Modern medicine makes it possible to examine organs without interfering with their structure and without disrupting their function. In the same way, OCT of the eye makes it possible to non-contactly assess the condition of the layers of the retina, cornea of the eye and optic nerve fibers.
OCT is the scanning of eye tissue with an infrared beam of light. After light passes through the structure of the eye, the return signal is processed by mathematical analysis and converted into an image. The method allows you to assess the condition of the tissue with high resolution. Thus, the retina is analyzed at the level of layers consisting of its cells, the optic nerve - at the level of its fibers.
How is it carried out?
The procedure is similar to an ultrasound examination, but instead of an ultrasonic sensor, infrared optical radiation is used, the wavelength of which is about 1 micrometer. The main quantitative characteristics of tomographs for OCT are axial and transverse resolution, as well as the number of scans per second.
During scanning, the radiation of a beam of infrared rays is concentrated on the eye tissue: they are reflected from it, which is recorded by an interferometric modulator, which further processes the collected data. Two planes are captured: horizontal and vertical, and a cross-section of the area under study can be obtained. Upon completion of the operation of the device, the specialist clears the images of noise obtained during the study, interprets them and makes a diagnosis.
During OCT, the subject must remain absolutely still, especially the eyeball, otherwise the result will be distorted. To capture your gaze at the time of scanning, there is a video camera with a flashing object on it. A certain distance is set between the eye and the camera, which is 9 mm. If the patient is unable, for some reason, to fix his gaze on one point, then the study is not carried out, since the data will be uninformative. The procedure itself is carried out quickly and is not accompanied by any pain or discomfort.
No preparatory measures are required; ophthalmologists can only resort to dilating the pupil with medications: this is necessary in order to have the most accurate information about the anatomy of the posterior part of the visual organ. The subject must be warned that for several hours after using medications to dilate the pupil, he will have blurred vision, especially close up. Therefore, it is imperative to exclude driving and any activity that requires high concentration.
The cost of retinal OCT, despite its complexity, is affordable for almost every person. Therefore, this examination is increasingly recommended for a person to undergo in order to obtain a reliable and quick idea of the state of the organ of vision.
Methodology and aftercare
The technical aspects of OCT include the following steps. First, the patient's data is entered and the examination begins. In this case, the patient is asked to fix his gaze on a flickering object (in the lens of the fundus camera). Next, the camera is gradually brought closer to the eye until the image of the retina on the monitor becomes clear. The doctor fixes the camera at this distance using a special button and additionally adjusts the sharpness of the image. If visual acuity is low (when the patient cannot see a flickering object), external illumination should be used, and the patient should look straight ahead. Typically, the distance from the eye to the camera lens is 9 mm. OCT is carried out by scanning, this process is controlled using a control panel, which consists of six groups of buttons and manipulators with different functions.
After scanning, the images are aligned and cleared of noise. Based on the data obtained, tissue measurements and optical density analysis are carried out. Quantitative measurements can be compared with normal values that have been stored in the computer's memory.
What can you find?
There are two versions of tomographs - the first for viewing the anterior segment of the eye, and the other for the posterior segment. Modern devices make it possible to diagnose diseases of both poles at once.
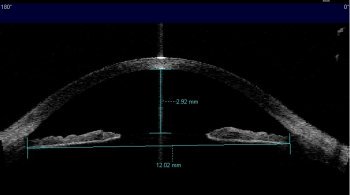
OKT of the anterior segment makes it possible to most thoroughly study the anatomical structure of the cornea: determine its thickness along its entire length, estimate the depth of the anterior chamber and its diameter, measure the chamber angle, its width. Such a study is widely used to assess the pre- and postoperative appearance of the iridociliary zone, since standard examinations do not bring the desired result. Anterior segment OKT sees corneal pathologies at the very beginning of their development, and the technology makes it possible to make a differential diagnosis between different types of glaucoma. There is only one situation that makes it difficult to carry out: when the patient has deep-set eyes.
Posterior tomography helps in detecting pathologies of the optic nerve, which transmits information from the inner lining of the eye to the brain. OCT is good because it can be performed an unlimited number of times to track the dynamics of the disease and the effectiveness of the treatment; infrared radiation is absolutely harmless to health.
Who is this examination intended for?
Patients undergo OCT, as a rule, for the diagnosis and treatment of diseases associated with pathology of the posterior segment of the eye such as:
- proliferative vitreoretinopathy (scarring of fibrous tissue)
- macular holes
- glaucoma
- retinal disinsertion
- all types of degenerative changes in the retina (including age-related)
- epiretinal membrane
- thrombosis of the central vein
- diabetic retinopathy
- cystoid macular edema
- abnormalities, swelling and atrophy of the optic nerve head
Advantages of OCT
Optical Coherence Tomography (OKT) allows you to obtain information about your visual health in the shortest possible time: you do not need to wait for your turn for several days or weeks; images along with interpretation can be obtained within 30 minutes. This is very significant in cases where immediate medical services are required (for example, for retinal diseases).
This method in medicine allows you to visualize the most microscopic structures and identify changes at the stage when they do not have any external symptoms. Timely diagnosis is considered the key to successful treatment, which is selected individually for each patient.
Retinal diseases vary in severity, and if untimely or poor-quality medical care is provided, they can lead to loss of vision. When performing OCT, the doctor receives an optimally complete picture, which cannot be obtained using other examination options. The accuracy of the result is affected by the equipment and its serviceability: the higher the quality of the equipment, the better the quality of the picture you can see in the end.
Optical coherence tomography of the retina was developed in the 1980s and since then the equipment and the method itself have been improved several times to improve the detection of vision problems. Gradually it became one of the most important diagnostic methods in ophthalmology.
Angio-OCT will soon be performed, but without contrast, as is still being done. Angio-OCT allows you to visualize the retinal arteries in more detail and assess blood flow - this is extremely important for hypertension, which entails damage to small vessels, for diabetic retinopathy, as well as for age-related maculopathy.
Optical coherence tomography in Moscow can be done in our clinic. The current price can be found in the corresponding section on the website.
Optical coherence tomography
- Physical basis of the method
- Indications for OCT
- OCT analysis and interpretation
- Fabric reflectivity
- Scan artifacts
- OCT of the anterior segment of the eye
- OCT retina
- OCT and histology
- Morphological analysis
OCT is a modern non-invasive, non-contact method that allows you to visualize various structures of the eye with higher resolution (from 1 to 15 microns) than ultrasound. OCT is a type of optical biopsy that does not require removal of a piece of tissue and its microscopic examination.
OCT is a reliable, informative, sensitive test (resolution is 3 µm) in the diagnosis of many fundus diseases. This non-invasive examination method, which does not require the use of a contrast agent, is preferred in many clinical cases. The resulting images can be analyzed, quantified, stored in a patient database, and compared with subsequent images, providing objective, documented information for disease diagnosis and monitoring.
For high-quality images, transparency of the optical media and normal tear film (or artificial tears) are required. The study is difficult with high myopia and clouding of the optical media at any level. Currently, scanning is performed within the posterior pole, but rapid advances in technology promise the possibility of scanning the entire retina in the near future.
The American ophthalmologist Carmen Puliafito first proposed the use of the concept of optical coherence tomography in ophthalmology in 1995. Later, in 1996-1997, the first device was introduced into clinical practice by Carl Zeiss Meditec. Currently, using these devices, it is possible to diagnose diseases of the fundus and anterior segment of the eye at the microscopic level.
Physical basis of the method
The examination is based on the fact that body tissues, depending on their structure, can reflect light waves differently. When it is carried out, the delay time of reflected light and its intensity after passing through the tissue of the eye are measured. Given the very high speed of the light wave, direct measurement of these indicators is impossible. For this purpose, tomographs use a Michelson interferometer.
A low-coherence beam of infrared light with a wavelength of 830 nm (for visualizing the retina) or 1310 nm (for diagnosing the anterior segment of the eye) is divided into two beams, one of which is directed to the tissues under study, and the other (control) to a special mirror. When reflected, both are perceived by the photodetector, forming an interference pattern. This, in turn, is analyzed by software, and the results are presented in the form of a pseudo-image, where, in accordance with a preset scale, areas with a high degree of light reflection are painted in “warm” (red) colors, with low ones - in “cold” up to black.
The layer of nerve fibers and pigment epithelium has a higher reflective ability, while the plexiform and nuclear layers of the retina have a medium reflective ability. The vitreous body is optically transparent and normally appears black on a tomogram. To obtain a three-dimensional image, scanning is carried out in the longitudinal and transverse directions. OCT can be complicated by the presence of corneal edema, clouding of optical media, and hemorrhages.
The optical coherence tomography method allows:
- visualize morphological changes in the retina and the layer of nerve fibers, as well as assess their thickness;
- assess the condition of the optic nerve head;
- examine the structures of the anterior segment of the eye and their relative spatial arrangement.
Indications for OCT
OCT is a completely painless and short-term procedure, but it gives excellent results. To conduct an examination, the patient needs to fixate his gaze on a special mark with the eye being examined, and if this is impossible, with the other eye that has better vision. The operator performs several scans and then selects the image with the best quality and information content.
When examining pathologies of the posterior part of the eye:
- degenerative changes in the retina (congenital and acquired, AMD)
- cystoid macular edema and macular hole
- retinal disinsertion
- epiretinal membrane
- changes in the optic nerve head (abnormalities, swelling, atrophy)
- diabetic retinopathy
- thrombosis of the central retinal vein
- proliferative vitreoretinopathy.
When examining pathologies of the anterior part of the eye:
- to assess the angle of the anterior chamber of the eye and the functioning of drainage systems in patients with glaucoma
- in case of deep keratitis and ulcers of the cornea
- during examination of the cornea during preparation and after laser vision correction and keratoplasty
- for control in patients with phakic IOLs or intrastromal rings.
When diagnosing diseases of the anterior part of the eye, OCT is used in the presence of ulcers and deep keratitis of the cornea, as well as in the case of diagnosing patients with glaucoma. OCT is also used to monitor the condition of the eyes after laser vision correction and immediately before it.
In addition, the optical coherence tomography method is widely used to study the posterior part of the eye for the presence of various pathologies, including retinal detachment or degenerative changes, diabetic retinopathy, as well as a number of other diseases
OCT analysis and interpretation
The application of the classical Cartesian method to OCT image analysis is not uncontroversial. Indeed, the resulting images are so complex and varied that they cannot be considered simply as a problem solved by the sorting method. When analyzing a tomographic image, consideration should be given to
- cut shape,
- thickness and volume of tissue (morphological features),
- internal architectonics (structural features),
- the relationship of zones of high, medium and low reflectivity with both the internal structure and tissue morphology features,
- the presence of abnormal formations (fluid accumulation, exudate, hemorrhage, neoplasms, etc.).
Pathological elements can have different reflectivity and form shadows, which further changes the appearance of the image. In addition, disturbances in the internal structure and morphology of the retina in various diseases create certain difficulties in recognizing the nature of the pathological process. All this complicates any attempt at automatic image sorting. At the same time, manual sorting is also not always reliable and carries a risk of errors.
OCT image analysis consists of three basic steps:
- morphology analysis,
- analysis of the structure of the retina and choroid,
- reflectivity analysis.
It is better to study scans in detail in black and white rather than in color. The shades of color OCT images are specified by the system software, each shade is associated with a certain degree of reflectivity. Therefore, in a color image we see a wide variety of color shades, while in reality there is a consistent change in the reflectivity of the fabric. A black-and-white image allows you to identify minimal variations in tissue optical density and see details that may go unnoticed in a color image. Some structures may be better visible on negative images.
Morphological analysis includes examination of the slice shape, vitreoretinal and retinochoroidal profiles, as well as the chorioscleral profile. The volume of the studied area of the retina and choroid is also assessed. The retina and choroid lining the sclera have a concave parabolic shape. The fovea is a depression surrounded by an area thickened due to the displacement of the nuclei of ganglion cells and cells of the inner nuclear layer here. The posterior hyaloid membrane has the densest adhesion along the edge of the optic disc and in the fovea (in young people). The density of this contact decreases with age.
The retina and choroid have a special organization and consist of several parallel layers. In addition to parallel layers, the retina has transversal structures that connect different layers.
Normally, the retinal capillaries, with their specific organization of cells and capillary fibers, represent true barriers to fluid diffusion. Vertical (cell chains) and horizontal structures of the retina explain the location, size and shape of pathological accumulations (exudate, hemorrhages and cystic cavities) in the retinal tissue, which are detected on OCT.
Anatomical barriers vertically and horizontally prevent the spread of pathological processes.
- Vertical elements - Müller cells connect the inner limiting membrane to the outer limiting membrane, extending through the layers of the retina. In addition, the vertical structures of the retina include cellular chains, which consist of photoreceptors associated with bipolar cells, which, in turn, contact ganglion cells.
- Horizontal elements: layers of the retina - The inner and outer limiting membranes are formed by Müller cell fibers and are easily recognized in a histological section of the retina. The inner and outer plexiform layers contain horizontal, amacrine cells and a synaptic network between photoreceptors and bipolar cells on one side and bipolar and ganglion cells on the other. From a histological point of view, the plexiform layers are not membranes, but to some extent function as a barrier, although much less durable than the inner and outer limiting membranes. Plexiform layers include a complex network of fibers that form horizontal barriers to fluid diffusion across the retina. The inner plexiform layer is more resistant and less permeable than the outer one. In the foveal region, Henle's fibers form a sun-like structure that can be clearly seen on the frontal section of the retina. The cones are located in the center and are surrounded by the nuclei of photoreceptor cells. Henle's fibers connect the cone nuclei to the bipolar cell nuclei at the periphery of the fovea. In the fovea region, Müller cells are oriented diagonally, connecting the inner and outer limiting membranes. Due to the special architecture of Henle fibers, the accumulation of fluid in cystoid macular edema has the shape of a flower.
Image segmentation
The retina and choroid are formed by layered structures with varying reflectivity. The segmentation technique makes it possible to identify individual layers of homogeneous reflectivity, both high and low. Image segmentation also makes it possible to recognize groups of layers. In cases of pathology, the layered structure of the retina may be disrupted.
The retina is divided into outer and inner layers (outer and inner retina).
- The inner retina includes a layer of nerve fibers, ganglion cells, and an inner plexiform layer, which serves as the boundary between the inner and outer retina.
- Outer retina - inner nuclear layer, outer plexiform layer, outer nuclear layer, outer limiting membrane, line of articulation of outer and inner segments of photoreceptors.
Many modern tomographs allow segmentation of individual retinal layers and identification of the most interesting structures. The automatic nerve fiber layer segmentation function was the first of its kind to be introduced into the software of all tomographs, and remains central to the diagnosis and monitoring of glaucoma.
Fabric reflectivity
The intensity of the signal reflected from the tissue depends on the optical density and the ability of the tissue to absorb light. Reflectivity depends on:
- the amount of light reaching a given layer after absorption in the tissues through which it passes;
- the amount of light reflected by a given fabric;
- the amount of reflected light reaching the detector after further absorption by the tissues through which it passes.
Normal structure (reflectivity of normal tissues)
- High Nerve fiber layer
- Line of articulation of the outer and inner segments of photoreceptors
- External limiting membrane
- Pigment epithelium-choriocapillaris complex
- Plexiform layers
- Nuclear layers
Vertical structures, such as photoreceptors, are less reflective than horizontal structures (eg, nerve fibers and plexiform layers). Low reflectivity can be caused by a decrease in the reflectivity of the tissue due to atrophic changes, the predominance of vertical structures (photoreceptors) and cavities with liquid contents. Structures with low reflectivity can be observed especially clearly on tomograms in cases of pathology.
Choroidal vessels are hyporeflective. The reflectivity of choroidal connective tissue is assessed as average, sometimes it can be high. The dark plate of the sclera (lamina fusca) looks like a thin line on tomograms; the suprachoroidal space is not normally visualized. Typically the choroid is about 300 microns thick. With age, starting from the age of 30, there is a gradual decrease in its thickness. In addition, the choroid is thinner in patients with myopia.
Low reflexivity (fluid accumulation):
- Intraretinal fluid accumulation: retinal edema. Diffuse edema (diameter of intraretinal cavities less than 50 µm) and cystic edema (diameter of intraretinal cavities more than 50 µm) are distinguished. To describe intraretinal fluid accumulation, the terms “cysts”, “microcysts”, “pseudocysts” are used.
- Subretinal fluid accumulation: serous detachment of the neuroepithelium. The tomogram reveals elevation of the neuroepithelium at the level of the tips of rods and cones with an optically empty space under the elevation zone. The angle of the detached neuroepithelium with the pigment epithelium is less than 30 degrees. Serous detachment can be idiopathic, associated with acute or chronic CSC, and also accompany the development of choroidal neovascularization. Less commonly found in angioid streaks, choroiditis, choroidal neoplasms, etc.
- Subpigment fluid accumulation: detachment of the pigment epithelium. Elevation of the pigment epithelium layer above Bruch's membrane is detected. The source of fluid is the choriocapillaris. Often the detachment of the pigment epithelium forms an angle of 70-90 degrees with Bruch's membrane, but always exceeds 45 degrees.
Scan artifacts
They can have a negative impact on both the qualitative analysis and the quantitative assessment of the study. They arise as a result of research errors, patient behavior, or device software errors.
- Inversion artifact (mirror artifact) - occurs when the scanned area extends beyond the so-called zero delay line of the device, as a result of which an inverted or partially inverted image with a decrease in signal is visualized in the images. It is observed if the device is located too close to the eye or with pathological changes such as high myopia, retinoschisis and asteroid hyalosis.
- Vignetting occurs when the shadow of the iris falls on any side of the image; you can avoid this artifact by simply moving a little further from the edge of the iris while performing the study.
- Averaging artifact - occurs as a result of the superposition of another scanning area on the resulting scan image (due to the movement of the patient's gaze during scanning), typical for high-resolution scans.
- Motion and blinking artifacts are visualized as a lack of signal, intermittent scans, or black stripes.
- Artifacts of floating opacities - lead to a decrease in signal quality; it is necessary to ask the patient to move their gaze in different directions to try to remove the opacification from the beam movement area.
- Alignment error - occurs at the time of analysis when the software does not correctly align images to anatomical landmarks. If in other aspects the research is carried out qualitatively, you can simply shift the template of the analysis zone.
- Segmentation error - is associated with a device error when selecting and lining up the lines between which the parameters are calculated.
- Out-of-order error - associated with the location of the device (close/far from the eye), as a result of which some part of the image (retina or choroid) falls out of the scanning area.
OCT of the anterior segment of the eye
Optical coherence tomography (OCT) of the anterior segment of the eye is a non-contact technique that creates high-resolution images of the anterior segment of the eye, superior to the capabilities of ultrasound devices.
OCT can accurately measure the thickness of the cornea (pachymetry) along its entire length, the depth of the anterior chamber of the eye at any segment of interest, measure the internal diameter of the anterior chamber, and also accurately determine the profile of the anterior chamber angle and measure its width.
The method is informative when analyzing the state of the anterior chamber angle in patients with a short anteroposterior axis of the eye and large lens sizes, in order to determine indications for surgical treatment, as well as to determine the effectiveness of cataract extraction in patients with a narrow APC.
Also, anterior segment OCT can be extremely useful for anatomical assessment of the results of glaucoma surgery and visualization of drainage devices implanted during surgery.
Scan Modes
- allowing to obtain 1 panoramic image of the anterior segment of the eye in a selected meridian
- allowing to obtain 2 or 4 panoramic images of the anterior segment of the eye in 2 or 4 selected meridians
- allowing to obtain one panoramic image of the anterior segment of the eye with higher resolution compared to the previous one
When analyzing images, you can perform
- qualitative assessment of the condition of the anterior segment of the eye as a whole,
- identify pathological foci in the cornea, iris, angle of the anterior chamber,
- analysis of the surgical area for keratoplasty in the early postoperative period,
- assess the position of the lens and intraocular implants (IOLs, drains),
- measure corneal thickness, anterior chamber depth, anterior chamber angle
- measure the size of pathological lesions - both relative to the limbus and relative to the anatomical formations of the cornea itself (epithelium, stroma, Descimet's membrane).
For superficial pathological foci of the cornea, light biomicroscopy is undoubtedly highly effective, but if the transparency of the cornea is impaired, OCT will provide additional information.
For example, with chronic recurrent keratitis, the cornea becomes unevenly thickened, the structure is heterogeneous with foci of compaction, it acquires an irregular multilayer structure with a slit-like space between the layers. In the lumen of the anterior chamber, network-like inclusions (fibrin threads) are visualized.
Of particular importance is the possibility of non-contact visualization of the structures of the anterior segment of the eye in patients with destructive-inflammatory diseases of the cornea. With long-term keratitis, destruction of the stroma often occurs from the endothelium. Thus, a lesion in the anterior parts of the corneal stroma, clearly visible during biomicroscopy, can mask the destruction occurring in the deep layers.
OCT retina
OCT and histology
Using the high resolution of OCT, it is possible to assess the state of the retinal periphery in vivo: to record the size of the pathological lesion, its location and structure, the depth of the lesion, and the presence of vitreoretinal traction. This makes it possible to more accurately determine the indications for treatment, and also helps to document the results of laser and surgical operations and monitor long-term results. To correctly interpret OCT images, it is necessary to have a good understanding of the histology of the retina and choroid, although tomographic and histological structures cannot always be accurately compared.
In fact, due to the increased optical density of some retinal structures, the line of articulation of the outer and inner segments of the photoreceptors, the line of connection of the tips of the outer segments of the photoreceptors and the villi of the pigment epithelium are clearly visible on the tomogram, while they are not differentiated on the histological section.
On the tomogram you can see the vitreous body, the posterior hyaloid membrane, normal and pathological vitreal structures (membranes, including those that have a traction effect on the retina).
- Inner Retina The inner plexiform layer, the ganglion or multipolar cell layer, and the nerve fiber layer form the ganglion cell complex or inner retina. The internal limiting membrane is a thin membrane formed by the processes of Müller cells and adjacent to the nerve fiber layer. The layer of nerve fibers is formed by processes of ganglion cells that extend to the optic nerve. Since this layer is formed by horizontal structures, it has increased reflectivity. The layer of ganglion, or multipolar, cells consists of very voluminous cells. The inner plexiform layer is formed by the processes of nerve cells; synapses of bipolar and ganglion cells are located here. Thanks to the many horizontally running fibers, this layer has increased reflectivity on tomograms and distinguishes the inner and outer retina./
- Outer retina The inner nuclear layer contains the nuclei of bipolar and horizontal cells and the nuclei of Müller cells. On tomograms he is hyporeflective. The outer plexiform layer contains synapses of photoreceptor and bipolar cells, as well as horizontally located axons of horizontal cells. On OCT scans it has increased reflectivity.
Photoreceptors, cones and rods
The layer of photoreceptor cell nuclei forms the outer nuclear layer, which forms the hyporeflective stripe. In the fovea area, this layer thickens significantly. The photoreceptor cell bodies are somewhat elongated. The nucleus almost completely fills the cell body. The protoplasm forms a conical protrusion at the apex, which contacts the bipolar cells.
The outer part of the photoreceptor cell is divided into inner and outer segments. The latter is short, conical in shape and includes discs stacked in successive rows. The inner segment is also divided into two parts: the inner myodal and outer filament.
The line of articulation between the outer and inner segments of the photoreceptors on the tomogram looks like a hyperreflective horizontal strip located at a short distance from the pigment epithelium-choriocapillaris complex, parallel to the latter. Due to the spatial increase in cones in the foveal zone, this line is somewhat removed at the level of the fovea from the hyperreflective stripe corresponding to the pigment epithelium.
The external limiting membrane is formed by a network of fibers coming mainly from Müller cells that surround the bases of photoreceptor cells. The external limiting membrane on the tomogram appears as a thin line located parallel to the line of articulation of the outer and inner segments of the photoreceptors.
Supporting structures of the retina
Müller cell fibers form long, vertically arranged structures that connect the inner and outer limiting membranes and perform a supportive function. The nuclei of Müller cells are located in the layer of bipolar cells. At the level of the outer and inner limiting membranes, the Müller cell fibers diverge in the form of a fan. The horizontal branches of these cells are part of the structure of the plexiform layers.
Other important vertical elements of the retina include chains of cells consisting of photoreceptors connected to bipolar cells and through them to ganglion cells, whose axons form a layer of nerve fibers.
The pigment epithelium is represented by a layer of polygonal cells, the inner surface of which is cup-shaped and forms villi that come into contact with the tips of the cones and rods. The nucleus is located in the outer part of the cell. Externally, the pigment cell is in close contact with Bruch's membrane. On high-resolution OCT scans, the line of the pigment epithelium-choriocapillaris complex consists of three parallel stripes: two relatively wide hyperreflective stripes, separated by a thin hyporeflective stripe.
Some authors believe that the inner hyperreflective stripe is the line of contact between the villi of the pigment epithelium and the outer segments of the photoreceptors, and the other, the outer stripe, represents the cell bodies of the pigment epithelium with their nuclei, Bruch's membrane and choriocapillaris. According to other authors, the inner stripe corresponds to the tips of the outer segments of the photoreceptors.
The pigment epithelium, Bruch's membrane and choriocapillaris are closely interconnected. Typically, Bruch's membrane is not differentiated on OCT, but in cases of drusen and small detachment of the pigment epithelium, it is defined as a thin horizontal line.
The choriocapillaris layer is represented by polygonal vascular lobules, which receive blood from the posterior short ciliary arteries and conduct it through venules into the vorticose veins. On the tomogram, this layer is part of a wide line of the pigment epithelium complex - choriocapillaris. The main choroidal vessels on the tomogram are hyporeflective and can be distinguished in the form of two layers: the layer of medium vessels of Sattler and the layer of large vessels of Haller. From the outside, you can visualize the dark plate of the sclera (lamina fusca). The suprachoroidal space separates the choroid from the sclera.
Morphological analysis
Morphological analysis includes determining the shape and quantitative parameters of the retina and choroid, as well as their individual parts.
General retinal deformation
- Concave deformation (concave deformation): in case of high myopia, posterior staphyloma, including cases of scleritis, a pronounced concave deformation of the resulting slice can be detected on OCT.
- Convex deformity (convex deformity): occurs in the case of a dome-shaped detachment of the pigment epithelium, and can also be caused by a subretinal cyst or tumor. In the latter case, the convex deformation is flatter and involves the subretinal layers (pigment epithelium and choriocapillaris).
In most cases, the tumor itself cannot be localized on OCT. Edema and other changes in the adjacent neurosensory retina are important in the differential diagnosis.
Retinal profile and surface deformation
- The disappearance of the fovea indicates the presence of retinal edema.
- Retinal folds, which form as a result of tension from the epiretinal membrane, are visualized on tomograms as irregularities in its surface, resembling “waves” or “ripples”.
- The epiretinal membrane itself can differentiate as a separate line on the surface of the retina, or merge with the layer of nerve fibers.
- Tractional deformation of the retina (sometimes star-shaped) is clearly visible on C-scans.
- Horizontal or vertical traction from the epiretinal membrane deforms the surface of the retina, leading in some cases to the formation of a central tear. Macular pseudohole: the fovea is widened, the retinal tissue is preserved, although deformed.
- Lamellar tear: the fovea is enlarged due to the loss of part of the inner retinal layers. Above the pigment epithelium, the retinal tissue is partially preserved.
- Macular hole: OCT allows you to diagnose, classify macular hole and measure its diameter.
According to the Gass classification, there are 4 stages of macular hole:
- Stage I: detachment of the neuroepithelium of traction origin in the fovea;
- Stage II: through defect of retinal tissue in the center with a diameter of less than 400 microns;
- Stage III: a through defect of all layers of the retina in the center with a diameter of more than 400 microns;
- Stage IV: complete detachment of the posterior hyaloid membrane, regardless of the size of the through defect in the retinal tissue.
Tomograms often reveal swelling and slight detachment of the neuroepithelium at the edges of the tear. Correct interpretation of the rupture stage is possible only when the scanning beam passes through the center of the rupture. When scanning the edge of a rupture, erroneous diagnosis of a pseudofracture or an earlier stage of rupture is possible.
The layer of pigment epithelium may be thinned, thickened, and in some cases it may have an irregular structure throughout the scan. The bands corresponding to the pigment cell layer may appear abnormally saturated or disorganized. In addition, the three stripes can merge together.
Retinal drusen cause the appearance of irregularity and wave-like deformation of the pigment epithelium line, and Bruch's membrane in such cases is visualized as a separate thin line.
Serous detachment of the pigment epithelium deforms the neuroepithelium and forms an angle of more than 45 degrees with the choriocapillaris layer. In contrast, serous detachment of the neuroepithelium is usually flatter and forms an angle equal to or less than 30 degrees with the pigment epithelium. Bruch's membrane is differentiated in such cases.
Interpretation
The diagnosis is always based on expert analysis of scanograms obtained from OCT. In this case, the doctor pays attention to the morphological indicators of tissues (the relationship of layers and sections, changes in the external contour, relationship with neighboring tissue structures), changes in light reflectivity (decrease or increase in transparency, the presence of pathological inclusions). With quantitative data analysis, you can see changes in the thickness of the cell layer (thinning, thickening), the volume of the structure being studied, and also obtain a surface map.