Pleurisy, what is it? Causes and treatments
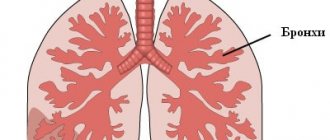
Pleurisy is an inflammation of the serous membranes that cover the outside of the lungs. This disease occurs very often. This is the most commonly diagnosed lung pathology. In the general structure of population morbidity, pleurisy accounts for 5-15%. The incidence rate varies from 300 to 320 cases per 100 thousand people. Men and women suffer from this disease equally often. Pleurisy in children is diagnosed less frequently than in adults.
An interesting fact is that women are most often diagnosed with so-called tumor pleurisy. It develops against the background of various neoplasms of the genital organs and breasts. As for men, effusion pleurisy often occurs with pathology of the pancreas and rheumatoid arthritis. In most cases, bilateral or unilateral pleurisy is secondary.
Causes
The causes of pleurisy can be divided into infectious and aseptic or inflammatory (non-infectious).
Non-infectious pleurisy usually occurs
- for rheumatoid arthritis,
- with vasculitis (vascular damage),
- for rheumatism,
- with systemic lupus erythematosus,
- with scleroderma,
- as a result of pulmonary embolism and pulmonary edema,
- with pulmonary infarction,
- when metastasis of lung cancer into the pleural cavity,
- with a primary malignant tumor of the pleura – mesothelioma,
- lymphoma,
- during hemorrhagic diathesis (clotting disorders),
- during leukemia,
- with a tumor process of the ovaries, breast cancer as a result of cancer cachexia (terminal stage of cancer),
- with myocardial infarction due to congestion in the pulmonary circulation.
- for acute pancreatitis.
Infectious diseases include:
- syphilitic or tuberculous pleurisy,
- parasitic (echinococcal or amoebic),
- pleurisy in particularly dangerous infections (tularemia, brucellosis, caused by the typhoid microbe or occurring with typhus),
- microbial pleurisy (infection of the pleural cavity with staphylococci, Escherichia coli and Pseudomonas aeruginosa, pneumococci, etc.)
- viral pleurisy (occurring when affected by the influenza virus, herpes),
- fungal pleurisy (damage to the pleura by candidiasis, coccidiosis, blastomycosis),
- pleurisy, which occurs during wounds or operations on the chest, due to microbes entering the pleural cavity.
Forms and types of pleurisy
There are 2 forms of pleurisy:
- effusion (also known as exudative)
- dry (or fibrinous)
As the disease develops, its initial nature may change. When the exudate resolves, a clinical picture of dry or adhesive pleurisy appears, and adhesions form between the visceral and parietal layers of the pleura.
Exudative pleurisy, according to the nature of the effusion, can be divided into the following types:
- serous
- serous-fibrinous
- putrefactive
- purulent
- pseudochyleous
- frail
- hemorrhagic
- mixed

Effluent pleurisy , in turn, is divided into the following forms:
- free
- encysted
Based on the type of causative agent, pleurisy can be divided into:
- specific (pathogens: spirochete pallidum, mycobacterium tuberculosis, etc.)
- infectious nonspecific (can be caused by staphylococci, pneumococci, etc.)
According to localization, pleurisy is divided into:
- costal (in the costal part of the pleura)
- apical (apical)
- paramediastinal
- diaphragmatic
- costodiaphragmatic
Also, according to prevalence, the process is divided into unilateral and bilateral.
Classification
In clinical practice, it is customary to distinguish several types of pleurisy, which differ in the nature of the effusion formed in the pleural cavity and, accordingly, in the main clinical manifestations.
- Dry (fibrinous) pleurisy . Develops at the initial stage of inflammatory damage to the pleura. Often, at this stage of pathology, there are still no infectious agents in the lung cavity, and the changes that occur are due to the reactive involvement of blood and lymphatic vessels, as well as an allergic component. Due to an increase in vascular permeability under the influence of pro-inflammatory substances, the liquid component of plasma and some proteins begin to leak into the pleural cavity, among which fibrin is of greatest importance. Under the influence of the environment in the inflammatory focus, fibrin molecules begin to unite and form strong and adhesive threads that are deposited on the surface of the serous membrane.
- Purulent pleurisy . Purulent exudate accumulates between the layers of the serous membrane of the lung. This pathology is extremely severe and is associated with intoxication of the body. Without proper treatment, it poses a threat to the patient's life. Purulent pleurisy can form either due to direct damage to the pleura by infectious agents, or due to the spontaneous opening of an abscess (or other accumulation of pus) of the lung into the pleural cavity. Empyema usually develops in debilitated patients who have serious damage to other organs or systems, as well as in people with reduced immunity.
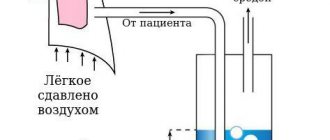
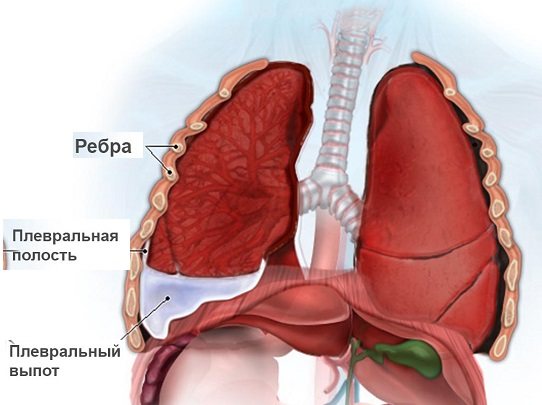
- Exudative (effusion) pleurisy . It represents the next phase of the development of the disease after dry pleurisy. At this stage, the inflammatory reaction progresses, and the area of the affected serous membrane increases. The activity of enzymes that break down fibrin threads decreases, and pleural pockets begin to form, in which pus can subsequently accumulate. The outflow of lymph is disrupted, which, against the background of increased fluid secretion (filtration from dilated blood vessels at the site of inflammation), leads to an increase in the volume of intrapleural effusion. This effusion compresses the lower segments of the lung on the affected side, which leads to a decrease in its vital volume. As a result, with massive exudative pleurisy, respiratory failure may develop - a condition that poses an immediate threat to the patient’s life. Since the fluid accumulated in the pleural cavity reduces to some extent the friction between the layers of the pleura, at this stage the irritation of the serous membranes and, accordingly, the intensity of the pain is somewhat reduced.
- Tuberculous pleurisy . It is often placed in a separate category due to the fact that this disease is quite common in medical practice. Tuberculous pleurisy is characterized by a slow, chronic course with the development of a syndrome of general intoxication and signs of damage to the lungs (in rare cases, other organs). The effusion from tuberculous pleurisy contains a large number of lymphocytes. In some cases, this disease is accompanied by the formation of fibrinous pleurisy. When the bronchi melt by an infectious focus in the lungs, specific curdled pus, characteristic of this pathology, can enter the pleural cavity.
This division in most cases is rather arbitrary, since one type of pleurisy can often transform into another. Moreover, dry and exudative (effusion) pleurisy are considered by most pulmonologists as different stages of one pathological process. It is believed that dry pleurisy initially forms, and effusion develops only with further progression of the inflammatory reaction.

Tuberculous pleurisy
Description
Tuberculous pleurisy is an inflammation of the pleura as a result of exposure to toxic substances, tissue decay products, or its specific damage with the formation of a tubercle, caseous foci when the process spreads from the lung or from the intrathoracic lymph nodes by contact, lymphogenous or hematogenous route. Symptoms See Pleurisy. Diagnosis The detection of mycobacteria in the exudate is of important diagnostic significance. However, when their number is small, the results of bacterioscopic examination are usually negative. Most often, MT is found when exudate is inoculated on special nutrient media and when inoculated into guinea pigs. Purulent pleurisy is the result of suppuration of serous fibrinous exudate or an acute primary purulent process due to pleural coseosis. An extremely serious condition is observed in patients with pleural empyema, which rapidly develops as a result of a violation of the integrity of the cavity. Mycobacteria are found in purulent fluid in 65–90% of cases. Hemorrhagic pleurisy is rare and occurs mostly with severe specific damage to the pleura with the development of a miliary or caseous process. In a number of patients, hemorrhagic pleurisy is discovered after a long-standing rigid pneumothorax ceases. Sometimes, to establish an etiological diagnosis, in addition to examining the exudate, a pleural biopsy is used. Some forms of tuberculous pleurisy occur most often in children and young people. Treatment See Respiratory tuberculosis
Symptoms
The clinical picture of pleurisy is divided into dry and exudative.
Symptoms of exudative pleurisy:
- general malaise, lethargy, low-grade fever;
- chest pain, shortness of breath intensify, a gradual increase in fever - this happens due to the collapse of the lung, the mediastinal organs are compressed.
Acute serous pleurisy usually has a tuberculous origin and is characterized by three stages:
- In the initial period (exudative), smoothing or even bulging of the intercostal space is noted. The mediastinal organs are shifted to the healthy side under the influence of a large amount of fluid in the pleural fissure.
- The stabilization period is characterized by a decrease in acute symptoms: the temperature drops, chest pain and shortness of breath disappear. At this stage, pleural friction may appear. In the acute phase, a blood test shows a large accumulation of leukocytes, which gradually returns to normal.
- It often happens that fluid accumulates above the diaphragm, so it is not visible with a vertical x-ray. In this case, it is necessary to conduct the study in a lateral position. Free fluid moves easily in accordance with the position of the patient's torso. Often its accumulations are concentrated in the cracks between the lobes, as well as in the area of the diaphragm dome.
Symptoms of dry pleurisy:
- chest pain;
- general unhealthy condition;
- dry cough;
- low-grade body temperature;
- local pain (depending on the location of the lesion);
- When palpating the ribs, deep breathing, and coughing, the pain intensifies.
In the acute course of the disease, the doctor diagnoses pleural noise by auscultation, which does not stop after pressing with a stethoscope or coughing. Dry pleurisy, as a rule, goes away without any negative consequences - of course, with an adequate treatment algorithm.
Acute symptoms, in addition to the described serous pleurisy, include purulent forms - pneumothorax and pleural empyema. They can be caused by tuberculosis and other infections.
Purulent pleurisy is caused by pus entering the pleural cavity, where it tends to accumulate. It should be taken into account that non-tuberculous empyema can be treated relatively well, but with an inadequate algorithm of action it can develop into a more complex form. Tuberculous empyema is severe and can be chronic. The patient loses significant weight, suffocates, experiences constant chills, and suffers from coughing attacks. In addition, the chronic form of this type of pleurisy causes amyloidosis of internal organs.
If optimal care is not provided, complications arise:
- respiratory arrest;
- spread of infection throughout the body through the bloodstream;
- development of purulent mediastinitis.
Diagnostics
The primary task in diagnosing pleurisy is to determine the location and cause of the inflammation or tumor. To make a diagnosis, the doctor studies the medical history in detail and conducts an initial examination of the patient.
Basic methods for diagnosing pulmonary pleurisy:
- Blood tests can help determine whether you have an infection, which may be the cause of pleurisy. In addition, blood tests will show the state of the immune system.
- A chest x-ray will determine if there is any inflammation of the lungs. A chest x-ray may also be taken with the patient lying down, which will allow the free fluid in the lungs to form a layer. A supine chest x-ray should confirm whether there is any fluid buildup.
- A computed tomography scan is performed if any abnormalities are found on a chest x-ray. This analysis presents a series of detailed, cross-sectional images of the chest. The images produced by a CT scan create a detailed picture of the inside of the breast, allowing your doctor to get a more detailed analysis of the irritated tissue.
- During a thoracentesis, the doctor will insert a needle into the chest area to test for fluid. The fluid is then removed and analyzed for infections. Due to its invasive nature and associated risks, this test is rarely done for a typical case of pleurisy.
- During a thoracoscopy, a small incision is made in the chest wall and a tiny camera attached to a tube is then inserted into the chest cavity. The camera locates the irritated area so a tissue sample can be taken for analysis.
- A biopsy is useful in the development of pleurisy in oncology. In this case, sterile procedures are used and small incisions are made in the skin of the chest wall. An X-ray or CT scan can confirm the exact location of the biopsy. A doctor may use these procedures to insert a lung biopsy needle between the ribs and into the lung. A small sample of lung tissue is then taken and the needle is removed. The tissue is sent to a laboratory where it will be analyzed for infections and abnormal cells consistent with cancer.
- Using ultrasound, high-frequency sound waves create an image of the inside of the chest cavity, which will allow you to see if there is any inflammation or fluid build-up.
As soon as the symptoms of pleurisy are identified, treatment is prescribed immediately. The first place in treatment is antibiotics against infection. In addition to this, anti-inflammatory drugs or other painkillers are prescribed. Sometimes cough medicine is prescribed.

Treatment of pleurisy
Effective treatment of pleurisy depends entirely on the cause of its occurrence and consists mainly in eliminating the unpleasant symptoms of the disease and improving the patient’s well-being. In case of a combination of pneumonia and pleurisy, treatment with antibiotics is indicated. Pleurisy, which accompanies systemic vasculitis, rheumatism, scleroderma, is treated with glucocorticoid drugs.
Pleurisy that occurs against the background of tuberculosis is treated with isoniazid, rifampicin, and streptomycin. Typically, such treatment lasts for several months. In all cases of the disease, diuretic, painkillers and cardiovascular drugs are prescribed. For patients who do not have any special contraindications, physical therapy and physiotherapy are indicated. Often, in the treatment of pleurisy, in order to prevent relapses of the disease, obliteration of the pleural cavity or pleurodesis is performed - the introduction of special “gluing” preparations into the pleural cavity.
The patient is prescribed analgesics, anti-inflammatory drugs, antibiotics, and drugs to combat cough and allergic manifestations. For tuberculous pleurisy, specific therapy with anti-tuberculosis drugs is carried out. For pleurisy resulting from a tumor of the lung or intrathoracic lymph nodes, chemotherapy is prescribed. Glucocorticosteroids are used for collagen diseases. If there is a large amount of fluid in the pleural cavity, a puncture is indicated to suction out the contents and administer medications directly into the cavity.
During the rehabilitation period, breathing exercises, physiotherapeutic treatment, and restorative therapy are prescribed.
Treatment
It is important to start with treating the disease that led to pleurisy. With dry pleurisy, chest pain can be reduced by bandaging the chest with an elastic bandage. It is recommended to bandage a pillow to the sore side to enhance local immobilization. The patient needs to be bandaged 1-2 times a day to prevent hypostatic phenomena in the lungs and irritation of the skin. For a dry, painful cough, the person should be prescribed antitussive medications, for example, prenoxdiazine or codeine.
Pleural puncture is necessary if there is fluid in the pleural cavity until the cause of the disease is determined. Antibacterial therapy is necessary if the nature of pleurisy is infectious. Gram smear bacterioscopy allows you to roughly determine the pathogen. Treatment of tuberculous pleurisy is carried out with three or more tuberculostatic drugs simultaneously in combination with pathogenetic therapy and pleural punctures.
If the effusion is significant, it is necessary to include diuretics in the treatment regimen. Furosemide is prescribed in most cases; it can be combined with spironolactone. In some cases of pleurisy of an infectious nature, anti-inflammatory drugs are needed, as in Dressler's syndrome and systemic connective tissue diseases. The use of non-steroidal anti-inflammatory drugs or glucocorticoids is relevant.
To treat pleural empyema, drainage of the pleural cavity and adequate antibiotic therapy are effective. At the early stage of fibrinous pleurisy, it is recommended to carry out alcohol warming compresses and electrophoresis with calcium chloride. Physiotherapy is prescribed at the stage of resolution of exudative pleurisy in order to speed up the resorption of exudate and reduce pleural adhesions. Electrophoresis with heparin, calcium chloride, magnetic therapy, and paraffin therapy are effective.
Prevention
Of course, it is impossible to predict how the body will react to the action of a particular factor. However, anyone can follow simple recommendations for the prevention of pleurisy:
- First of all, complications should not be allowed during the development of acute respiratory infections. To prevent pathogenic microflora from penetrating the mucous membrane of the respiratory tract, and then into the pleural cavity, colds cannot be left to chance!
- For frequent respiratory tract infections, it is good to change the climate for a while. Sea air is an excellent means of preventing respiratory tract infections, including pleurisy.
- If pneumonia is suspected, it is better to take a chest x-ray in a timely manner and begin adequate therapy. Improper treatment of the disease increases the risk of complications in the form of inflammation of the pleura.
- Try to strengthen your immune system. In the warm season, do hardening, spend more time in the fresh air.
- Stop smoking. Nicotine becomes the first cause of the development of pulmonary tuberculosis, which in turn can provoke inflammation of the pleura.
- Do breathing exercises. A couple of deep breaths after waking up will serve as an excellent prevention of the development of inflammatory diseases of the respiratory system.
Pleurisy
Description
Pleurisy is an inflammation of the pleura with the formation of fibrinous plaque on its surface or effusion in its cavity. - Dry pleurisy - Exudative pleurisy - Exudative pleurisy It is always secondary, it is a syndrome or complication of many diseases, but at a certain period it can come to the fore in the clinical picture, masking the underlying disease. Etiology, pathogenesis The occurrence of pleurisy of an infectious nature is due to the inaction of pathogens of specific (mycobacterium tuberculosis, Treponema pallidum) and nonspecific (pneumococci, staphylococci, E. coli, viruses, fungi, etc.) infections; pathogens penetrate into the pleura by contact, lymphogenously, hematogenously, when the pleural cavity is disrupted. A common cause of pleurisy is systemic connective tissue diseases (rheumatism, systemic lupus erythematosus, etc.); neoplasms; thromboembolism and thrombosis of the pulmonary arteries. Pathogenesis Most pleurisy is allergic. In the development of blastomatous pleurisy, the blocking of lymph nodes, lymphatic and venous vessels by tumor metastases is of great importance; when the tumor grows from adjacent organs, destruction of the serous integument occurs. Symptoms Symptoms and course are determined by the localization, prevalence, nature of inflammation of the pleura, changes in the function of neighboring organs. The main forms of pleurisy: dry, or fibrinous, effusion, or “exudative”. Exudative pleurisy, in turn, is divided according to the nature of the effusion into serous, serous fibrinous, purulent, hemorrhagic, chylous, and mixed. Having determined the nature of the effusion, it is possible to clarify the cause of the development of pleurisy and choose pathogenetic therapy. Thus, the cause of dry and serous, serous fibrinous pleurisy is more often tuberculosis, pneumonia (parapneumonic, metapneumonic pleurisy), rheumatism and other systemic connective tissue diseases (rheumatic, lupus and other pleurisy). Hemorrhagic pleurisy most often develops with neoplasms, thromboembolism and thrombosis of the pulmonary vessels, hemorrhagic diathesis, influenza, and less often with tuberculosis and rheumatism. Based on the location of the effusion, they are classified into paracostal, diaphragmatic, paramediastinal, and interlobar. Dry pleurisy Symptoms The main symptom is pain in the side, aggravated by inhalation and coughing. Pain is reduced by lying on the affected side. There is a noticeable limitation in the respiratory mobility of the corresponding half of the chest; with unchanged percussion sound, weakened breathing may be heard due to the patient sparing the affected side, and pleural friction noise. Body temperature is often subfebrile, there may be chills, night sweats, and weakness. Diagnosis of diaphragmatic dry pleurisy is difficult. They are characterized by pain in the chest, hypochondrium, in the area of the lower ribs, hiccups, abdominal pain, flatulence, tension in the abdominal muscles, pain when swallowing. A type of chest breathing involving only the upper part of the chest and increased pain in the lower part with a deep breath. Pain points are identified: between the legs of the sternocleidomastoid muscle, in the first intercostal spaces near the sternum, at the place of attachment of the diaphragm to the ribs, on the spinous processes of the first cervical vertebrae. X-ray examination helps in recognizing diaphragmatic pleurisy, which reveals indirect symptoms of functional disorders of the diaphragm: its high standing, limitation of its mobility on the affected side (Williams' symptom). Prognosis The course is favorable, the duration of the disease is 10–14 days, but relapses of dry pleurisy are possible over several weeks with rapid recovery. Exudative pleurisy Symptoms At the beginning of pleural exudation, pain in the side, limited respiratory mobility of the affected side of the chest, and pleural friction noise are noted. A dry, painful cough of a reflex nature often occurs. As the effusion accumulates, the pain in the side disappears, sensations of heaviness, increasing shortness of breath, moderate cyanosis, some bulging of the affected side, and smoothing of the intercostal spaces appear. Percussion reveals a dull sound above the exudate; vocal tremor and bronchophony are weakened, breathing is not carried out or is significantly weakened; above dullness - a tympanic tone of percussion sound, a bronchial tone of breathing and fine bubbling rales. With percussion and x-ray examination, a characteristic contour of the upper border of the effusion can be determined. Large effusion causes a shift of the mediastinum to the healthy side and significant impairment of the function of external respiration due to disruption of respiratory mechanics: the depth of breathing decreases, it becomes more frequent; functional diagnostic methods reveal a decrease in external respiration indicators (vital capacity of the lungs, ventilation reserves, etc.). Disorders of the cardiovascular system occur: a decrease in stroke and cardiac output due to a decrease in blood suction into the central veins due to ventilation disorders, displacement of the heart and large vessels with large pleural effusions; compensatory tachycardia develops, blood pressure tends to decrease. Exudative pleurisy Characterized by febrile body temperature from the very beginning of pleural exudation, severe symptoms of intoxication, neutrophilic leukocytosis, and increased ESR. Pleural exudate has a relative density higher than 1016–1018, is rich in cellular and elements, and gives a positive Rivalta reaction. The tumor etiology of pleurisy is excluded by cytological examination of the exudate. The course depends on the etiology of pleurisy. In case of infectious-allergic pleurisy, including tuberculosis, the exudate can resolve within 2–4 weeks. An outcome is possible with the development of an adhesive process in the pleural cavity, fusion of the pleural cavities and interlobar fissures, the formation of massive overlays, moorings, thickening of the pleura, the formation of pleuropneumocirrhosis and respiratory failure. (For purulent pleurisy, see Pleural empyema) Treatment Comprehensive, includes active treatment of the underlying disease and early vigorous treatment of pleurisy; for effusion pleurisy, it is carried out in a hospital. Treatment consists of the following components: Antibacterial therapy for infectious-allergic pleurisy and targeted chemotherapy for pleurisy of other etiologies (for example, tumor); Antibiotics and chemotherapy drugs are administered parenterally, and if indicated, intrapleurally. Sanitation of the pleural cavity by evacuation of exudate, and, if necessary, rinsing with antiseptic solutions. Indications for urgent evacuation: displacement of the heart and large vessels to the healthy side with severe impairment of cardiac function, lung collapse (severe shortness of breath, cyanosis, rapid small pulse, arterial hypotension). Non-urgent indications: sluggish, protracted course of pleurisy, lack of tendency for exudate to resolve. Prescription of desensitizing and anti-inflammatory drugs (sodium salicylate and other salicylic acid preparations, butadione or phenylbutazone, amidopyrine, calcium chloride). For pleurisy of tuberculous and rheumatic etiology, the use of prednisolone in a daily dose of 15–20 mg is effective. Inclusion of means aimed at mobilizing protective immunobiological reactions of the body: individual regimen (in the acute period, bed rest), a rational fortified diet with a sufficient amount of protein (1.5–2 g/kg), restriction of water and table salt, parenteral administration of ascorbic acid, group vitamins B, intravenous drip injections of plasma-substituting solutions, individually dosed physical therapy, oxygen therapy, and during the period of pleurisy subsiding - physical methods of treatment. Symptomatic therapy - warm compresses, mustard plasters, immobilization of the diseased half of the chest with tight bandaging (for pain), codeine, ethylmorphine hydrochloride for coughing; cardiotonic drugs for circulatory failure. In the future, patients are subject to clinical observation for 2–3 years. Occupational hazards are excluded, a high-calorie diet rich in vitamins is recommended.
Forecast
The prognosis for pleurisy is favorable, although it directly depends on the underlying disease. Inflammatory, infectious, post-traumatic pleurisy can be successfully cured and does not affect the quality of future life. Unless, during the rest of your life, pleural adhesions will be noted on radiographs.
The exception is dry tuberculous pleurisy, as a result of which fibrous deposits can calcify over time, forming the so-called armored pleurisy. The lung becomes encased in a “stone shell,” which interferes with its full functioning and leads to chronic respiratory failure.
To prevent the formation of adhesions that form after removal of fluid from the pleural cavity, after treatment, when the acute period subsides, the patient should undergo rehabilitation procedures - this is physiotherapy, manual and vibration massage, daily breathing exercises are required (according to Strelnikova, using a Frolov breathing simulator) .