What is a stroke?
Stroke is a common disease that often leads to disability or death of the patient. It occurs as a result of decreased cerebral blood flow or after hemorrhage in the brain tissue.
Due to a decrease in blood flow or a rupture of a blood vessel, some brain cells die and its function is also lost, in whole or in part.
A person of any age, including childhood, can experience a stroke. In terms of incidence, stroke ranks third after myocardial infarction and oncology, and second among all causes of mortality.
Features of examination after a stroke
After a stroke, MRI is an indispensable method that is superior to CT - changes in soft tissues are visible in the images for a long time:
- swelling - its reduction indicates the effectiveness of treatment;
- cyst - helps to give a prognosis;
- growth of neural networks - if available, the effectiveness of rehabilitation and restoration of lost functions is assessed.
MRI is recommended to be carried out annually; if your health worsens, the doctor will advise you to take pictures more often. Research in the late recovery period is valuable.
MRI is relevant for ischemic stroke; it is difficult to detect hemorrhages in the images. In the future, the tomograph will help determine the effectiveness of treatment and rehabilitation. Studies are carried out annually; on the advice of a doctor, it is sometimes prescribed more often.
Symptoms of a stroke
Symptoms of a stroke are:
- loss of sensation or paralysis on one side of the body,
- loss of visual function (completely/partially),
- speech disorder,
- Strong headache,
- loss of consciousness,
- change in gait.
However, a stroke is not a disease that occurs suddenly. The factors leading to this disease accumulate in the human body for quite a long time (years, tens of years). Poor nutrition, smoking, stress, a sedentary lifestyle - all this leads to rapid wear and tear of the circulatory and nervous systems, and a stroke is the “last straw” when the body can no longer cope with the stress.
Indications for MRI
In case of stroke or suspicion of it, diagnostics such as MRI of the brain
, simply necessary. It is important to correctly and timely assess the degree of damage, the type of stroke and understand the causes of its occurrence.
Brain MRI for stroke is performed when necessary:
- determine the exact size of the lesions;
- identify consequences long after the attack;
- determine the cause of hemorrhage and type of stroke;
- accurately assess the structure of the layers of the brain.
There are also contraindications for MRI. It is claustrophobic because the test involves the patient being in a tight, confined space for 30 minutes or more. Also, MRI is not performed for people weighing more than 120 kg (for technical reasons), if there is a pacemaker, metal implant, or insulin pump in the body.
Procedure
Unlike mid-field MRI, tomographs with a power of at least 1.5 Tesla are used to diagnose cerebrovascular accidents. Preference is given to high-field 3 T devices, which have the following advantages:
- pictures are taken with a large number of sections - this helps to thoroughly examine the lesion;
- the image is clear and informative - thanks to this, an accurate, detailed diagnosis is made;
- the examination time is reduced - this reduces discomfort, the necessary therapy is prescribed, and conclusions are drawn about the prognosis.
Since the study does not require preparation, the doctor makes a decision, and with the patient’s consent, a diagnosis is carried out.
The procedure for performing MRI for stroke includes the following steps:
- removing metal jewelry;
- the doctor makes sure that there are no metal crowns, a pacemaker or an insulin pump;
- the patient lies down on the platform, the head is carefully secured with a belt;
- The patient is placed in the capsule of the device, where images are taken.
The study will take 30-40 minutes. If the patient suddenly becomes ill, he uses the communication button and calls a doctor.
In an emergency situation, when minutes are counting and it is necessary to determine whether there is blood or a blood clot in the head, in this case a CT scan is prescribed (not informative in the first 6 hours).
How to diagnose a stroke on an MRI?
Ischemic stroke
The most common type of stroke. Its occurrence is due to a lack of blood supply to a certain area of the brain. This can happen, for example, due to thrombosis, when an atherosclerotic plaque clogs a vessel supplying the brain.
The first symptoms of an ischemic stroke are quite numerous: frequent headaches, numbness of the limbs, double vision, deterioration of speech. Nausea may also occur, and spots may appear in the eyes.
Bright indicators of ischemic stroke:
- the patient cannot smile or his smile is asymmetrical;
- a person cannot pronounce his name correctly;
- the person feels weakness in the limbs on the affected side.
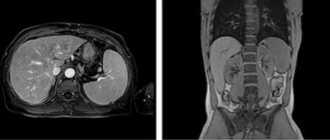
Will an MRI detect the source of a stroke? A diagnostic specialist will be able to see the pathology almost immediately after the hemorrhage has occurred. The affected area is visualized already 3 hours after the attack. The stages of an ischemic stroke are visible on MRI.
Hemorrhagic stroke
Hemorrhagic stroke occurs in approximately 15% of all cases. This is an acute circulatory disorder in the brain, which causes blood to leak from a blood vessel into the brain substance. This condition most often occurs due to a sharp increase in blood pressure. In addition, head injuries can provoke a hemorrhagic stroke.
What does a hemorrhagic stroke look like on MRI? It is necessary to evaluate whether an increase in the T2 signal is visualized and whether the lesion is clearly defined. A qualified diagnostician should pay attention to this and clearly determine the type of stroke.
Subarachnoid hemorrhage
Subarachnoid hemorrhage (CAH) is a severe pathology that is expressed in a sudden (due to trauma or spontaneous) outpouring of blood into the subarachnoid space of the brain.
This type of stroke is uncommon (5-7% of all strokes). At risk are people aged 45-60 years (mostly women).
Ischemic cerebral stroke
Ischemic stroke is the most common form of acute cerebrovascular accident.
Pathology
Cerebral infarction is a zone of necrosis formed as a result of persistent disturbances of cerebral circulation due to stenosis (occlusion), embolism or thrombosis of the main arteries in the neck or brain.
Microscopically
- 12-24 hours: eosinophilic granules in the cytoplasm of neurons, pycnolysis of the nucleus, disappearance of the Nissl substance (body)
- 24-72 hours: neutrophil infiltration
- 3-7 days: infiltration by macrophages and glial cells, beginning of phagocytosis
- 1-2 weeks: reactive gliosis and proliferation of small vessels at the border of the necrosis zone
- more than 2 weeks: formation of a glial scar
Subtypes of ischemic stroke
TOAST and Baltimore-Washington Cooperative Young Stroke Study criteria 1993-1995
- atherothrombotic 14-66%
- cardioembolic 20%
- lacunar (small artery occlusion) 10-29%
- acute stroke with another specific etiology 6-16%
- stroke of unknown etiology 1-8 - 29-40%
Stages by RG Gonzalez
- acute
- up to 6 hours
- interventions are possible
- acute
- 6-24 hours
- stroke may not be visible on CT/MRI
- subacute
- 24 hours - 6 weeks
- contrast accumulation stage
- fogging effect
- chronic
- more than 6 weeks
- resorption and scarring
Diagnostics
CT scan
Early CT signs of ischemic stroke
- Obscuration of lenticular nuclei.
- Pointed increase in MCA density
- Hyperdense middle cerebral artery sign
- Decreased differentiation of the insular cortex
Late CT signs of ischemic stroke:
- zone of hypodense density of brain parenchyma
Magnetic resonance imaging
Diffusion-weighted images
Diffusion-weighted images are most sensitive to stroke. Normally, water protons diffuse extracellularly, so the signal is lost. High signal intensity on DWI indicates a limitation in the ability of water protons to diffuse extracellularly. As a result of cytotoxic edema, an imbalance of extracellular water to Brownian motion occurs, so these changes are clearly detected on DWI. ADC maps may demonstrate a hypointense signal within minutes of stroke onset and are more sensitive than diffusion-weighted images. There are several reports of documented strokes accompanied by the absence of changes on DWI in the first 24 hours, particularly in the vertebrobasilar region. in the trunk and in the case of lacunar infarctions [1].
T2-weighted images
High signal intensity on T2-weighted images does not appear in the first 8 hours after the onset of ischemic stroke. Hyperintensity is characteristic of the chronic phase, reaching a maximum in the subacute period. The haze phenomenon on MRI can be visualized 1–4 weeks after stroke, with a peak occurring at 2–3 weeks, and appears as an isointense area relative to the GM, which is thought to be a consequence of infiltration of the infarct area by inflammatory cells. In large lesions, there may be loss of normal ipsilateral carotid flow on T2-weighted images 2 hours after symptom onset.
FLAIR images
Signal intensity on FLAIR images after stroke varies. Most studies show that signal intensity on FLAIR images changes in the first 6 to 12 hours after symptom onset. The simultaneous presence of changes on DWI and the absence of such changes on FLAIR images indicates a stroke less than 3 (6) hours old with specificity (93%) and positive predictive value (94%) [1].
T1-weighted images
Low signal intensity in the affected area is usually not visible in the first 16 hours after the onset of symptoms, but persists in the chronic phase. The presence of an area of serpinginous cortical hyperintensity may be present in patients with laminar or pseudolaminar necrosis 3 to 5 days after onset, but is most often visualized after 2 weeks.
Signal characteristics depending on the stage [1]:
Early acute stroke (0-6 hours)
- T1 : isointense signal
- T1 with paramagnetic agents : arterial accumulation of contrast agent may occur in the first two hours;
- parenchymal contrast accumulation in an incomplete stroke may occur for 2-4 hours
- isointense signal;
- signal intensity varies;
Late acute period (6-24 hours)
- T1 : usually low signal intensity approximately 16 hours after onset
- T1 with paramagnetic agents : arterial accumulation of contrast material may occur;
- cortical enhancement in incomplete stroke;
- possible meningeal accumulation
Acute and early subacute period (24 hours-1 week)
- T1 : low signal intensity;
- hyperintensity with cortical necrosis (3-5 days)
- arterial and meningeal storage patterns;
Subacute period (1-3 weeks)
- T1 : low signal intensity;
- hyperintensity with cortical necrosis (after 2 weeks)
- high signal intensity on days 10-14;
- low signal intensity on days 7-10;
Chronic period (>3 weeks)
- T1 : low signal intensity;
- may hyperintensity with cortical necrosis (after 2 weeks)
- signal intensity varies;
Differential diagnosis
- CT states simulating cerebral artery hyperdensity high hematocrit
- microcalcifications in the vascular wall
- low density of brain parenchyma (e.g. due to edema), due to which the vessels appear more hyperdense
- infiltrating tumor (eg astrocytoma)
Other diagnostic methods
In addition to MRI, the patient may be prescribed other diagnostics, such as computed tomography (CT) of the brain
. This research method will be the most informative if the patient has a hemorrhagic stroke. CT will detect the disease in the early stages, show even the weakest signs of hemorrhage, and provide complete information about the structure, location, diameter of the lumen of the vessel, as well as the presence of blood clots or atherosclerotic plaques in it. CT is a method used to clarify the location of a vascular rupture.
Which is better for stroke, CT or MRI? Computed tomography is much faster than MRI, but at the same time it has, albeit slightly, a negative radiation effect on the human body.
Angiography with MRI
If it is necessary to assess the degree of cerebral circulatory impairment, angiography is performed with a contrast agent, which is administered a few minutes before the procedure.
The contrast stains the arteries and determines:
- the cause of ischemia (vasospasm, detachment of a blood clot, atherosclerotic plaque);
- level of blockage;
- area of the brain that is left without blood.
Allergy to contrast is rare; a minimal test is done to determine it. If there is no intolerance, a study is carried out.