Causes of increased blood levels
The reasons for the increase in segmented neutrophils in the blood are very different. Numerous studies have shown that their high activity is observed during bacterial infection. The function of these cells is to identify, subsequently engulf and digest the infectious agent through phagocytosis.
An increase in segmented neutrophils is observed in the following situations:
- otitis media, bronchitis, pneumonia, tonsillitis and other bacterial infections;
- allergic diseases, diabetes mellitus, various metabolic disorders;
- autoimmune group of pathologies: rheumatism, lupus erythematosus, rheumatoid arthritis;
- purulent-septic conditions;
- psoriasis, dermatitis and other skin problems;
- open extensive damage to the skin - burns, trophic ulcers;
- diseases of the circulatory system, bone marrow.
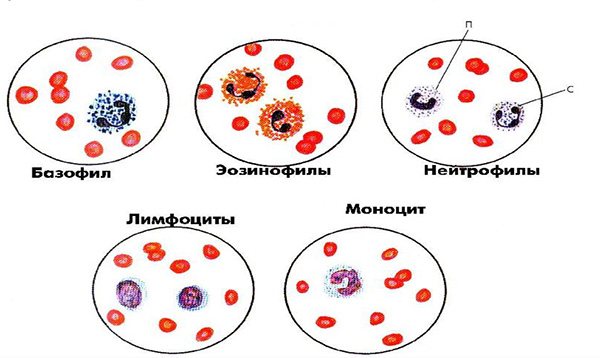
There are other causes of neutrophilia - this is the term used in the medical literature when an increased number of neutrophils is present in the tests. Segmented representatives are mature forms that perform the entire range of intended functions. They are also called granulocytes due to the content of specific inclusions with biologically active components in their structure.
What does a reduced level of segmented neutrophils in a child indicate? Reasons for the increase in band neutrophils in the blood of an adult.
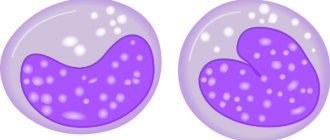
Segmented neutrophil under a microscope
Why are immature band neutrophils needed?
In human blood, young leukocyte bodies are present in small quantities. Despite the fact that they are not completely ripe, they are still capable of performing minor protective functions. Band neutrophils do not yet absorb small foreign particles, microbes, bacteria and do not have enzymes that carry out phagocytosis.
It is important to note that segmented bodies are capable of destroying infection that spreads in the patient’s organs and tissues. They penetrate the walls of blood vessels and reach the site of inflammation only by acquiring a core divided into segments. But rod species do not have this ability, so they are always diagnosed only in the bloodstream.
After the immunocompetent cells of the segmented type digest the pathogen, they die. Therefore, constant production of white blood cells is required to kill infections. During a massive attack on the body, the bone marrow produces them in large quantities, which is why a high concentration of immature elements is found in the blood of a sick person.
The breakdown products of neutrophil cells cause tissue softening. This is how purulent exudate is formed, which can be seen on the face in the form of boils or pimples, as well as in wounds where infection occurs. The formation of pus can indicate the activity of leukocytes.
What does this mean if neutrophils are low?
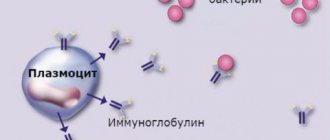
In certain situations, the following picture is observed: against the background of an increase in segmented neutrophils in the blood, there is a decrease in the level of lymphocytes - other representatives of the leukocyte fraction. They, in turn, are responsible for fighting viral and fungal infections, as well as tumor cells. A similar imbalance is present in hematological diseases and taking glucocorticosteroids.
Severe viral diseases, congenital and acquired immunodeficiencies, and malignant neoplasms can lead to a decrease in the number of lymphocytes. If, against this background, an inflammatory process occurs, especially of a purulent nature, a blood test shows an increased level of neutrophils.
What are neutrophils?
Before moving on to the question of what neutrophils are and why their level is elevated, we note that blood consists of red and white blood cells. White cells - leukocytes - are responsible for fighting infection. Experts divide them into several groups, which are differentiated by the color obtained after treatment with a special coloring composition. Neutrophils are white blood cells that react to any type of dye reagent.
Among white cells, the content of neutrophils is approximately 50%, although this figure varies depending on the age of the patient. These bodies perform the task of capturing the emerging infection and destroying it. Band nuclei in the total number of neutrophils are only from 1 to 6%.

Stages of neutrophil development
Neutrophils are produced in the bone marrow. These bodies are divided according to their age:
- myelocytes – newly emerged neutrophils;
- metamyelocytes are also early leukocytes, slightly older than the previous type;
- band neutrophils – the next oldest neutrophils;
- segmented.
There should be no young myelocytes and metamyelocytes in human blood. They are required to undergo the procedure of full maturation and only after that enter the vessels and arteries. But it doesn't always work out that way. Mature neutrophils self-destruct when fighting infection.
If the disease is not defeated, the rod cells have to enter the fight. As a result, their levels become elevated. And behind them, metamyelocytes and myelocytes may appear in the blood. The norm of leukocytes in the blood of a woman, man and child.
Neutrophils stay in the body for only 2 weeks. The period of formation of these leukocytes in the bone marrow takes 6 days. Then they move into the blood, where they travel for no more than 10 hours. In the next period of life, the corpuscles are found in tissues and organs, where for a week they perform the main function of counteracting infection.
Another feature of neutrophils is the presence of enzyme granules in their plasma. As part of these leukocytes, the granules are assigned the most important functions. They contain 2 dozen active substances that do the job of destroying the infection.
In addition to destroying pathogenic microorganisms, neutrophils secrete cytokines that notify the cells of the human body about the presence of infection.
Increase in lymphocyte agranulocytes in an adult
The presence of a focus of infection is what is most often indicated by the condition when an increased level of neutrophils is detected in an adult. With age, the immune system becomes more stable, therefore, as a rule, it is less susceptible to colds and sore throats. But there is a certain list of diseases that are much more common in adults than in children:
- Inflammatory diseases of internal organs. Most often this is the appendix, gallbladder, pancreas, fallopian tubes. Segmented neutrophils are most significantly increased in purulent inflammation.
- Thrombophlebitis - usually affects the veins of the lower extremities. The precursor to the pathology is varicose veins, the risk of which increases as the body ages.
- Heart failure, heart attacks, strokes. All these conditions threaten older people. An increase in segmented neutrophils in such cases is not a diagnostically significant criterion.
- Oncological diseases.
In adulthood, hormonal drugs are more often prescribed. The level of segmented neutrophils in adults is increased, and the level of lymphocytes is decreased. This is due to the fact that glucocorticosteroids reduce the production of lymphocytes, while stimulating the release of neutrophils from the bone marrow into the peripheral blood.
Blood cells
How to reduce the high percentage of neutrophils in the blood of an adult?
Therapeutic prescriptions depend on the specific lesion of the body. In order to determine the exact cause of infection or penetration of foreign bodies, you may need to do an ultrasound of the internal organs (to diagnose inflammatory processes or pathological changes), CT scan (to identify tumors).
They also take a stool test (assess the condition of the mucous membranes of the gastrointestinal tract and the presence of worms), urine (determine neutrophilia in the urinary system), and a gynecological smear (infections in the reproductive system). If pathogenic microbes are suspected of settling in the respiratory organs, bacterial culture is performed.
Once a diagnosis is made, therapy can be prescribed to reduce neutrophilia. If the disease is infectious, then it is carried out with several types of drugs:
Antibiotics;
They destroy bacteria, prevent the development of purulent formation, and relieve the inflammatory process. To reduce the symptoms of inflammation, antibacterial agents are used to which microbes have not developed resistance. And such a factor is revealed by bacterial culture and determination of the sensitivity of the pathogen to a specific group of drugs (cephalosporins, macrolides, tetracyclines, etc.).
Immunostimulants;
Prescribed as antiviral drugs. They boost the immune system and stimulate its activity in order to quickly overcome the infection. The mobilization of protective forces is carried out by Immunal, Timalin and similar means. Immunostimulants are also required for recurrent diseases.
Corticosteroids;
Used to relieve inflammation. Hormonal drugs should not be used for a long time, as they can cause serious side effects. But the correct dosage and duration of treatment helps relieve inflammation and relieve symptoms. Prednisolone, Dexamethasone, etc. are often used.
If neutrophilia is provoked by other diseases or pathologies, then medications are prescribed on an individual basis.
Change during pregnancy
Pregnant women may experience an increased number of white blood cells. This is explained by the fact that the child’s gene composition is only half the same as the mother’s. It is foreign to the body, which means it is capable of causing an immune response. This is what the increased level of segmented neutrophils in a pregnant woman indicates. This physiological reaction is mild and safe for both the mother and the fetus.
It’s another matter if the indicator is greatly increased during pregnancy or other symptoms of inflammation are present. In this case, you should urgently consult your doctor.
Increased levels during pregnancy
During pregnancy, the level of neutrophil leukocytes sometimes increases to 12x10⁹/l.
The reason is that the genetic material of the embryo is essentially an antigen and the body produces neutrophils to fight unidentified proteins. If the indicator remains markedly and persistently elevated, then the following pathologies in pregnant women are possible:
- damage to the lymphatic system;
- bacterial infection;
- food poisoning or intoxication in a pregnant woman with waste products of the fetus;
- cancer;
- blood poisoning.
Also, an increased level of band neutrophil leukocytes is observed when there is little of their segmented variety in the body. This happens with reduced immunity during pregnancy.
In a pregnant woman, the growth of band neutrophils can be observed as a reaction to changing climatic conditions. Nervous stress, physical work, a reaction to certain medications, and large blood loss can cause an increase in the rate.
Increased rate in children
An increase in segmented neutrophils in children is observed regularly. This is due to the fact that the immune system reacts more acutely to the presence of foreign agents in the body. There are a number of diseases that are inherent in childhood. The most common ones are listed below:
- sore throat, tonsillitis;
- scarlet fever;
- meningitis;
- bronchitis, pneumonia.
Segmented neutrophils are increased in various types of poisoning, which are more often the cause of the disease in children than in adults. There is such a thing as physiological neutrophilia: with nervous or physical stress, rapid temperature changes. In such situations, the level of leukocytes quickly returns to normal when conditions normalize.
You should know that until the age of five, children normally have a lower number of segmented neutrophils than lymphocytes.
Causes of neutrophilia
Physiological reasons
There is a so-called physiological neutrophilia, or pseudoneutrophilosis. Its occurrence is not associated with increased neutrophil production, but with their redistribution, i.e. a change in the ratio of the parietal and circulating pools of neutrophils towards the latter. Pseudoneutrophilia is observed under stress, intense physical activity, exposure to heat or cold, and after eating. Also, neutrophils are often increased during pregnancy and in a newborn child.
Infections in children
Due to a physiological decrease in the level of neutrophils due to leukocyte crossover, a child of preschool age (up to 5-6 years) has an increased susceptibility to bacterial infections. In children, neutrophils increase mainly with scarlet fever and streptococcal sore throat. A dangerous infection such as diphtheria is quite common in the pediatric population. Parasitic infestations (ascariasis, enterobiasis, toxocariasis) are also common among preschoolers. In these diseases, in addition to neutrophilia, high eosinophilia is observed in the blood.
Infections in adults
Most often, neutrophils are increased during bacterial infections. The main function of neutrophils is anti-infective protection of the macroorganism, namely, the destruction of bacteria. They also take part in the fight against viruses and parasites. Migrating through the vascular wall, neutrophils are directed to the site of localization of the pathogenic microorganism. By releasing cytokines and inflammatory mediators, neutrophils activate other components of the immune system (complement, T-B lymphocytes).
Neutrophil leukocytes first phagocytize (absorb) the infectious agent, then secrete degradation enzymes (lysozyme, lactoferrin, phosphatases) and reactive oxygen species (superoxide anion, hydroxyl radical, hydrogen peroxide), which contributes to the death of microorganisms. Neutrophilia increases rapidly, reaches a maximum parallel to the height of the disease, and gradually decreases after antibacterial therapy.
The most common cause of neutrophilia in adults is acute localized bacterial (pneumonia, sinusitis, pyelonephritis) or specific infections (typhoid fever). Moderate neutrophilia is typical for them. Less commonly, the cause is severe generalized infections (bacterial endocarditis, sepsis, meningococcal meningitis), characterized by high neutrophilia with a hyperregenerative or degenerative shift.
Acute surgical pathologies
Quite often, neutrophils are increased in acute abdominal pathology (cholecystitis, pancreatitis, perforation of a stomach or duodenal ulcer), purulent processes (phlegmon, abscess). Neurophilia in a child often occurs with appendicitis. An increase in the number of neutrophil leukocytes in these diseases acts as a reaction to the inflammatory process. A correlating relationship between the severity of inflammation and the degree of increase in neutrophils has been precisely established. Usually there is high neutrophilia with a degenerative shift of the leukocyte formula to the left, which quickly regresses after emergency surgery. However, neutrophils may remain within normal limits.
Tissue damage or breakdown
Such conditions include infarctions of various organs (myocardium, lungs, intestines), abdominal operations, gangrene, pancreatic necrosis. The cause of neutrophilia is stimulation by decay products of granulocytopoiesis in the bone marrow. An additional role is played by reactive neutrophilia, which occurs due to the release of large amounts of stress hormones (catecholamines, glucocorticosteroids) into the blood.
Also, the occurrence of neutrophilia in these conditions is facilitated by the addition of a secondary infection (for example, pneumonia due to pulmonary infarction). The degree of neutrophilia correlates with the volume of damaged, necrotic tissue, often reaches very high values (especially in a child), can persist for a long time, and decreases with recovery.
Rheumatological diseases
Neutrophilia can be observed in some chronic inflammatory pathologies of a rheumatic nature. There is an assumption that mediators, cytokines, and autoantibodies that are formed during rheumatic inflammation stimulate the bone marrow production of neutrophilic granulocytes. Typically, the appearance of neutrophilia along with other laboratory markers, such as an increased erythrocyte sedimentation rate and C-reactive protein, indicates an exacerbation of the disease.
After anti-inflammatory treatment, the concentration of neutrophils gradually returns to normal. In adults, especially high neutrophilia is characteristic of acute gouty attack, necrotizing vasculitis (polyarteritis nodosa, granulomatosis with polyangiitis). In a child, neutrophils are enlarged most often due to dermatomyositis.
- Joint diseases
: rheumatoid arthritis, ankylosing spondylitis (ankylosing spondylitis). - Diffuse connective tissue diseases (collagenoses)
: systemic lupus erythematosus, systemic scleroderma, Sjogren's disease. - Inflammatory bowel diseases
: Crohn's disease, ulcerative colitis. - Systemic vasculitis:
Takayasu's nonspecific aortoarteritis, Horton's giant cell arteritis.
Oncological diseases
Neutrophilia can sometimes indicate a malignant tumor. Its occurrence is promoted by two mechanisms - the breakdown of tumor tissue and the ability of some tumor cells to secrete granulocyte colony-stimulating growth factors (paraneoplastic syndrome). Neutrophilia most often occurs in patients with breast, lung, colon, and ovarian cancer. Neutrophilia increases slowly as the tumor grows, reaches moderate numbers, gradually regresses after chemotherapy, or quickly returns to normal after surgical removal of the neoplasia.
Hematological diseases
High neutrophilia is observed in oncohematological diseases. It can reach very high numbers (up to 100 thousand) in myeloproliferative diseases (acute, chronic myeloid leukemia). In lymphoproliferative pathologies (non-Hodgkin's lymphomas, lymphosarcoma), neutrophilia is slightly less pronounced and is almost always accompanied by absolute lymphocytosis. In a child, the most common cause is lymphogranulomatosis (Hodgkin's lymphoma).
In addition to neutrophilia itself, in patients with acute leukemia, a basophilic-eosinophilic association, a large number of blast cells and the absence of intermediate forms (leukemic failure) are found in the blood. The mechanism of neutrophilic leukocytosis lies in the malignant transformation of a hematopoietic stem cell. Granulocyte counts return to normal only after several courses of chemotherapy or bone marrow transplant.
Rare causes
- Endocrine disorders
: Cushing's disease or syndrome, thyrotoxic crisis. - Blood diseases
: hemolytic anemia, polycythemia vera, Addison-Birmer pernicious anemia. - Endogenous intoxication
: chronic renal failure, liver failure, diabetic ketoacidosis. - The phenomenon of bone marrow hyperactivation
: after agranulocytosis, treatment of megaloblastic anemia. - Use of medications
: adrenaline, cardiac glycosides, glucocorticosteroids, lithium. - Intoxication with mercury, lead
. - Exposure to ionizing radiation
.