Breast milk is a unique nutrition that is necessary for the full growth and development of a newborn. Only mother's milk provides the baby with a full range of vitamins and elements. Only such food satisfies the child’s needs 100%. Breast milk contains about 500 nutrients.
To understand how breast milk is produced, let's find out what prolactin is. Prolactin performs reproductive function and regulates the menstrual cycle. This is the hormone where breast milk comes from. During breastfeeding, prolactin levels increase. It begins to act in response to sucking or pumping.
Types of milk
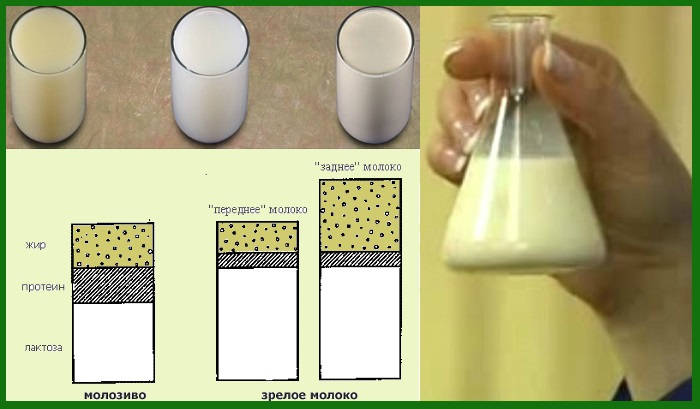
- Colostrum is a sticky, thick, yellow liquid that is produced in the first four days after a baby is born. Colostrum contains more proteins, vitamins and salts and less fat and lactose than other types of milk. This is high-calorie milk with a high content of protective substances, which is very important for a baby in the first days of life;
- Transitional milk appears 4-5 days after birth. The composition of breast milk acquires more fat and approaches the normal mature milk to which we are accustomed;
- Mature milk appears at the end of the second or beginning of the third week. The composition of breast milk continues to change throughout the lactation period, becoming thicker and fattier. In addition, the quality and taste varies depending on the diet of the nursing mother, time of year and day. The composition of breast milk also affects a woman's health and well-being.
Composition of milk
| Component | Functions | Content |
| Water | Provides necessary moisture and quenches thirst. If the baby is fully breastfed, he does not need supplemental feeding | 87-89% |
| Carbohydrates | Accelerate the development of nerve cells and the brain, protect against harmful bacteria and microbes, normalize intestinal function | 7% |
| Fats | A source of strength, vigor and energy, they form and strengthen the immune system, participate in the construction of nerve cells | 4% |
| Squirrels | Provides growth and weight gain for the baby. Low protein content prevents obesity and diabetes | 1% |
| Hormones, vitamins and minerals, antibodies and white blood cells | Provide the necessary dose of substances for full growth and development. And such a small content contributes to quick and easy absorption. | Up to 1% |
Composition of breast milk
percentage of the composition of breast milk
Each woman’s milk is unique, like herself, but the set of components of this product is the same for all nursing mothers. Composition of breast milk:
- Biologically active water (88%) is the main component, perfectly absorbed by infants. If the baby is completely breastfed, then there is no need to give him additional water;
- Carbohydrates (7%) are presented in the form of lactose (milk sugar), which accelerates the development of the brain and nervous system, promotes the full absorption of iron and calcium and the bifidum factor with an antifungal and antibacterial effect that normalizes intestinal function;
- Fats (4%) are a source of strength for the baby: thanks to them, the immune system is strengthened and a full-fledged central nervous system is formed. Fats contain cholesterol (for the production of vitamin D), bile and major hormones. The balance of fats and carbohydrates in breast milk is ideal for a growing baby;
- Proteins (1%) are the basis for the growth of infants who quickly gain weight. They contain whey protein, taurine (for the development of the central nervous system and brain), lactoferrin (a source of iron), nucleotides (building material for DNA), lactase (for the breakdown of lactose), lipase (for complete absorption of fats);
- The remaining components (0.2%) are iron, vitamins, minerals, 20 types of hormones (growth factors), antibodies, leukocytes (protection of the immune system).
The quality of breast milk in a nursing mother is not constant; its composition can change under the influence of many factors:
- The time of day is more dense during the day than at night.
- Weather - in the heat milk is liquid, in the cold it thickens.
- Mom’s health – if you have a weakened immune system or are taking medications, the composition of the product is different.
- The baby's activity - at first the milk is liquid (instead of water), with intense sucking it thickens and becomes fatty.
A mother breastfeeding twins may have a different composition of milk food, because it must be adapted to the needs of each baby. The volume and quality of milk largely depends on the health of the nursing mother, adequate nutrition, sleep and rest patterns, medication intake, and bad habits (nicotine, alcohol).
It is important to know: the more often you put your baby to your breast, the more invaluable product it produces. There will be exactly as much as the baby needs, so you need to feed him on demand! We read about which feeding method to choose - by the hour or on demand.
[sc:rsa]
Types of milk by age
Colostrum, fore and hind milk
- Colostrum is a thick, sticky yellowish liquid produced in small quantities in the first 4 days. Its composition is close to the baby's blood serum - a significant amount of proteins, leukocytes, vitamins, immunoglobulin, and salts. Promotes rapid adaptation of the newborn to a new way of eating. This is why it is so important to put your baby to the breast in the first hours after birth. If the baby was born premature, mother's milk for 2 weeks is close in composition to colostrum, since this is exactly the food the baby needs during this period. On the subject: What is the importance of early attachment of a newborn to the breast;
- Transitional milk is produced in the first 2-3 weeks. In composition, it is more nutritious and less protein, adapted to a growing body and new products;
- Mature milk appears from the third week. It is more oily and watery. Protein is produced less and less with age; mature milk contains mainly fatty acids, which are responsible for normal brain function. Normally, a woman produces up to 1.5 liters of mature breast milk per day. A distinction is made between foremilk and hindmilk: Foremilk - bluish and liquid - is secreted in the first minutes of feeding, it contains carbohydrates, salts and water, and serves to quench thirst.
- The back is yellowish and thick - complete food for the baby.
Benefits of breastfeeding for your baby
- Breast milk reduces the risk of the appearance and development of viral diseases, allergies and dysbacteriosis in infants;
- Breastfeeding provides close emotional contact between mother and baby, which has a positive effect on the psyche and well-being of the newborn;
- Breast milk is always ready for consumption thanks to its sterility and optimal temperature. It does not need to be sterilized or heated or cooled. Artificial mixtures require preparation;
- Breastfeeding prevents the occurrence of vascular and heart diseases, obesity and diabetes;
- Milk contains as many elements as a baby needs for his age. The composition of milk changes with the baby's needs;
- Breast sucking forms the correct bite and prevents caries;
- Mother's milk forms healthy intestinal microflora;
- Breastfeeding promotes the normal formation of hormones and the development of reproductive functions.
NEW LEVEL
An interesting and provocative study recently published in the journal Social Science and Medicine suggests that the benefits of breastfeeding have been exaggerated. Using a clever experimental design, the study authors analyzed information from the U.S. Department of Labor's Bureau of Employment Statistics national database. They questioned the effect of breastfeeding in families with young children (more than one child) on the following parameters from this database: body mass index, obesity, asthma, hyperactivity, attachment to parents, obedience, reading comprehension, hearing comprehension, speech comprehension, mathematical abilities, memory-based intelligence, learning ability. First, the researchers processed data on all families with siblings and noted that breastfed children were better developed than their formula-fed siblings. This applied to all parameters except one: to everyone’s surprise, asthma was more common in infants compared to their artificially-bred siblings. When the researchers scrutinized data from families where one child was breastfed and the other formula-fed (this in-depth study helps control for other modes of feeding besides breastfeeding that may account for the differences), they found no differences between siblings in either one parameter under study. Therefore, the authors concluded that the importance and benefits of breastfeeding are exaggerated.
In the media and blogosphere, this information acquired the status of a sensation, and flashy headlines like: Study claims: “Breast milk is no better than formula.” Are the benefits of breastfeeding overrated, overrated, or the best for your health? Don't rush to blame yourself! A new study has found that the benefits of breastfeeding have been greatly overestimated.
Does this publication really support the view that breastfeeding is not as valuable as is commonly believed? I have several arguments regarding this opinion:
First, the “surprising” results for asthma are not really that surprising. Over the past decades, the belief has emerged that breastfeeding reduces the risk of developing asthma. As asthma increasingly appears as a hereditary disease, it is likely that mothers who have asthma or have a family history of asthma are forced to do everything possible to prevent their children from developing asthma. And it seems likely that the mothers in the study who were asthmatic and/or had a family history of asthma were more motivated to breastfeed in an attempt to prevent their children from developing the disease, precisely because of the widespread belief that Breastfeeding protects against asthma. And because these children are genetically more predisposed to developing asthma, many of them developed asthma despite breastfeeding. In this case, breastfeeding has nothing to do with it, it did not increase the likelihood of developing asthma; on the contrary, the likelihood of a child developing asthma due to genetic predisposition increases the mother’s possible choice in favor of breastfeeding her child. Thus, the analysis established the connection, and the research model only revealed the correlation between these events, but not the cause itself or the direction of the cause-and-effect relationship.
Secondly, the study authors only looked at the effects of breastfeeding on children. But they completely ignored the importance and beneficial effects of breastfeeding on the mother, such as protection against cancer, diabetes, cardiovascular disease and mental illness. Finally, the study factors chosen by the authors seem quite strange to me. The table below shows the benefits of breastfeeding and the risks of using formula, published in many scientific publications:
Table
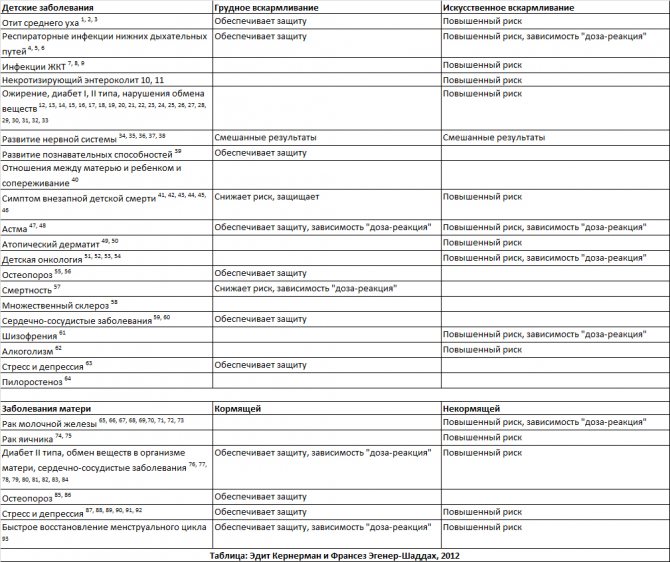
The list of references referred to by the author in the table is presented at the end of this article.
From the list above, I would select asthma, obesity and neurocognitive development as factors that have a weak association between the risk of their development and the protective benefits of breastfeeding. In other words, the study does not conclusively prove that breastfeeding reduces asthma, improves brain development, or protects against obesity. There are many compelling public health reasons for promoting breastfeeding beyond those mentioned in the study. And, as shown in the table, there are many more than these three factors under study. It is also surprising that the authors chose obesity, asthma, and several neurocognitive indicators to study in their study. The effect would have been the same if the authors had initially been biased toward negative study outcome results, choosing to examine factors that were least likely to demonstrate any difference between breastfeeding and formula feeding.
So, does the study clearly demonstrate that formula feeding is as good as breastfeeding? I do not think so. Does this study prove that the benefits of breastfeeding are exaggerated? In relation to obesity, asthma, and cognitive development - perhaps. But for many of the other beneficial effects that breastfeeding has on the baby and mother, it does not.
Links to studies (to the table): 1. Duncan et al. Exclusive Breastfeeding for at least 4 Months Protects Against Otitis Media. Pediatrics, pp 867-872. Vol. 91, No. 5, May 1, 1993. 2. Ip S, Chung M, Raman G, et al. A summary of the Agency for Healthcare Research and Quality's evidence report on breastfeeding in developed countries. Breastfeed Med. 4(suppl):17–30, 2009. 3. Sheryl W. Abrahams and Miriam H. Labbok. Breastfeeding and Otitis Media: A Review of Recent Evidence Current Allergy and Asthma Reports, Volume 11, Number 6, Pages 508-512 4 Bachrach V, Schwarz E, Bachrach L. Breastfeeding and the Risk of Hospitalization for Respiratory Disease in Infancy: A Meta-analysis. Arch Pediatr Adolesc Med. 157(3):237-243. doi:10.1001/archpedi.157.3.237, 2003. 5. W. Oddy et al. Breastfeeding and Respiratory Morbidity in Infancy: A Birth Cohort Study. Arch Dis Child. 88 (3): 224-228, March, 2003. 6. Wilson et al. Relation of Infant Diet to Childhood Health: Seven Year Follow Up of Cohort of Children in Dundee Infant Feeding Study. British Medical Journal. Vol. 316, ISS: 7124. pp. 21-25, 1998. 7. Chien PF, Howie. Breastfeeding and the risk of opportunistic infection in infantry in industrialized and non-industrialized settings. Adv Nutr Res. 10:69-104, 2001. 8. Kramer MS, Chalmers B Hodnett Ed, et al. Promotion of Breastfeeding Intervention Trial (PROBIT): A randomized trial in the Republic of Belarus. JAMA. 285:413-420, 2001. 9. Quigley MA, Cumberland P, et al. How Protective is breast-feeding against diarrheal diseases in infants in 1990s England? A Case-Control Study. Arch dis child. 91(3): 245-50, march, 2006. Epub 2005. 10. Ip S, et al 2009. 11. Holman RC, Stoll BJ, Curns AT et al. Necrotizing enterocolitis hospitalizations among neonates in the United States. Paediatr Perinat Epidemiol. 20:498-506, 2006. 12. Arenz S, Rukerl R, Koletzko B, et al. Breastfeeding and childhood obesity—a systematic review. Int J Obes Relat Metab Disrd. 28:1247–1256, 2004. 13. Harder T, Bergmann R, Kallischnigg et al. Duration of breastfeeding and risk of overweight: a meta-analysis. Am J Epidemiol. 165: 397–403, 2003. 14. Horta BL, Bahl R, Martines JC, et al. Evidence on long-term effect of breastfeeding: systematic review and meta-analyses. Geneva: World Health Organization: 1-57, 2007. 15. Taveras EM, Rifas-Shiman SL, Scanlon KS, Grummer-Strawn LM, Sherry B, Gillman MW. To what extent is the protective effect of breastfeeding on future overweight explained by decreased maternal feeding restriction? Pediatrics. 2006 Dec;118(6):2341-8. 16. Olga Miralles, Juana Sánchez, Andreu Palou, Catalina Picó. A Physiological Role of Breast Milk Leptin in Body Weight Control in Developing Infants *Obesity (2006) 14, 1371–1377; doi: 10.1038/oby.2006.155 17. Owen CG, Whincup PH, Gilg JA et al. Effects of breastfeeding in infancy on blood pressure in later life: a systematic review and meta-analysis. BMJ. 327: 1189–1195, 2003. 18. Martin RM, Gunnell D, Smith GD, et al. Breastfeeding in infancy and blood pressure in later life: systematic review and meta-analysis. Am J Epidemiol. 161:15-26, 2005. 19. Owen CG, Martin RM, Whincup PH, et al. Effect of infant feeding on the risk of obesity across the life course: a quantitative review of published evidence. Pediatrics. 115:1367–1377, 2005. 20. Owen CG, Martin RM, Whincup PH, et al. Does breastfeeding influence risk of type 2 diabetes in later life? A quantitative review of published evidence. Am J Clin Nutr. 84:1043–1054, 2006. 21. Twells L, Newhook LA. Can exclusive breastfeeding reduce the likelihood of childhood obesity in some regions of Canada? Can J Public Health 2010;101(1):36-39 22. Stettler N, Stallings VA, Troxel AB, et al. Weight gain in the first week of life and overweight in adulthood: a cohort study of European American subjects fed infant formula. Circulation 2005;111:1897-1903. 23. Shim JE, Kim J, Mathai RA; STRONG Kids Research Team. Associations of infant feeding practices and picky eating behaviors of preschool children. J Am Diet Assoc. 2011 Sep;111(9):1363-8. 24. Shields L, Mamun AA, O'Callaghan M, Williams GM, Najman JM. Breastfeeding and obesity at 21 years: a cohort study. J Clin Nurs. 2010 Jun;19(11-12):1612-7. 25. Seach KA, Dharmage SC, Lowe AJ, Dixon JB. Delayed introduction of solid feeding reduces child overweight and obesity at 10 years. International Journal of Obesity 2010 Oct;34(10):1475-9 26. Musso G, Gambino R, Cassader M. Obesity, diabetes, and gut microbiota: the hygiene hypothesis expanded? Diabetes Care. 2010 Oct;33(10):2277-84. 27. Metzger MW, McDade TW. Breastfeeding as obesity prevention in the United States: A sibling difference model. Am J Human Biology 2010;22:291-296. 28. Martens PJ. What do Kramer's Baby Friendly Hospital Initiative PROBIT studies tell us? A review of a decade of research. Journal of Human Lactation 2012 Aug;28(3):335-42. 29. Mangrio E, Lindström M, Rosvall M. Early life factors and being overweight at 4 years of age among children in Malmö, Sweden. BMC Public Health. 2010 Dec 15;10:764. 30. L i R, Magadia J, Fein SB, Grummer-Strawn LM. Risk of Bottle-feeding for Rapid Weight Gain During the First Year of Life. Arch Pediatr Adolesc Med. 2012 May;166(5):431-6. 31. Karanja N, Lutz T, Ritenbaugh C, Maupome G, Jones J, Becker T, Aickin M. The TOTS community intervention to prevent overweight in American Indian toddlers beginning at birth: A feasibility and efficacy study. J Community Health. 2010 Dec;35(6):667-75. 32. Shim JE, et al 2011 33. Scott JA, Ng SY, Cobiac L. The relationship between breastfeeding and weight status in a national sample of Australian children and adolescents. BMC Public Health. 2012 Feb 7;12:107. 34. Anderson JW, Johnstone BM, Remley DT. Breastfeeding and cognitive development: a meta-analysis. Am J Clin Nutr. 70: 525-535, 1999. 35. Stuebe, Alison. The Risks of Not Breastfeeding for Mothers and Infants. Reviews in Obstetrics and Gynecology. Vol.2 No. 4, 2009. 36. Jain A, Concato J, Leventhal JM. How good is the evidence linking breastfeeding and intelligence? Pediatrics. 109:1044–1053, 2002. 37. Drane DL, Logemann JA. A critical evaluation of the evidence on the association between type of infant feeding and cognitive development. Paediatr Perinat Epidemiol. 14:349-356, 2000. 38. Dewey KG, Cohen RJ, Brown KH, et al. Effects of exclusive breastfeeding for four versus six months on maternal nutritional status and infant motor development: results of two randomized trials in Honduras. J Nutr. 131: 262-267, 2001. 39. Kramer MS, et al 2001. 40. Kim P et al. J Child Psych Psychiatry 2011 41. M, Raman G, et al. A summary of the Agency for Healthcare Research and Quality's evidence report on breastfeeding in developed countries. Breastfeed Med. 4(suppl):17–30, 2009. Breastfeeding and the Risk of Postneonatal Death in the United States 42. Aimin Chen and Walter J. Rogan Pediatrics 2004;113;e435. 43. McVea KL, Turner PD, Peppler DK. The role of breastfeeding in sudden infant death syndrome. J Hum Lact. 16:13-20, 2000 44. American Academy of Pediatrics Task Force on Sudden Infant Death Syndrome. The changing concept of sudden infant death syndrome: diagnostic coding shifts, controversies regarding the sleeping environment, and new variables to consider in reducing risk. Pediatrics. 116: 1245-1255, 2005 45. McKenna, JJ, Ball, HL and Gettler, LT (2007), Mother–infant cosleeping, breastfeeding and sudden infant death syndrome: What biological anthropology has discovered about normal infant sleep and pediatric sleep medicine. Am. J. Phys. Anthropol., 134: 133–161. doi: 10.1002/ajpa.20736 46. Vennemann MM, Bajanowski T, Jorch G, Mitchell EA. Does Breastfeeding reduce the Risk of Sudden Infant Death Syndrome?” Pediatrics Vol.123, March 2009, pp e406-410 47. Ip S, et al, 2009. 48. Ip S et al. Breastfeeding and Maternal and Infant Health Outcomes in Developed Countries. US AHRQ. 2007 49. Gdalevich M, Mimouni D, David M, et al. Breast-feeding and the onset of atopic dermatitis in childhood: a systematic review and meta-analysis of prospective studies. J Am Acad Dermatol. 45: 520-527, 2001. 50. Kramer MS, et al, 2001. 51. C Svanborg, A Aits, P Brest et al. HAMLET, a tumoricidal molecular complex form human milk. BioMed Central. 3 (suppl 5): S11, 2009. 52. Greaves MF. Speculation on the cause of childhood lymphoblastic leukemia: a meta-analysis. Leukemia 2: 120-125, 1988. 53. Ip S, Chung M, Raman G, et al. A summary of the Agency for Healthcare Research and Quality's evidence report on 54. Schraw J, et al “Longer formula feeding and later age at introduction of solids increase the odds ratio of pediatric acute lymphoblastic leukemia” AACR-FCPR 2012; Abstract A102. 55. Bishop NJ, Dahlenburg SL, Fewtrell MS, et al. Early diet of preterm infants and bone mineralization at age five years. Acta Pædiatr 1996;85:230-6 56. Ryan S. Bone mineralization in Preterm Infants. Nutrition. 1998;14:745-747 57. Aimin Chen, MD, PhD, Walter J. Rogan, MD Breastfeeding and the Risk of Postneonatal Death in the United States PEDIATRICS Vol. 113 No. 5 May 1, 2004 pp. E435 -e439 58. Conradi S, Malzahn U, Paul F, Quill S, Harms L, Then Bergh F, Ditzenbach A, Georgi T, Heuschmann P, Rosche B. Breastfeeding is associated with a lower risk for multiple sclerosis. Mult Scler. 2012 Sep 4 59. Williams, M. J. A., Williams, S. M., & Poulton, R. (2006). Breast feeding is related to C-reactive protein concentration in adult women. Journal of Epidemiology and Community Health, 60, 146-148 60. Brion MJ, Lawlor DA, Matijasevich A, Horta B, Anselmi L, Araújo CL, Menezes AM, Victora CG, Davey Smith G What are the causal effects of breastfeeding on IQ , obesity and blood pressure? Evidence from comparing high-income with middle-income cohorts. Int J Epidemiol. 2011 Feb 24. 61. HJ Sørensen, EL Mortensen, JM Reinisch, SA Mednick. Breastfeeding and risk of schizophrenia in the Copenhagen Perinatal Cohort. 62. Acta Psychiatr Scand. July 2005; 112(1): 26–29. doi: 10.1111/j.1600-0447.2005.00548.x 63. Sørensen HJ, Mortensen EL, Reinisch JM, Mednick SA. Early weaning and hospitalization with alcohol-related diagnoses in adult life. Am J Psychiatry. 2006 Apr;163(4):704-9. 64. Montgomery, S. M., Ehlin, A., & Sacker, A. (2006). Breast feeding and resilience against psychosocial stress. Archives of Diseases of Childhood, 91, 990-994 65. Krogh, C et al. Bottle-feeding and the Risk of Pyloric Stenosis. Pediatrics, Sept 2012 online 66. Stuebe AM, Willet WC, Xue F, et al. Lactation and incidence of premenopausal breast cancer: a longitudinal study. Arch Intern Med. 169:1364–1371, 2009. 67. Tryggvadóttir L, Tulinius H, Eyfjord JE, et al. Breastfeeding and reduced risk of breast cancer in an Icelandic cohort study. Am J Epidemiol.154:37-42, 2001 68. Michels KB, Willet WC, Rosner BA, et al. Prospective assessment of breastfeeding and breast cancer incidence among 89,887 women. Lancet. 347:431-436, 1996. London SJ, Colditz GA, Stampfer MJ, et al. Lactation and risk of breast cancer in a cohort of US women. Am J Epidemiol.132:17-26.1990. 69. Stuebe, Alison et al Arch Intern Med 2009; 70. Lee SY, Kim MT, Kim SW, et al. Effect of lifetime lactation on breast cancer risk: a Korean women's cohort study. Int J Cancer. 105: 390-393, 2003. 71. Kvale G, Heuch I. Lactation and cancer risk: is there a relation specific to breast cancer? J Epidemiol Community Health. 42:30-37, 1988. 72. Collaborative Group on Hormonal Factors in Breast Cancer. Breast cancer and breastfeeding: collaborative reanalysis of individual data from 47 epidemiological studies in 30 countries, including 50,302 women with breast cancer and women without the disease. Lancet. 360:187–195, 2002. 73. Bernier MO, Plu-Bureau G, Bossard N, et al. Breastfeeding and risk of breast cancer: a meta-analysis of published studies. Hum Reprod Up-date. 6:374–386, 2000. 74. Cramer DW, Titus-Ernstoff L, McKolanis JR, et al. Conditions associated with antibodies against the tumor-associated antigen MUC1 and their relationship to risk for ovarian cancer. Cancer Epidemiol Biomarkers Prev.14: 1125-1131,2005 75. Danforth KN, Tworoger SS, Hecht JL, et al. Breastfeeding and risk of ovarian cancer in two prospective cohorts. Cancer Causes Control.18:517-523, 2007 76. Kac G, Benício MHDA, Velásquez-Meléndez G, Joaquim et al. Breastfeeding and postpartum weight retention in a cohort of Brazilian women. Am J Clin Nutr 2004; 79: 487 – 493 Olga Miralles, et al. 2006 77. Stuebe AM, Michels KB, Willett WC, et al. Duration of lactation and incidence of myocardial infarction in middle to late adulthood. Am J Obstet Gynecol. 200:138.e1-e8. 2009. 78. Stuebe AM, Rich-Edwards JW, Willett WC, et al. Duration of lactation and incidence of type 2 diabetes. JAMA. 294:2601–2610, 2005. 79. Dewey KG, Heinig MJ, Nommsen LA. Maternal weight-loss patterns during prolonged lactation. Am J Clin Nutr. 58:162–166, 1993. 80. Schwarz EB, Ray RM, Stuebe AM, et al. Duration of lactation and risk factors for maternal cardiovascular disease. Obstet Gynecol. 113:974-982, 2009. 81. Stuebe AM, Rich-Edwards JW. The reset hypothesis: lactation and maternal metabolism. Am J Perinatol. 26:81-88, 2009. 82. Eleanor Bimla Schwarz, MD, MS, Roberta M. Ray, MS, Alison M. Stuebe, MD, MSc, 83. Matthew A. Allison, MD, MPH, Roberta B. Ness, MD, MPH, Matthew S. Freiberg, MD, MSc, and Jane A. Cauley, DrPH Duration of Lactation and Risk Factors for Maternal Cardiovascular Disease 84. Ram KT, Bobby P, Hailpern SM, et al. Duration of lactation is associated with lower prevalence of the metabolic syndrome in midlife-SWAN, the study of women's health across the nation. Am J Obstet Gynecol. 198:268.e1-e6, 2008. 85. Chantry CJ, Auinger P, Byrd RS. Lactation among adolescent mothers and subsequent bone mineral density. Arch Pediatr Adolesc Med 2004;158:650-6 86. Ward et al. Curr Opin Obstet Gynecol. 2005 87. Groer, M. W. (2005). Differences between exclusive breastfeeders, formula-feeders, and controls: A study of stress, mood, and endocrine variables. Biological Nursing Research, 7(2), 106-117 88. Groër, M. W., Davis, M. W., Smith, K., Casey, K., Kramer, V., & Bukovsky, E. (2005). Immunity, inflammation and infection in post-partum breast and formula feeders. American Journal of Reproductive Immunology, 54, 222-231 89. Groer, M. W., & Davis, M. W. (2006). Cytokines, infections, stress, and dysphoric moods in breastfeeders and formula feeders. Journal of Obstetric, Gynecologic and Neonatal Nursing, 35, 599-607 90. Heinrichs, M., Meinlschmidt, G., Neumann, I., Wagner, S., Kirschbaum, C., Ehlert, U., et al. (2001). Effects of suckling on hypothalamic-pituitary-adrenal axis responses to psychosocial stress in postpartum lactating women. Journal of Clinical Endocrinology & Metabolism, 86, 4798-4804 91. Kendall-Tackett, K. A new paradigm for depression in new mothers: The central role of inflammation and how breastfeeding and anti-inflammatory treatments protect maternal mental health. International Breastfeeding Journal, 2:6(https://www.internationalbreastfeedingjournal.com/content/2/1/6).2007 92. Peus V, Redelin E, Scharnholz B, Paul T, Gass P, Deuschle P, Lederbogen F , Deuschle M: Breast-Feeding in Infancy and Major Depression in Adulthood: A Retrospective Analysis. Psychother Psychosom 2012;81:189-190 93. McNeilly A. Endocrinol Metab Clin North Am. 1993 Mar;22(1):59-73
Benefits of breastfeeding for mom
- Pre-pregnancy forms and the body of a woman who is breastfeeding are restored faster. This occurs due to the hormone oxycidine, which is produced during sucking. Oxtiocide contracts the uterus, which promotes recovery;
- Lactational amenoria is a natural method of contraception that gives rest to a woman’s reproductive system and protects against a new pregnancy. The effectiveness of this method is 98-99%. However, the method only works with complete and properly organized breastfeeding! Be careful: a new pregnancy during lactation is possible even in the absence of menstruation!;
- Breastfeeding reduces a woman's risk of cancer;
- Neropeptides or “happiness hormones”, which are produced during breastfeeding, give strength and energy, elevate mood and increase resistance to stress. This is very important for a woman, because caring for a newborn requires a lot of emotional and physical strength;
- Breastfeeding promotes rapid bone tissue renewal and the removal of toxins from the body. This strengthens the mother’s immunity and improves her well-being.
A secret behind seven seals: breastfeeding is good for mothers
Alicia Dermer - family physician, professional consultant IBCLC Old Bridge, New Jersey, USA From NEW BEGINNINGS magazine, issue 18 No. 4 July-August 2001, pp. 124-127
Translation by Victoria Khudyakova and Maria Sorokina Edited by Natalia Gerbeda-Wilson
Thanks for providing the photo to Alisa and her daughter Sonya
The article has been updated to correct outdated information, add the latest scientific data, and remove information that relates to the United States and is not at all consistent with Russian cultural or historical realities.

Everyone knows that breastfeeding is good for babies. Did you know that breastfeeding is good for mothers too? Every now and then you hear around that feeding takes away strength and ruins a woman’s health. But is it? Few people know that breastfeeding is as beneficial for the health of mothers as it is for children. Breastfeeding is not only a continuation of the natural physiological process that began with conception and pregnancy. Breastfeeding is beneficial not only because it prevents postpartum bleeding immediately after childbirth, or simply feels good while the woman is breastfeeding. The positive and protective effects of breastfeeding are noticeable throughout a woman's life. Today we have ample scientific evidence that not only is breastfeeding beneficial, but that if a woman does not breastfeed, she is more likely to develop certain types of cancer or osteoporosis.
Unfortunately, even those health workers who know about the benefits of feeding for mothers rarely pay attention to this topic when counseling expectant parents, and it is often not mentioned at all in books and magazines. Why is breastfeeding good for women? Why do so few mothers know about this? Let's figure it out together and find answers to these questions.
The influence of breastfeeding on the physiology of the female body
Immediately after birth, when the baby is frequently latched to the breast, the mother's pituitary gland releases the hormone oxytocin. Oxytocin not only stimulates the release of milk from the mammary glands (milk ejection reflex or “hot flashes”), but also contracts the muscles of the uterus. This prevents postpartum bleeding and promotes uterine involution (the return of the uterus to its pre-pregnancy state). Women who are breastfed with artificial breast milk substitutes are often given synthetic oxotocin drips immediately after birth, but bleeding persists for the next few days, when the risk of bleeding is highest without the protective effect of oxytocin.
Typically, a woman will not have her period as long as she is breastfeeding her baby exclusively, not supplementing with formula or adult foods, and when she is not giving her baby a pacifier (Lawrence and Lawrence 1999). Lactational amenorrhea (absence of menstruation during breastfeeding) in breastfeeding women lasts from several months to several years, in contrast to women who feed their children artificial formula. What is the benefit of not having periods? Amenorrhea often helps naturally delay the next pregnancy and also preserves iron in the mother's body.
The amount of iron that is consumed during lactation is much less than during blood loss during menstruation, therefore, compared to non-breastfeeding mothers, nursing mothers are less likely to have iron deficiency anemia. The longer a mother breastfeeds and the longer her period goes without returning, the lower the risk of anemia (Institute of Medicine 1991). (editor's note. Blood loss during normal periods is insignificant and does not lead to anemia. The risk of anemia is only in women with excessively heavy or prolonged periods. I could not find the study that the author refers to. The full text of the document is here. The difference is The incidence of anemia between breastfeeding and non-breastfeeding may be explained by more frequent pregnancies in non-breastfeeding.)
As already mentioned, lactational amenorrhea is an effective way to prevent pregnancy. Scientific studies show that the lactational amenorrhea method (LAM) is a reliable method of contraception with an effectiveness of 98-99% in the first 6 months after childbirth. The LAM method helps naturally space births, which prevents infant mortality, and gives the mother the opportunity to recover between pregnancies. Women who formula feed should start using contraception 6 weeks after birth (Kennedy 1989).
Long-term benefits of breastfeeding
Today we have more and more evidence that breastfeeding is beneficial not only immediately after childbirth. Scientific research shows that breastfeeding is very important for a mother's health. If a woman does not breastfeed, it negatively affects the metabolism, increases the risk of various types of cancer, and can also have a negative impact on the psychological health of the mother.
Milk production is an active metabolic process that consumes approximately 200-500 calories per day. A non-breastfeeding mother would need to swim at least 30 pools or bike uphill for an hour every day to burn the same amount of calories. It is clear that breastfeeding mothers are more likely to lose weight gained during pregnancy more quickly. Research confirms that non-breastfeeding mothers have a harder time losing weight and have a harder time maintaining their normal weight than breastfeeding mothers (Brewer 1989).
Maintaining a stable, healthy weight is especially important for women who develop diabetes during pregnancy (gestational diabetes). After birth, breastfeeding women with gestational diabetes have lower blood sugar levels than non-breastfeeding mothers with the same diagnosis (Kjos 1993). It is especially important for these women to lose excess weight because they are already at increased risk of developing diabetes in the future, and excess weight further increases the risk of diabetes. Breastfeeding helps you maintain a healthy weight and therefore reduces your risk of diabetes in the future. Women with juvenile-onset diabetes need less insulin during breastfeeding because breastfeeding lowers blood sugar levels.
Breastfeeding mothers tend to have high levels of "good cholesterol" (high-density lipoprotein cholesterol, HDL - translator's note) (Oyer 1989). A healthy weight, normal blood sugar levels, and high levels of “good cholesterol” can all reduce your risk of heart disease in the future. This is especially important for women, since heart attacks are the leading cause of death among women (Editor's note: According to the World Health Organization, cardiovascular disease is the leading cause of death in women worldwide. Indeed, the most recent research shows that in breastfeeding women who for a total of two years or longer during their life, the risk of coronary heart disease was lower than for non-breastfeeders.)
Let's talk about calcium now. You've probably heard that when a woman breastfeeds, calcium is washed out of her bones. Because women lose calcium during lactation, some health care providers mistakenly believe that breastfeeding women have a higher risk of osteoporosis. (Editor's note. The content of calcium and phosphorus in the blood of lactating women is higher than that of non-lactating women. Lactation stimulates the absorption of calcium and the active form of vitamin D, which helps absorb calcium. This is especially noticeable after stopping breastfeeding. Such changes in the mechanism of absorption, assimilation and excretion calcium may help conserve calcium during lactation. Even if a woman has a low calcium intake, there is no benefit from dietary calcium supplementation. Studies show that in the group supplemented with supplemental calcium, excess calcium was excreted in the urine. (Lawrence & Lawrence 2005)) However, modern Research shows that once breastfeeding women stop breastfeeding, their bone density returns to pre-pregnancy levels or even higher (Sowers 1995). As you can see, lactation strengthens bones and reduces the risk of osteoporosis. Moreover, women who have not breastfed are at greater risk of hip fractures after menopause (Cummings 1993).
Numerous studies have found that women who have not breastfed are more susceptible to cancer of the reproductive system. Ovarian and uterine cancer most often affects women who did not breastfeed. This may be due to repeated ovulation cycles and the influence of estrogen, which is higher in women who are not breastfeeding. An analysis of data from 47 epidemiological studies from 30 countries, which compared 50 thousand women with breast cancer and about 100 thousand women without breast cancer, showed that, compared with healthy women, among women who developed breast cancer, more were those who did not breastfeed at all. chest. It was also found that the average total duration of breastfeeding among patients with the disease was more than half as long (Collaborative Group on Hormonal Factors in Breast Cancer). The cause of this phenomenon may be suppression of ovulation and decreased estrogen levels; but it is also important that breastfeeding is a normal physiological function of the mammary glands. This assumption emerged from a study in which women who fed only one breast were significantly more likely to suffer from cancer of the breast that did not lactate. (Ing, Ho, and Petrakis 1977).
Two studies have documented an increase in rheumatoid arthritis among breastfeeding mothers (Jorgensen 1996; Brenna 1994). However, another study found that the severity and mortality rate of rheumatoid arthritis were higher among women who had never breastfed. (Brun, Nilson, and Kvale 1995). (Editor's note: A 2004 study found that breastfeeding mothers have a lower risk of developing rheumatoid arthritis, and the longer they breastfeed, the lower the risk.)
For other studies on how bottle-feeding harms women's health, read the Difference between breastfeeding and bottle-feeding section.
In summary, breastfeeding reduces the risk factors for three of the most serious diseases among women: gynecological cancer, heart disease and osteoporosis, without having a noticeable negative impact on a woman's health, contrary to popular misconceptions.
Breastfeeding and psychology
If the incidence of various diseases can be measured in numbers, then how can we measure the peace of mind of the mother of a healthy baby? How to calculate stress in a family where a lot of money is spent on buying formula and increased medical expenses?
Health organizations recommend breastfeeding because of its proven health benefits, but they fail to communicate to every mother and family how breastfeeding can impact the emotional relationship between mother and child. In Western society, the choice between breastfeeding and bottle feeding is still seen largely as a personal decision for the mother, based primarily on the mother's convenience (Editor's note: In Russia, most women still do not choose to breastfeed or formula feed, but turn to artificial substitutes are forced. The idea that one can choose not to breastfeed often arises among women who find themselves in an environment where the ideology of such a choice is a cultural norm. The idea that breastfeeding and formula feeding is just a choice between two products, rather than a choice between two very different processes, launched by manufacturers of artificial breast milk substitutes.) When a mother decides not to breastfeed, she does not take into account that family life can turn into a complete stress if the child is often sick, or that she and the child will not have those special relationships that only develop during breastfeeding.
Breastfeeding sets the tone for a certain relationship between mom and baby that is difficult to replicate for women who bottle feed. (Editor's note: Is it possible to imitate behavior similar to breastfeeding while bottle feeding? Without a doubt! To do this, you first need to know how exactly breastfeeding differs from bottle feeding, and then work, work and work again to artificially bring to life what happens on its own during breastfeeding without additional thought and effort.) Sucking at the breast creates a certain hormonal background in the mother. (Editor's note: Oxytocin, the hormone that is responsible for milk letdown, acts as a sedative for moms.) One study shows that breastfeeding mothers have a weaker response to adrenaline, a hormone that is released during stressful, dangerous and anxious situations. (Altemus 1995). (Editor's note: Maybe because of this, breastfeeding women are more patient with their babies, they have less depression, and they believe that they have less stressful situations, compared to those who feed formula? The difference between breastfeeding and artificial feeding. )
Measuring the impact of breastfeeding on peace in a society is especially difficult if in this society few people are able to breastfeed for any long period of time, and feeding is supported only in words and not in deeds. When a woman tries to breastfeed in such an environment, she inevitably faces practical and emotional difficulties, such as establishing breastfeeding or how to fend off advice-givers. (How to Avoid Controversy and Respond to Criticism About Breastfeeding) The reason for these problems lies in the fact that there are few or no examples of successful breastfeeding around. The problems are aggravated by the fact that the formula is very easy to buy, and, at the same time, it is difficult to find a health worker who will not prescribe the formula at the first opportunity, but will help establish breastfeeding.
Even if the mother managed to establish feeding, she no, no, and will hear judgmental remarks like “Are you still feeding?” or “Your milk is low-fat, there is nothing useful in it anymore, stop starving the child - give him formula!” Or a woman goes to work, and there are absolutely no suitable conditions there to feed the baby or express milk. And how many women are reproached and shamed for going to a cafe or museum and being fed there! It is not surprising that not every mother will remember feeding as a pleasant and peaceful time in her life...
| Why do so few people know about the benefits of breastfeeding for women? The evidence clearly indicates that breastfeeding is a normal and healthy condition that is beneficial to both the body and soul of a woman. And in life, most mothers feed solely because it is good for children, while society views breastfeeding as torture for the sake of the child’s health. Faced with some easily solvable problem, a woman stops feeding early, but then blames herself for depriving the child of something healthy. There are always “well-wishers” nearby who will reassure and assure: “How many healthy children grew up on formula!” Do you think that if women knew that breastfeeding was good for themselves, maybe they would figure out how to solve the problem that made them stop breastfeeding? If society knew that formula feeding poses significant risks to women's health, might it not be so easy to encourage women to stop breastfeeding? Why don’t mothers know that feeding is not torture, but salvation? Many mothers are simply not told how healthy and normal breastfeeding is. Lack of common sense, ignorance, low level of education, the influence of historical, cultural and personal prejudices, advertising of manufacturers of artificial breast milk substitutes lead to the fact that health workers who are today responsible for disseminating knowledge about breastfeeding either themselves do not know, or know but are silent, and sometimes even embarrassed to say what has long been known to science. It's time to reveal this secret! When this information becomes common knowledge, perhaps there will be an atmosphere in society in which breastfeeding is easy and enjoyable for most women, and if any woman does encounter problems, there will be plenty of accessible ways to solve them. Women will stop tormenting, suffering and being victims of feeding, and instead will fully enjoy the joy and health that seem to be intended by nature itself as a reward for maternal work. |
Alicia Dermer, a family physician, professional lactation and breastfeeding consultant IBCLC, is a clinical associate professor in the Department of Family Medicine at the University of Medicine and Dentistry of the Medical Institute of New Jersey-Robert Wood Johnson in New Brunswick, NJ.
Bibliography
Altemus, M. et al. Suppresion of hypothalmic-pituitary-adrenal axis responses to stress in lactating women. J Clin Endocrinal Metab 1995;80:2954.
Brenna, P. Breast-feeding and the onset of rheumatoid arthritis. Arthritis Rheum 1994; 6:808.
Brun, J., Nilssen, S., Kvale, G. Breast feeding, other reproductive factors and rheumatoid arthritis: A prospective study. Br J Rhemmatol 1995;34:542.
Brewer, MM, Bates, MR, Vannoy, LP Postpartum changes in maternal weight and body fat deposits in lactating vs. nonlactating women. Am J Clin Nurs 1989; 49:259.
Dewey, K. Heinig, M., Nommsen, L. Maternal weight-loss patterns during prolonged lactation. Am J Clin Nurs 1993; 58:162.
Hale, Thomas. Medicines and Mothers' Milk Amarillo, TX: Pharmasoft Medical Publishing, 2000.
Ing, K, Ho, J., Petrakis, N. Unilateral breastfeeding and breast cancer. Lancet 1977; 2:124.
Jorgensen, C. et al. Oral contraception, parity, breast feeding, and severity of rheumatoid arthritis. Ann Rheumatic Dis 1996; 55:94.
Kennedy, KL et al. Consensus statement on the use of breastfeeding as a family planning method. Contraception. 1989 May;39(5):477-96.
Kramer, F., Stunkard, A., Marshall, K, et al. Breastfeeding reduces maternal lower-body fat. J Am Diet Assoc 1993; 93:429.
Kjos, S. Henry O. Lee, R., eta al. Effect of lactation on glucose and lipid metabolism in women with recent gestational diabetes. Obstet Gynecol 1993; 82:451.
Lawrence, R., Lawrence, R. Breastfeeding: A Guide for the Medical Profession. St. Louis: Mosby, 1999.
Layde, P., et al. The independent associations of parity, age at first full term pregnancy, and duration of breastfeeding with the risk of breast cancer J Clin Epidemiol 1989; 42:963.
Newcomb, P. et al. Lactation and a reduced risk of postmenopausal breast cancer. N Engl J Med 1994; 330:81.
Oyer, D., Stone, N. Cholesterol levels and the breastfeeding mom. JAMA 1989, 262:2092.
Sowers, M., Randolph, J., Shapiro, S. Jannausch, M. A prospective study of bone density and pregnancy after an extended period of lactation with bone loss. Ostet Gynecol 1995; 85:285.
Specker, B. Tsang, R., Ho, M. Changes in calciurn homeostasis over the first year postparturn: Effect of lactation and weaning. Obstet Gynecol 1991; 78.56.
Sinigaglia, L., Varenna, M., Binelli, L., Gallazzi, M., Calori, G., Ranza, R. Effect of lactation on postmenopausal bone mineral density of the lumbar spine. J Reprod Med 1996;41:439.
Breastfeeding rules
- Correct infant attachment and feeding position. Make sure your baby latch onto both the nipple and areola. Read more about how to properly organize feeding here;
- Feed your baby on demand, not according to a schedule. During the day, a newborn should be fed every two hours, at night - at least four times. However, if your baby requires more, feed more often;
- The nutrition of a nursing mother affects the well-being of the baby. After all, food components pass into breast milk, and then to the baby. They can cause both positive and negative reactions. This could be allergies, stomach upsets, or even poisoning. The breastfeeding diet will tell you how to eat properly;
- Choose comfortable underwear for feeding, take care of hygiene and nipples. It is enough to wash your breasts twice a day with warm water using liquid neutral soap. It is better to wipe with napkins. Regular soap and towels rub and irritate the breasts;
- Regularly check your breasts for lumps and lumps to avoid future problems such as lactostasis or mastitis;
- Prevent cracked nipples. Infection can get into breast milk through cracks and wounds! In addition, painful nipples lead to lactostasis and mastitis. For prevention, use cabbage leaf compresses, special ointments and creams for nursing mothers containing retinol. Which remedy is better to choose, read the article “Cracks and abrasions on the nipples during feeding”;
- If there is a need to express, then it is better to do the procedure by hand;
- Do not take medications without consulting your doctor! Many medications are dangerous for babies and cause intoxication, delays in growth and development;
- To maintain lactation longer, drink more fluids. The required volume is 2-3 liters, with half the volume being plain drinking water. In addition, foods and drinks to improve lactation will help increase milk production;
- Complementary feeding begins at 4-5 months. But you can continue breastfeeding as long as lactation continues. Doctors recommend stopping breastfeeding when the baby is 1.5-2 years old. However, this is an individual decision that depends only on the child and mother.
Plenty of warm drinks, proper nutrition and well-established breastfeeding are the key to successful lactation, high-quality and healthy breast milk! Don't stop breastfeeding unless absolutely necessary. No amount of formula can replace the benefits of breast milk.
Subscribe to our VKontakte group
Breastfeeding: benefits not only for the child, but also for the mother
Pregnancy, childbirth and lactation are three acts of the play that the female body “acts out” after conception. All organs and systems are set up for a long story in three acts, where everything that happens is interconnected. Some metamorphoses prepare others, smoothly moving from the beginning to the climax and denouement - the moment when the system, having completed the task, switches to another mode of life. Now imagine, after the second act of the play, the audience is told that the theater is closing and they will not see the continuation of the performance. People will experience disappointment, resentment, in other words, stress. And the same condition occurs in an organism that is deprived of the opportunity to accomplish what it carefully and systematically prepared for.
Breastfeeding has different stages, and each has its own duration. Immediately after birth, the colostrum period begins, after 3 days milk comes, and during the first 1.5 months the feeding process is established, then the stage of mature lactation follows. With the introduction of complementary foods, new metamorphoses occur: the feeding regime changes, milk production slows down and gradually disappears. If a mother tries to “jump” over a step, in a hurry to wean the baby from the breast, then the natural course of events is interrupted. The normal duration of breastfeeding is at least 10 months, and it is best to wean your baby from the breastfeeding breast when he is between 1 year 3 months and 1 year 7 months. If a woman says that she fed her baby for up to 4 months, this means that she has just begun to master breastfeeding.
Due to the unexpected interruption of breastfeeding at the very beginning, a woman’s body experiences trauma at the hormonal level, tantamount to the loss of a child. In an effort to compensate for the loss, systems and organs begin to urgently, under stress and overexpenditure of vital resources, prepare for a new pregnancy. And this condition will complicate and delay recovery after childbirth.
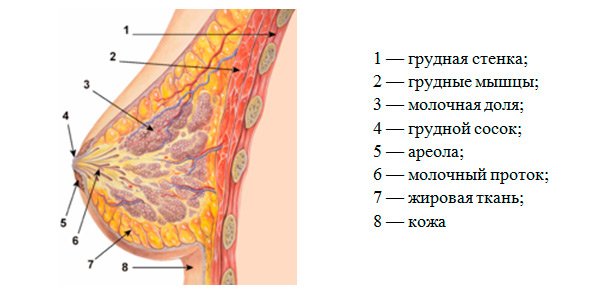
Breastfeeding: benefits for the uterus

The phrase “contraction of the uterus” means not only its return to its “pre-pregnancy” size. After childbirth, the internal surface of the organ is a wound surface covered with gaping vessels, remnants of fetal membranes, placenta, and blood clots. During recovery, the blood vessels heal, and all other formations resolve and come out in the form of lochia. To prevent discharge from accumulating in the uterus, causing inflammation, it must actively contract, which is what happens if the baby latches onto the nipple correctly. Most of the areola should be in the baby's mouth. And the more often the baby is put to the breast, the faster the uterus is restored.
If the baby takes the breast incorrectly, the effect is reduced. To avoid mistakes, you need to seek help from a midwife, pediatrician or lactation consultant.
Breastfeeding: back in shape
Getting back into shape after pregnancy, which is the dream of all women, will be easier if breastfeeding continues for more than six months. To make sure of this, you need to be patient and not make hasty conclusions if in the first weeks after birth the weight not only does not decrease, but, on the contrary, increases. This happens to many, however, after stepping on the scales after a month or two or three, the woman will notice that she has lost weight without additional effort.

The hormonal background that is established during feeding helps speed up metabolism. As a result, fats are processed faster and do not have time to be stored in reserve. A proper diet also contributes to changes: if a mother does not want her baby to cry in pain due to increased gas formation, she will refuse foods that cause this process - flour and sweets. And in order to provide the baby with vitamins and microelements, he will lean on fresh, unrefined foods - cereals, vegetables, fish, meat. The longer the lactation, the more active the favorable metamorphoses occur. When a breastfed baby turns 6 months old, his mother's sugar levels will decrease, which will have a beneficial effect on insulin secretion and reduce the risk of diabetes.
THIS IS A FACT A study of American doctors, covering almost 140 thousand medical histories of women over 50 years of age, showed: those who practiced breastfeeding for only three months, even after many years, have low blood cholesterol levels and stable blood pressure. And those who breastfed their baby for a year or longer had a 12% lower risk of hypertension and a 9% lower risk of myocardial infarction and stroke.
Weight loss is especially active when breastfeeding a baby at the age of 6–9 months. It is at this point that most young mothers return to their pre-pregnancy forms.
Database
At the time of birth, about 1 million follicles are stored in the girl’s ovaries, producing eggs from which the baby develops during fertilization. By the age of menarche (first menstruation), the resource is already several orders of magnitude smaller - about 300 thousand. Subsequently, losses accelerate, with each menstruation another group dies.

When the eggs are completely gone, the woman will lose the ability to become a mother and will begin menopause with all the ensuing consequences. The main one is a decrease in the production of estrogen, which protects bones from calcium leaching, and the heart and blood vessels from diseases. After all, the less of this hormone in the body, the greater the risk of developing a heart attack, stroke, osteoporosis, as well as increased blood pressure and cholesterol levels. With the loss of estrogen, the aging process becomes more active. For those who do not violate the “biological plan”, this process starts later and does not accelerate, since menstruation does not resume for a longer time, that is, the eggs do not mature, do not die, and the ovaries receive a break. A young mother who quickly weans her baby from the breast or does not even start breastfeeding misses the opportunity to give the ovaries a break, dooming them to quickly deplete their reserves.
A young mother who puts her baby to her breast on demand, but at least 6 times a day, may not have menstruation for six months. As soon as lactation begins to subside, the cycle will be restored. But no matter how long the period of ovarian inactivity lasts, it will have a positive effect on health.
Breastfeeding: prevention of “bad formations”
Some women believe that by interrupting breastfeeding they will preserve the appearance of the gland. Give up vain hopes: no matter how long you fed your baby or whether you did it at all, after 9 months of gestation your breasts will look different. But after a rapid cessation of lactation, it is more difficult to restore shape. As well as ensuring that the glands remain healthy. Successful and prolonged lactation will help the lumps to resolve, and interrupted lactation at the very beginning will increase the likelihood of their occurrence. Experienced mammologists, when detecting benign formations in the mammary gland, often advise women of reproductive age not to visit a surgeon, but to start a new pregnancy.

The use of medications that interrupt lactation increases the risk of developing diabetes.
Doctor's advice
If the baby has already been born and you feel that you are not ready to be a mother, do not give up breastfeeding under any circumstances. This is what will help you overcome the first adversity and doubts. By putting your baby to your breast, you establish contact with him, reduce the distance, gain confidence in your abilities and literally learn to love your child. In itself, this feeling comes only to a few. The rest are learning it. By taking the baby in your arms and placing it on your chest, you overcome the internal barrier and reach another level of relationship.










