In connection with the coronavirus epidemic, the editors of the Medical Channel decided to direct all their efforts to combat this threat. We translate the latest and best scientific journal articles on COVID-19 because we believe that knowledge is the best weapon. If you want to support our editorial staff to produce as many translations as possible, then you can make a donation through Yandex or subscribe to our Patreon. We will be very grateful for your help; all funds raised will go to pay for the work of translators, editors and illustrators. Yandex: https://yasobe.ru/na/medach
Patreon: https://www.patreon.com/medach
In this retrospective case series, chest CT scans of 21 symptomatic Chinese patients infected with the 2021 novel coronavirus (2019-nCoV) were analyzed; emphasis was placed on identifying and characterizing the most common symptoms.
Typical CT findings included bilateral ground-glass opacities of the lung parenchyma and areas of consolidation that were sometimes round in shape and extended to the peripheral lungs. Notably, pulmonary cavitation, solitary nodules, pleural effusion, and lymphadenopathy were absent. With further CT monitoring in this group of patients during the study, mild or moderate progression of changes was often revealed, which was manifested in an increase in the degree and density of areas of compaction of the lung tissue.
The 2021 novel coronavirus infection exhibits characteristic features on chest CT scans that assist the radiologist in early detection and diagnosis of this new global health emergency.
- Of the 21 patients with 2019-nCoV infection, 15 (71%) had lesions of more than two lobes on chest CT, 12 (57%) had ground-glass consolidations, seven (33%) had round-shaped consolidations, seven (33%) had peripheral distribution, six (29%) had foci of both consolidation and ground-glass consolidation, and four (19%) had a crazy-paving pattern.
- There were no pulmonary cavitations, solitary pulmonary nodules, pleural effusions, or lymphadenopathy.
- Fourteen percent of patients (three of 21) were normal on computed tomography.
On 31 December 2021, the World Health Organization (WHO) was notified of several cases of a respiratory illness of unknown origin detected in Wuhan City, Hubei Province, China, with clinical manifestations resembling those of viral pneumonia, including fever, cough and shortness of breath. As of January 30, 2021, WHO has designated this outbreak as a global health emergency. Chest x-rays often showed lung opacities in patients. By January 3, 2021, 44 patients with this disease of unknown etiology had been reported to WHO, with a preliminary epidemiological investigation showing that most patients worked or were frequent visitors to the Huanan Seafood Wholesale Market [1]. Analysis of bronchoalveolar lavage fluid samples and electron microscopy revealed that the causative agent is a coronavirus, with its characteristic ultrastructural morphology on electron microscopy due to the presence of spiny appendages emanating from the viral envelope, reminiscent of a crown appearance.
The discovered virus was temporarily named 2019 novel coronavirus (2019-nCoV). Coronaviruses belong to the family Coronaviridae, order Nidovarales, and a family that includes viruses that cause diseases ranging from the common cold to severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS) [2]. The SARS outbreak began in southern China and was recognized as a global public health threat in March 2003, resulting in the deaths of 774 of 8098 people infected from November 2002 to July 2003 [3]. MERS was first reported in 2012 in Saudi Arabia, and to date there have been 858 deaths among 2,494 infections [4].
As of January 28, 2021, there are 4,593 confirmed cases of the disease worldwide. Of these, 4,537 are in China and 56 are from 14 other countries. In addition, another 6,973 cases are suspected in China. As of January 28, 2021, there have been 106 deaths, all in China [5]. On January 30, 2021, the WHO declared the Chinese coronavirus a global health emergency. An initial prospective analysis of clinical data from 41 initially admitted Wuhan patients with laboratory-confirmed 2019-nCoV found that 2019-nCoV caused severe disease clinically similar to SARS, sometimes resulting in the need for intensive care unit admission (13 of 41 [32% ]) and death (6 of 41 [15%]). All patients with pneumonia in this study had changes on chest computed tomography: preliminary reports indicated that there were bilateral lung parenchymal consolidations in all patients [6].
In this article, we describe and characterize the key CT features found in a cohort of 21 patients infected with 2019-nCoV in China to familiarize radiologists and other members of clinical teams with the radiographic manifestations of this new disease. Early recognition of the disease can expedite treatment and ensure early isolation of the patient, and will allow for early surveillance, containment and public health response to this infectious disease.
Patients and chest CT
Our institutional review board waived the requirement to obtain written informed consent for the retrospective analysis of this case series, which assessed de-identified data and did not anticipate potential risk to patients. To prevent possible breaches of confidentiality, communications between patients and researchers were not available.
Between January 18, 2021 and January 27, 2021, 21 patients with confirmed 2019-nCoV infection were admitted to three hospitals in three provinces in China; All had a chest CT scan. Ten patients from Zhuhai (Guangdong Province) underwent tomography with 1-mm slices using a UCT 760 scanner (United Imaging, Shanghai, China). Nine patients from Nanchang (Jiangxi Province) underwent tomography with 8 mm thick slices using an Emotion 16 scanner (Siemens Healthineers, Erlangen, Germany). Two patients were from Qingdao (Shandong Province) and were examined with a 5 mm slice thickness, one using a BrightSpeed scanner (GE Medical Systems, Milwaukee, WS) and one using an Aquilion ONE scanner (Toshiba Medical Systems, Tokyo, Japan) . All studies were carried out with the patient in the supine position at the height of inspiration, without the introduction of a contrast agent. All patients had confirmed 2019-nCov infection by laboratory testing of bronchoalveolar lavage fluid, endotracheal aspirate, nasopharyngeal swab, or oropharyngeal swab.
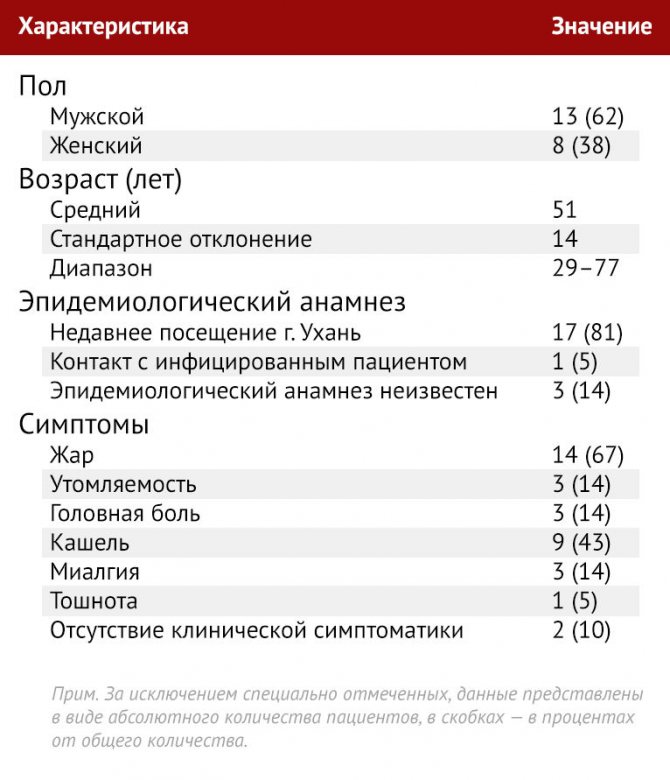
Patient selection for this study was continuous at each of the three institutions, and no exclusion criteria were applied (Table 1). In addition to information on age and sex, clinical information collected included data on the severity and course of symptoms, as well as epidemiological history, including information about the patients' travel history.
Table 1 | General patient data (n = 21)
Principle of operation
The basis of CT is the ability of tissues to absorb X-rays differently, and the image is obtained from certain sections. Detailed information can be obtained using a sensitive matrix and special sensors inside the device, as well as automatic saving and conversion of data into digital format.
Tomographs of the twenty-first century consist of electronic and mechanical components. X-rays passing through the internal structures of the body are recorded using high-sensitivity detectors. The latter are constantly being modernized, each manufacturer of medical equipment offers its own developments.
The key to the effective functioning of the device is software that allows you to:
- perform research with the required parameters;
- process and transform information;
- analyze the received data.
Analysis of CT studies
Each CT examination was reviewed by two radiologists trained in cardiothoracic radiology with approximately 5 years of experience each (MC and AB) using a viewing console. The studies were reviewed independently and the final results were based on consensus. If there was a disagreement between the two main interpretations, a third board-certified cardiothoracic radiologist with 10 years of experience made the final decision. Negative controls and blinding were not used.
For each of the 21 patients, the initial CT scans were assessed for the following characteristics: (a) presence of ground-glass opacities, (b) presence of consolidation, (c) number of lobes, per which spread ground glass compactions and areas of consolidation, (d) the degree of lobe damage in addition to the general “scale of severity of lung damage”, (e) the presence of nodules, (f) the presence of pleural effusion, (g) the presence of thoracic lymphadenopathy (defined as lymph node size ≥10 mm in short axis measurement) and (h) the presence of an underlying lower respiratory tract disease such as emphysema or fibrosis. Other CT findings such as cavitation, reticulation, interlobular septal thickening, calcifications, and bronchiectasis were also noted.
Ground-glass opacification was defined as an increase in the density of the lung tissue in the form of a haze with preservation of visualization of the edges of the bronchi and vessels, and consolidation was defined as an increase in the density of the lung tissue with darkening of the edges of the vessels and walls of the airways [7]. Each of the five lung lobes was scored for degree of involvement and classified as none (0%), minimal (1–25%), mild (26–50%), moderate (51–75%), or severe (76–100%). Lack of involvement corresponded to 0 points, minimal involvement - 1 point, mild involvement - 2 points, moderate involvement - 3 points, and severe involvement - 4 points.
The result on the overall “lung severity scale” was formed by summing the scores from each of the five lobes of the lung (possible score range 0–20). Eight patients underwent follow-up chest CT scans during the study. These scans were also assessed for change or progression over time, which was qualitatively assessed using a consensus approach by two radiologists (MC and AB).
The study included 13 men and 8 women with an age range of 29–77 years; mean age ± standard deviation, 51 years ± 14.
When can a doctor refer you for a CT scan?
Due to its information content, accuracy and safety, the method has become widespread. The doctor can prescribe a study:
- During a routine examination after undergoing ultrasound diagnostics, X-rays, tests, etc. The results are used to rule out errors in diagnosis.
- If you have symptoms of various diseases. Reasons for referral for scanning may include headaches, injuries without loss of consciousness, fainting, and manifestations of lung cancer.
- If there is a need to provide emergency medical care to a patient. This happens with a history of cancer, fever, development of convulsive syndrome, serious skull injuries, suspicion of dissecting aortic aneurysm, acute lesions of parenchymal organs, organic brain damage, etc.
- To monitor how patients are being treated and whether adjustments to the treatment plan are required.
Before surgery to clarify the parameters of tumors, the affected area, the location of blood vessels and obtain other information necessary for the safe performance of surgical procedures.
Ground glass seals and consolidation
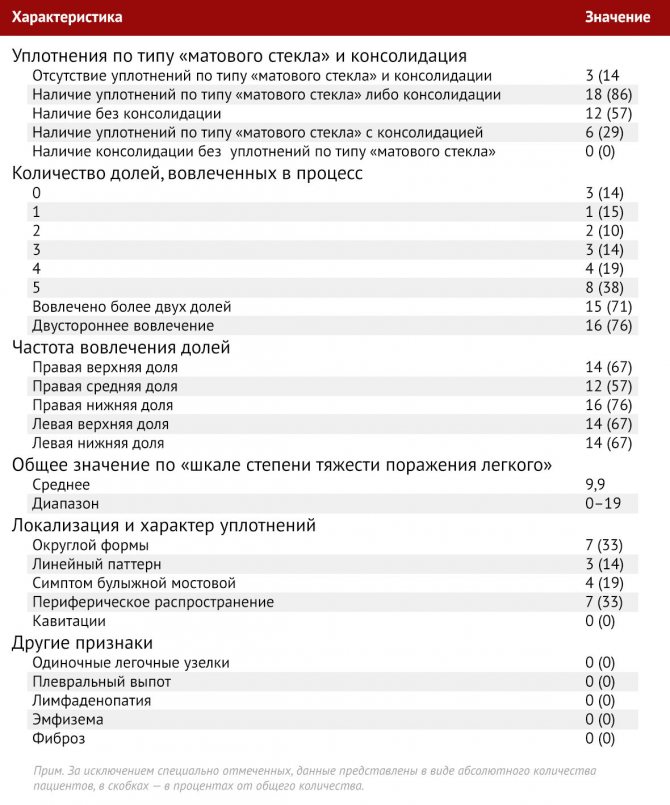
Of the 21 initial CT examinations, three (14%) patients did not demonstrate ground-glass opacities; in fact, these three patients had no CT evidence of chest pathology on admission (Table 2). Of the 18 patients in whom areas of ground-glass consolidation or consolidation were visualized, only ground-glass consolidation was observed in 12 (without consolidation). Not a single patient had areas of consolidation of lung tissue without the presence of ground glass compaction.
Table 2 | CT signs detected in 21 patients during the initial examination
The importance of timely examination
Coronavirus infection is dangerous due to complications. A person may not realize that he is developing bilateral pneumonia, since the clinical symptoms are vague or completely absent. Therefore, timely laboratory and instrumental tests are required to help the doctor identify the diagnosis and begin treatment.
The reliability of tomography is more than 90%, the effectiveness of radiography is much lower.
Doctors advise using laboratory tests to determine the degree of complications of covid-19. If the patient is at risk and has developed clinical symptoms, a CT scan is always required. It can be used to select an antibiotic.

For mild pneumonia, a less aggressive drug is used than for severe pneumonia. If the doctor detects CT2, he will explain what this means for coronavirus and what medications to use to prevent further progression of the pathology. To eliminate the risk of residual infection that cannot be heard with a phonendoscope, it is recommended to undergo a repeat tomography at the end of therapy. If the lungs are clean and laboratory tests do not reveal active coronavirus, the recovered person is discharged. He can communicate with people around him.
Prevalence and patterns of increased lung tissue density
With the exception of three patients with a normal initial chest CT scan, the remaining 18 of 21 patients (86%) were defined to have changes involving at least one lobe. Of the 21 patients, one patient (5%) had one lobe affected, two patients (10%) had changes in two lobes, three patients (14%) had three lobes affected, four (19%) had four, and in eight patients (38%), pathological changes extended to all five lobes.
The right upper lobe was involved in 14 of 21 patients on initial CT examination (67%), the right middle lobe in 12 (57%), the right lower lobe in 16 (76%), and changes in the left upper lobe were noted in 14 ( 67 %) patients, left lower - in 14 (67 %).
Of the 18 patients with increased lung tissue density, 16 had bilateral changes, and two had unilateral changes (both had the right lung affected). The total “lung severity scale” score ranged from 0 (with three normal CT examinations) to a maximum of 19, with a mean score of 9.9. The patient with the highest severity score was admitted to the intensive care unit (Figure 1). .
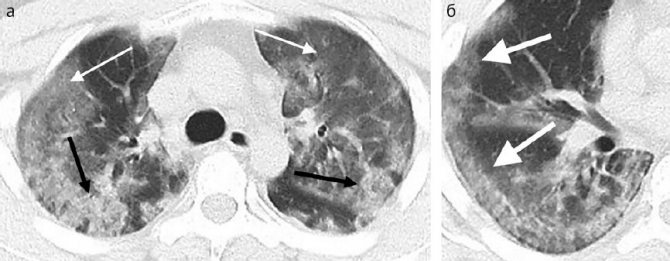
Picture 1
A 29-year-old man with an unknown epidemiological history was admitted with complaints of fever and cough and was immediately referred to the intensive care unit. (a) Axial thin-section CT scan without contrast agent shows diffuse areas of ground-glass consolidation of a confluent nature bilaterally (white arrows) and areas of consolidation (black arrows). (b) Axial CT scan without contrast agent shows that changes in the right middle and lower lobes tend to be peripheral (arrows).
In seven (33%) patients, initial examination revealed ground-glass opacities and/or rounded areas of consolidation (Fig. 2). Three of 21 patients (14%) had indurations with a predominantly linear pattern, and four (19%) had a cobblestone sign (Fig. 3). In seven patients (21%) changes were observed to spread to the peripheral parts of the lung (Fig. 4). No patients had pulmonary cavitations, isolated pulmonary nodules, pleural effusion(s), lymphadenopathy, pulmonary emphysema, or fibrosis. .
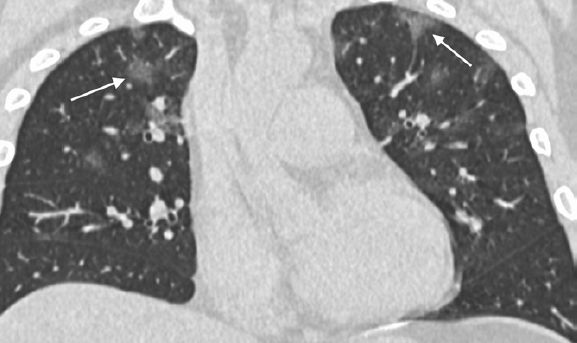
Figure 2
A 36-year-old man with recent travel to Wuhan complained of fever, fatigue, and myalgia. A coronal thin-section CT scan without contrast agent shows rounded areas of ground-glass opacification in both upper lobes (arrows).
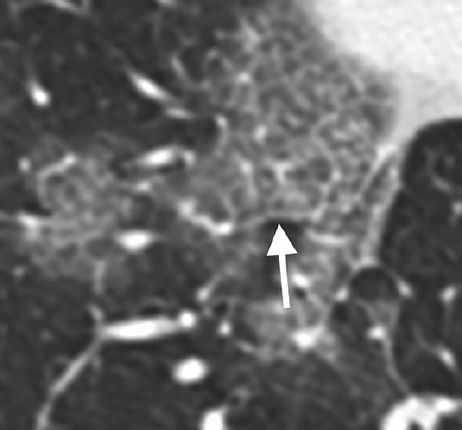
Figure 3
A 66-year-old woman had a fever and productive cough after recent travel to Wuhan. An axial thin-section collimated CT scan without contrast agent shows the cobblestone sign: a reticular pattern of interlobular septal thickening and linear interstitial consolidation associated with a ground-glass lesion in the right lower lobe (arrow).
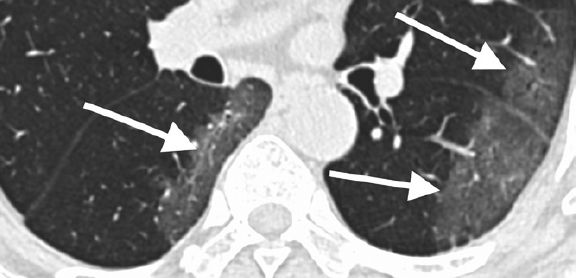
Figure 4
A 69-year-old man who recently visited Wuhan was admitted with fever. An axial thin-section CT scan without contrast agent shows ground-glass opacities in the lower lobes with a strong tendency toward peripheral distribution (arrows).
Who should do it first?
The diagnostic method makes sense to use for the initial assessment of the condition of patients with severe progressive forms of covid , including for separating viral lesions from pneumonia or vascular changes of another origin (community-acquired bacterial pneumonia, pulmonary embolism).
It is necessary to do a CT scan to assess the effectiveness of treatment and the dynamics of lesions, the development of complications, and residual effects.
With a mild or asymptomatic form, it is possible to detect changes in the lungs even before positive test results appear. But in this case, CT data does not influence the choice of treatment and does not become a reason for hospitalization. For these patients, tomography is performed only if:
- clinical indications,
- risk factors,
- organizational capabilities.
Therefore, CT is not practical as a method of mass research for diagnosing coronavirus with a mild or asymptomatic course.
Even with a positive test for coronavirus, a CT scan is not taken:
- In the absence of a respiratory infection clinic
- In the absence of signs of respiratory failure
If Covid is suspected, a computed tomography scan of the lungs should be prescribed by a doctor.
The category of patients for whom a CT scan of the lungs for coronavirus should be performed without fail. Indications:
- moderate course - body t above 38, respiratory rate >22 per minute, shortness of breath during exertion, decreased blood oxygen saturation <95%, which is manifested by paleness, cyanosis of the skin (see shortness of breath with coronavirus),
- severe - t from 39, respiratory rate > 30, blood oxygen saturation 93% or lower, disturbances of consciousness, agitation, blood pressure drop below 90 to 60 mmHg,
- extremely severe course - persistent fever above 38, respiratory rate>35, acute respiratory failure, septic shock, multiple organ failure.
Who should not do it and about contraindications
A mild respiratory infection or suspected coronavirus without symptoms does not require immediate tomography.
When examining pregnant women, newborns and young children, special measures are required to limit radiation doses. Protective collars and aprons are used. The study can begin with an ultrasound of the lungs and only if indicated, a CT scan is prescribed.
Absolute contraindications for tomography:
- without contrast - weight over 130 kg.
- for contrast - pregnancy, allergy to iodine, thyroid pathologies, severe liver or kidney dysfunction.
Relative contraindications:
- fear of confined spaces,
- hyperkinesis (obsessive movements in parkinsonism, cerebral palsy, epilepsy),
- extremely serious condition of the patient.
Indications for CT of the whole body
Whole body scans are not ordered everywhere, but are necessary for the following abnormal conditions:
- osteoporosis, diseases of joints, ligaments, cartilage;
- constant pain of unknown origin;
- metastatic tumors - to control and analyze the spread of the process;
- frequent dizziness and headaches;
- suspicion of a malignant tumor of uncertain location;
- hidden, unclear clinical course of the disease;
- threat of internal hemorrhage.
The proposed diagnostic method allows you to analyze the condition of all organs and systems, timely identify the pathological focus and establish the correct diagnosis. To prevent surprises, a CT scan may be prescribed for preventive purposes.
Scanning has not only examination qualities, but also healing properties. It is advisable to carry out the procedure for the purpose of radiation treatment of certain types of cancer, to drain the internal inflammatory process.
Preliminary preparation for the study
No specific preparation is required for the diagnostic procedure. It is necessary to abstain for some time before it from foods that contribute to gas formation in the intestines (legumes, cabbage, baked goods). 2-3 hours before the procedure, refrain from eating and drinking water.
Immediately before the start of the session, you need to remove all metal objects. Jewelry, precious metals, watches, glasses, and removable dentures are removed. These objects interfere with the operation of the tomograph. A person can remain in clothes, since their fabrics do not interfere with the penetration of the X-ray beam. Some clinics offer special loose shirts.
Before prescribing the technique, it is necessary to notify the doctor about taking medications, the presence of chronic and systemic diseases, and allergic reactions. Separately, it should be said about the need to conduct an allergic and biological test for iodine before performing a contrast scan. The device exposes a person to a certain radiation dose, so it is not recommended to undergo the examination several times within one calendar year.