci of inflammation in the following pathologies of the spinal column:
- Traumatic injuries of the spine and spinal cord.
- Anomalies and malformations.
- Tumors of soft tissues, bone structures of the spine and spinal cord, metastases.
- Syringomyelia, multiple sclerosis.
- Vascular diseases of the spinal cord.
- Degenerative and dystrophic diseases of the spine.
- Spondylitis, epiduritis.
- Postoperative monitoring of the results of surgical treatment of diseases and injuries of the spine and spinal cord.
Indications for X-ray diagnostics
X-ray technology is a leader in the diagnosis of violations of the integrity of bone structures. But the use of this method is inappropriate in cases of damage to the soft tissues of the spine and spinal cord, as well as in young children due to its low information content.
- Spinal injuries.
- Osteomyelitis.
- Osteochondrosis.
- Osteoarthritis.
- Spondylosis.
- Curvature of the spine.
- Pain syndrome in the spine and limbs.
- Anomalies in the development of the spine.
- Herniated intervertebral discs.
- Suspicion of spinal tuberculosis.
Functional spondylography is performed for diseases such as spondylolisthesis (displacement of vertebral bodies). Pictures are taken with maximum flexion and extension of the spine in lateral projections. Despite the diagnostic value of both techniques, they cannot be used in some situations.
Possible contraindications for MRI and X-ray of the spine
There are conditions when the study threatens the patient’s life, in which case they speak of absolute contraindications for MRI. These include the presence of a pacemaker, metal clips on the blood vessels of the brain, implanted insulin pumps and artificial heart valves with metal elements. Also, people with artificial hip joints, osteosynthesis and hearing restoration devices, metal foreign objects in the body of any location, fragments, automatic drug dispensers are not allowed to undergo the examination.
If conditions create a danger or make it difficult to perform magnetic resonance imaging, they are called relative contraindications. The procedure is possible after comparing the risks and benefits for the patient. The list of relative contraindications includes: the presence of hemostatic staples in the human body (except for the brain), the first three months of pregnancy, severe heart failure, claustrophobia.
The presence in the body of surgical suture material, stents, artificial heart valves that do not contain ferromagnetic particles, and artificial metal teeth are not an obstacle to the study.
Contraindications for spondylography: pregnancy, severe conditions of patients with bleeding or open wounds of the chest.
CT
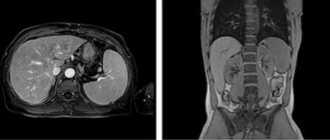
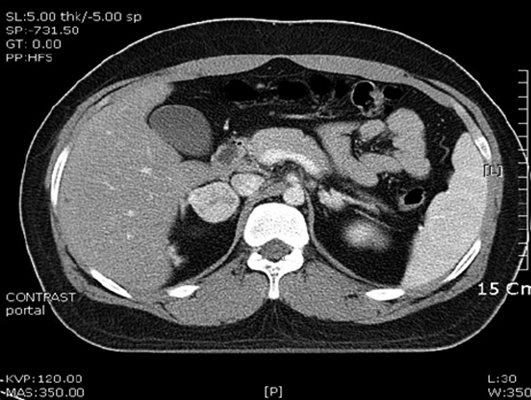
CT (computed tomography) is a method based on X-rays. It can be used to examine the adrenal glands and identify various types of pathologies, as well as neoplasms. Early diagnosis of adrenal diseases is quite important. They produce hormones. If the adrenal glands are removed without constant medical intervention and the use of hormonal drugs, a person faces death.
Indications for using this method are:
- Diagnosis of neoplasms.
- If tumors are present, determine the location and stage of development.
- Diagnosis of cysts.
- Determining the location of injury after an accident.
- Presence of metastases.
- Endocrine diseases.
CT scanning is contraindicated during pregnancy and breastfeeding. It is also not recommended for use in children under 12 years of age. In this case, the study is carried out only on an urgent basis. When performing a procedure with a contrast agent, the procedure is prohibited for patients with an allergy to iodine, hypothyroidism and bronchial asthma. CT scanning of the adrenal glands is not recommended more than once a year.
No special preparation is required for the study. Basically, the procedure is performed on an empty stomach. A few days before the CT scan, you should not consume gas-forming foods or alcohol.

During the procedure, doctors receive a three-dimensional image of the organ being examined. The photographs are taken in the form of sections. From here, the specialist can examine each piece of the organ and form an overall picture.
Diagnostic cost comparison
If you compare the cost of MRI and spondylography, preference may be given to x-ray diagnostics. Examination of all parts of the spine using a magnetic resonance imaging scanner can cost from 7,500 to 9,000 rubles, and individual parts - from 2,500 to 3,000 rubles.
The cost of radiography of the spine depends on the expected disease, the required number of images and projections. The average price ranges from 2500 to 3500 rubles. Each method has its own advantages and disadvantages.

Advantages and disadvantages of each method
When giving preference to one of the examination methods, you need to take into account the patient’s condition, the disease with which he applied, and whether he has the opportunity to conduct research. The advantage of radiography is that it is informative in cases of traumatic injuries of the spine.
| Advantages and disadvantages | MRI | Spondylography |
| Advantages | Safety for children and pregnant women | Availability and ease of diagnosis for most segments of the population |
| Allows you to examine soft tissues, vessels, organs in sections with an accuracy of 1mm | Information content for examining bone structures | |
| The study can be repeated without restrictions | Indispensable in emergency and primary diagnostics | |
| Allows you to get a three-dimensional image | It is possible to quickly make a linear image in several projections | |
| Flaws | The study is limited to a certain category of patients | Ionizing radiation is dangerous for the body; repeated studies are limited to previous radiation doses |
| Bone structures and stones are poorly visible due to low hydrogen content | Uninformative for diagnosing soft tissue pathology | |
| The appearance of artifacts at the slightest movement | X-rays travel only in one plane, motion errors are possible | |
| Long study duration | Contraindicated for children and pregnant women | |
| High cost and low availability |
Deciding whether X-ray or MRI of the spine is better, we can come to the conclusion that X-ray can be used in the initial stages of diagnosing lesions of the spinal column. The doctor must choose the examination method based on the official indications for a specific method.
In most cases, magnetic resonance imaging is used as an additional examination to clarify the diagnosis, the exact size and location of the pathological focus in the spine, spinal structures and soft tissues, with dynamic monitoring of the condition of patients after operations on these organs.
University
→ Home → University → University in the media → Tomogram or X-ray?
In the department of paid medical services, a woman makes an appointment for a spinal tomography. When the registrar asks to clarify the area of examination, he vaguely shrugs his shoulders: “I don’t know, let’s go to all departments”... The more accessible and informative methods of radiation diagnostics become, the more pressing the problem of their unreasonable prescription, including by patients to themselves. There are many common beliefs about X-rays, computed tomography (CT) and magnetic resonance imaging (MRI). Not all of them are true.
Where is the truth and where is the myth? - Kirill Senko, assistant at the Department of Radiation Diagnostics of the Belarusian State Medical University, radiologist at the Minsk City Clinical Emergency Hospital, explains.
Photo from the personal archive of K. Senko. Belief 1. X-ray is obsolete, it will be completely replaced by CT
The similarity of the techniques is only in the use of x-rays.
Traditional X-ray examination provides a planar image in a maximum of several projections, and CT provides a spatial image. In the latter case, a beam of X-rays passes through organs and structures, and sensors located on the side opposite the X-ray tube collect information and transmit it to a computer, which constructs axial (transverse) sections. A special program, if necessary, converts data in different planes. You can create frontal, sagittal, and 3D reconstructions, depending on your needs. Radiologists prefer transverse sections, because the remaining planes are “thought out” by the computer, which can cause errors (the so-called averaging effect).
There is no reason yet to believe that X-ray examination will become a thing of the past. The method is inexpensive and therefore widely used for both screening and confirmatory studies. Without its individual types (radiography, fluoroscopy and fluorography), it is difficult to imagine the primary stage of examination, when the task is to find out whether the patient has pathology of the lungs, mammary glands and other organs. Fluorographs today are available in almost every outpatient clinic, including in rural areas.
If a specific nosology is suspected, the radiation diagnostic method is chosen according to the principle from the simplest and least expensive to the more complex and expensive. For example, if it is necessary to exclude disease of the chest organs, they resort to fluorography. If there are doubts about the interpretation of the image, they are sent for radiography. When, even after this, ambiguities remain, CT will dot the i’s.
True, when diagnosing some ailments, CT is beginning to replace X-ray examination. So, previously, if a tumor of the pituitary gland was suspected, an X-ray of the sella turcica area was performed using special placements, but now it is prescribed, as a rule, only if it is not possible to urgently do a CT or MRI, and the result needs to be obtained quickly.
Belief 2. X-rays do not “see” diseases of the abdominal cavity well.
Right. Almost all organs of the abdominal cavity are not visualized on survey photographs without the administration of contrast agents. Only gross pathology can be considered, for example, perforation of a hollow organ (determined by the presence of free gas), acute intestinal obstruction, some types of foreign bodies and calculi.
After contrasting, the information content of an x-ray examination increases significantly.
Belief 3: CT is safer than radiography
The radiation dose per 1 slice in CT is less than per 1 projection in radiography. But the picture looks different if we compare studies of a specific organ or zone. So, with an X-ray of the head, only the bones of the skull are visualized, and the brain and other soft tissues are not visible. Radiation dose - 0.05 mSv. You can get only 2 projections - frontal and lateral.
CT allows you to visualize, in addition to bone structures, everything that is located inside the skull. There are more scans (from 80 to 100), and therefore the total radiation exposure is much higher - 0.4 mSv.
Belief 4. If it is possible to do a CT scan, x-ray techniques are neglected
In some cases, this approach can cause serious harm. Let's say a patient does a CT scan of the lungs instead of an annual fluorography, being confident that this thereby increases the chances of detecting pathology. As a result, a person receives radiation exposure tens of times greater than during a standard examination in a clinic.
Belief 5. MRI is the most accurate method of radiological diagnostics
This study is the method of choice (the most preferred) in diagnosing pathology of all types of soft tissues and blood vessels. A significant advantage over CT: to visualize veins and arteries, it is not necessary to administer iodinated contrast agents.
But an MRI will not provide useful information to a doctor about lung pathology. The parenchyma of this organ is airy, and only structures that contain hydrogen atoms are capable of reacting to magnetic nuclear resonance.
Unlike CT, MRI will not “see” acute hematoma, calcifications, or bone structures. The disease of the latter can be judged by MRI only by changes in nearby soft tissues or bone marrow.
Belief 6. In case of acute pathology, it is better to do a CT scan
Right. This is mainly due to the length of the process. Depending on the area and scope of the study, the CT procedure takes 10–30 seconds, and the MRI procedure takes 10–30 minutes. In urgent (life-threatening) situations, CT is used.
Belief 7. CT has more contraindications than MRI.
In fact, it's the opposite. Limitations when prescribing CT are related to radiation exposure, so it is not performed during pregnancy and lactation. Also, CT with contrast cannot be done for those who are allergic to iodine-containing drugs, acute and chronic renal failure, or severe diabetes. CT scans are performed for children with the consent and in the presence of parents and only in cases where the benefit of the study outweighs the risk.
The list of contraindications for MRI includes the presence of cardiac and neurostimulators, middle and inner ear implants, i.e. devices containing metal. Magnetic resonance can cause them to malfunction or even stop.
MRI is prohibited if there are hemostatic clips on the vessels of the brain. The diagnostic procedure should also be prescribed with caution to patients with hemostatic clamps on other organs. MRI is dangerous for patients with injuries and injuries in which there are ferromagnetic fragments in the eyeball, brain and soft tissues where blood vessels pass nearby. Foreign bodies can move and damage the walls of veins or arteries, which will result in massive bleeding.
MRI is not performed for those suffering from fear of closed spaces (claustrophobia) or mental illness; under alcohol or drug intoxication.
There are no scientific studies yet that would reveal the harm of MRI. Due to the possible (but unproven) negative impact, MRI is not performed on women in the 1st trimester of pregnancy, when the organs and systems of the fetus are developing.
Belief 8: If the patient is on life support (such as a ventilator), a CT or MRI will not be performed.
Yes and no. The limitations are, as a rule, due to the connection of various sensors, catheters, infusion systems... In most cases, it is physically impossible to place such a patient in an MRI machine (with the exception of open-type installations).
If life support equipment contains ferromagnetic elements (plastic, silicone, polyurethane, glass, etc.), then tomography will not be possible. Therefore, for intensive care patients, special life support devices are used, consisting only of materials that do not contain ferromagnets.
When performing CT scans, such problems do not arise, since X-ray radiation does not affect the operation of electromechanical equipment. The gantry aperture of a CT scanner is much shorter than that of a magnetic resonance imaging scanner, which means it is easier to connect the equipment to a person on life support.
Belief 9. Preparation before CT and MRI is not necessary
In most cases, yes. But if the abdominal and pelvic organs are examined, then a special diet and intestinal cleansing through enemas are necessary (the number and timing are determined based on the characteristics of the person’s constitution and the type of suspected pathology).
Before an MRI, the patient must remove all items containing ferromagnetic elements (watches, belts with buckles, jewelry, and clothing with zippers).
Tsifir. In 2010, in organizations subordinate to the Health Committee of the Minsk City Executive Committee, there were 10 CT and 2 MRI machines; in 2014 - 11 and 5, respectively. Elena Kleshchenok Photo from the personal archive of K. Senko Medical Bulletin , July 9, 2015