Prevention
There is no specific prevention of problems with blood clotting during pregnancy.
Doctors recommend adhering to a proper daily routine, in which the woman will not experience heavy physical activity and will have enough time to sleep. It is important to saturate the diet with vitamins, especially vitamins C, B and K. Do not neglect taking folic acid
It is precisely because of disorders of folic acid metabolism that increased thrombus formation often occurs; its deficiency leads to increased vascular trauma, which increases the level of D-dimer in the blood. Diseases of the thyroid gland and kidneys increase the likelihood of hemostasis disorders, and therefore such pregnant women should visit the doctor more often and not refuse planned and additional diagnostic measures.
For information about the effect of increasing D-dimer during IVF, see below.
Research by Irish scientists
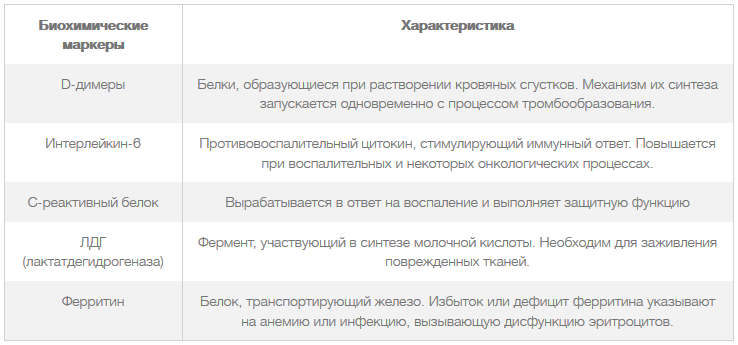
When the hypothesis arose that COVID-19 was directly related to the occurrence of problems with blood clotting that negatively affected the patient’s condition, one of the Irish hospitals decided to have each patient undergo a coagulogram.
The testing showed that in people suffering from severe coronavirus infection and requiring intensive care, coagulation factors deviated from the reference values, and especially against their background, increased D-dimer coefficients stood out. On average, scores were higher than those of individuals who did not require intensive care.
In the process of studying the results of the study and the medical history of the patients, it was found that the development of DIC syndrome is a serious predictor of death. In deceased patients, this pathology occurred in 71.4% of cases, while in survivors it occurred in only 0.6%.
In addition, a significant increase in D-dimer and prothrombin (the most important protein compound involved in the process of hemostasis) was noted with a simultaneous decrease in fibrinogen (a protein, a coagulation factor) on days 10-14 in patients with a fatal outcome.
The results of the study indicate the need for careful monitoring of blood concentrations of D-dimer, prothrombin, fibrinogen and other coagulogram parameters. Elevated levels of D-dimer (more than 1 μg/ml) are considered as a serious independent risk factor for death in patients with concomitant hemostasis disorders.
The results of the study suggested that increased coagulability may cause a decrease in oxygen content in the blood, as well as lead to other severe features of the course of coronavirus disease.
Based on these studies, it is still difficult to draw conclusions about which coagulation disorders are typical for coronavirus infection and how they can be prevented with anticoagulation therapy.
Biomarkers, the increase of which indicates a high risk of death in patients with COVID-19
Changes in protein levels during pregnancy
Blood pressure increases or decreases after eating
Table 1. D-dimer during pregnancy, reference values
In addition to pregnancy, excess of the D-dimer norm is initiated by three pathologies:
- thromboembolia;
- disseminated intravascular coagulation syndrome;
- hereditary thrombophilia;
- oncological diseases;
- over 80 years of age;
- inflammatory processes;
- infectious diseases;
- liver diseases.
It is important to note that thoughtless use of anticoagulants in this case is very dangerous. These medications lead to intense blood thinning beyond normal limits, and fibrin activity is also reduced. During pregnancy, this can lead to early placental abruption and heavy bleeding after childbirth.
According to statistics, this pathology is the most common cause of female mortality during childbirth.
During pregnancy, this can lead to early placental abruption and heavy bleeding after childbirth. According to statistics, this pathology is the most common cause of female mortality during childbirth.
When carrying several fetuses at the same time, D-dimer may be increased even more during pregnancy. This fact can make correct diagnosis difficult. Accordingly, the doctor should prescribe you medications only after confirming the source of the increase in D-dimer. With this approach to therapy, the risk of pathology is reduced.
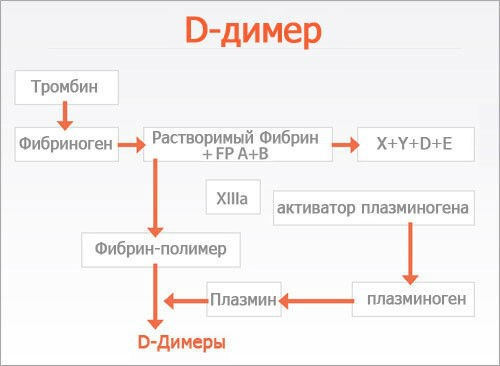
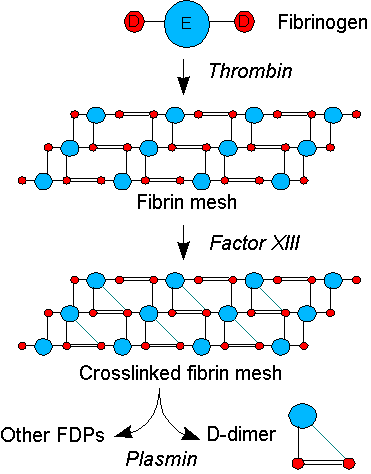
The principle of formation of D-dimer in the blood is as follows:
- in case of any damage to the tissues of blood vessels, the substance fibrinogen, which is constantly present in human blood in dissolved form, passes into a form that does not dissolve in the blood - fibrin;
- fibrin, in turn, covers the damaged area with a kind of network of long threads;
- this network retains red blood cells and platelets, which form blood clots, i.e. blood clots that prevent further blood loss;
- After the damaged tissue has finally healed, a process called fibronolysis begins, i.e. thrombus disintegration process. D-dimer is one of the elements of a broken blood clot.
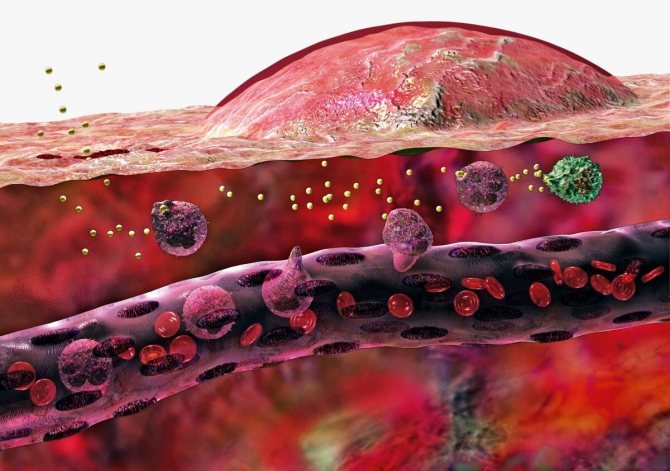
But even such a seemingly ideal natural mechanism can fail. Under certain circumstances, blood clots can form in the lumen of healthy vessels, which leads to obstruction of blood through the vessels and other diseases. A large number of articles have been written about the danger that blood clots pose to the human body.
The D-dimer level test is done by taking a blood sample from a vein.
The appearance of D-dimers in the blood plasma indicates excessively active fibrinolysis. An intensive splitting process indicates an increase in the blood clotting threshold and the accumulation of insoluble fibrin at previous stages. If, during a study of blood plasma, D-dimers are found in it, then there is an increased risk of thrombosis, and immediate measures must be taken to correct hemostasis.
Before childbirth and directly during childbirth, it reaches its maximum level, after 3 days it rapidly declines, and after 30-35 days it reaches standard values.
Normal D-dimer values by week of pregnancy in ng/ml
Pregnancy is a condition that is both physiological and pathological. The physiology of this condition is determined by the fact that the female body is naturally programmed for procreation. The pathology lies in the fact that in order to engraft a fertilized egg, the woman’s body is forced to create a state of artificial immunodeficiency.
During pregnancy, changes in the protein composition of the blood are also observed. It may also happen that D-dimer is elevated during pregnancy. This usually occurs as a result of the fact that under the influence of estrogens the synthesis of most blood proteins, including D-dimer, increases. You shouldn’t be afraid of this - the condition will go away on its own as the pregnancy resolves.
If previously the determination of D-dimer was available only to specialized clinics, then in modern medicine any medical institution providing assistance for acute pathologies of hemostasis has equipment to implement the technique. Emergency diagnostics carried out at a high level help to begin treatment in a timely manner and save the health and lives of patients.
D-dimer - what is it?
The use of D-dimer as a test for diagnosing the early stages of a blood clot has been practiced since the 90s of the last century. The method began to be used in practice as one of the main tests that makes it possible to detect conditions predisposing to the formation of blood clots at an early stage in the laboratory. Such a feature of the D-dimer as the appearance of protein compounds after the disintegration of a blood clot was known 20 years before the use of this analysis in practice, but the discovery did not receive practical significance due to the little knowledge of the method.
If previously the determination of D-dimer was available only to specialized clinics, then in modern medicine any medical institution providing assistance for acute pathologies of hemostasis has equipment to implement the technique. Emergency diagnostics carried out at a high level help to begin treatment in a timely manner and save the health and lives of patients.
D-dimer is elevated: reasons
Blood tests during pregnancy: coagulogram

The basis for an increase in the D-dimer index is usually the following factors: a large number of blood clots in the vessels, preventing the free flow of blood, severe pregnancy and the risk of its termination, atrial fibrillation and heart problems, pathological conditions of the liver and kidneys, oncology.
The D-dimer level is elevated in the following diseases:
- DIC syndrome - the formation of a large number of small blood clots in the vessels;
- renal and liver failure;
- malignant tumors;
- a large number of blood clots in the veins;
- blood clots localized in the arteries, the risk of developing gangrene, myocardial infarction, stroke, kidney damage;
- difficult course of pregnancy, toxicosis that manifests itself in later stages, high blood pressure that threatens the life of mother and child, gestosis;
- atrial fibrillation;
- internal bleeding (stomach or intestinal).
If the diagnosis of thrombosis was removed, and the D-dimer level is still above normal, this indicates the development of rheumatoid arthritis, an infectious disease, the use of drugs administered intravenously, the advanced age of the patient, cigarette abuse, and the postoperative period.

The level of increase in D-dimer is characterized by:
- area of distribution and number of blood clots formed;
- the time period that has passed since the formation of the blood clot;
- use of anticoagulants or thrombolytic drugs.
If the D-dimer is high, but other components of the coagulogram are normal, this indicates the absence of thrombosis, but the following conditions are possible:
- diseases caused by infectious lesions;
- inflammatory processes;
- autoimmune pathologies caused by malfunctions of the immune system;
- pregnancy;
- age over 50;
- smoking;
- multiple bruises;
- postoperative period.

D-dimer and the risk of heart attack are directly related.
Attention!
Clinical studies have confirmed the relationship between elevated levels of the marker and coronary heart disease, and the likelihood of an imminent stroke/heart attack.
The analysis allows you to respond in a timely manner to changes in blood composition and take measures to prevent the negative consequences of the development of thrombosis. It is necessary to undergo testing for the marker at least once a year if:
- upon reaching 50 years of age;
- with severe nicotine addiction;
- diabetes mellitus;
- high cholesterol, elevated levels of triglycerides, low-density lipoproteins;
- obesity;
- hypertension;
- an increase in CRP (a complex compound of carbohydrates and proteins produced by liver cells);
- hereditary predisposition to vascular lesions;
- frequent stressful situations;
- neglect of physical activity.
An incorrect diet with a large amount of carbohydrates provokes a deviation from the norm.
How to lower D-dimer
Correction of D-dimer cannot be done on your own. Strict medical supervision is required. Self-medication can lead to worsening of the condition. The correction method is selected taking into account the causes of the deviation, the patient’s health status and some other factors.
The main task of correction is to achieve a balance between the coagulating and pro-coagulating abilities of the blood. To achieve the goal, in addition to drug therapy, you can use traditional methods and diet.
Nutrition correction

The diet in the correction program serves as an auxiliary measure. To correct the composition of the blood, proper nutrition alone is not enough.
To reduce the coagulation element in the blood, it is recommended to include in the diet:
- lean meat (rabbit, chicken, turkey);
- sea fish (flounder, mackerel, halibut).
Omega-3 foods can help lower D-dimer levels:
- beans, soybeans;
- flax seeds;
- nuts;
- oats, wheat;
- spinach, leek;
- cauliflower;
- strawberries, raspberries;
- avocado;
- tofu cheese;
- mulberry;
- olive, rapeseed and linseed oil.
The following products have a liquefying effect:
- sunflower seeds – no more than 30 g per day;
- ginger root - add a little to tea;
- dark chocolate – up to 30 g per day;
- green onions;
- aloe juice – 1 tsp. before eating;
- vitamin complexes with a high content of vitamin E.

It is necessary to exclude from the diet foods that thicken the blood:
- bananas;
- dark buckwheat;
- chokeberry;
- nettle infusion;
- White cabbage.
On a note! If d-dimer is high, restrictions are imposed on coffee, tea, and alcoholic drinks. Fatty, fried and spicy foods, rich broths are contraindicated.
Folk remedies

Before being treated with traditional methods, it is recommended to take allergy tests. If there are no individual contraindications, you can safely use folk remedies.
Traditional recipes:
- Green tea with cinnamon and ginger. Add a couple of pieces of ginger and a pinch of cinnamon to the loose leaf tea. Pour boiling water over and leave for 10 minutes. Drink the tea warm with a little honey and a slice of lemon. 250 ml of drink per day is enough.
- Ginkgo biloba. Pour 50 g of dry leaves into 0.5 liters of boiling water. Leave for 10 minutes and then bring to a boil. Cool and strain. Drink 1 d.l. before eating. Course – 12 days.
- Horse chestnut. Pour 50 g of chestnut peel into 1 liter of boiling water. After leaving for a day, strain and add 5 tbsp. l. lemon juice. 2 tbsp. l. dilute the infusion with a glass of mineral water and drink in the morning. Course – 2 weeks. Break – 2 weeks.
- Mulberry root. Grind the fresh tree root in a blender or coffee grinder. Pour 200 g of powder into 3 liters of water and cook over low heat. Turn off the boiling broth and cool. Store the decoction in a cool place. Drink 2 tbsp. l. after breakfast and dinner.
- Tea collection. Mix dry raw materials of large-leaf black tea, wild rose petals and meadowsweet flowers. 1 tbsp. l. collection, pour a glass of boiling water. Cool and drink in small sips throughout the day.
- Raspberry jam. Eat 5-7 spoons of raspberry jam every day. Contraindications: diabetes and allergic reactions.
- Orange juice. Squeeze the juices of two oranges. Add a little cinnamon to 100 ml of juice and drink. One dose per day is sufficient.
- Cranberry and raspberry tea. Take dry berries in equal parts. Pour 1 tbsp. l. a glass of boiling water. Drink 1-2 glasses of infusion a day.
What does d-dimer show?
Why can a woman have an increased platelet count in her blood test and what does this mean for her health?

D-dimer is formed only during the breakdown of fibrin. Detection of it in the blood shows that the blood coagulation system has been launched. A very high d-dimer indicates that massive thrombosis or disseminated intravascular coagulation syndrome is occurring in the body. These conditions are very life-threatening. Thrombosis is the process of formation of blood clots in the lumen of an intact vessel. Often occurs with varicose veins of the lower extremities. There are venous thrombosis, when a blood clot forms in the veins, and arterial thrombosis, when a blood clot forms in the arteries. Disseminated intravascular coagulation syndrome or DIC is a severe pathology of the hemostatic system, characterized by massive formation of blood clots in the vascular bed. This depletes fibrin reserves in the body, the blood stops clotting and the patient dies from uncontrolled bleeding and damage to all organs. DIC syndrome often occurs as a complication of blood poisoning, infection, after surgical interventions accompanied by massive bleeding, severe injuries with extensive tissue damage (for example, 3-4 degree burns with a large area of damage). For all pathologies complicated by DIC syndrome, it is necessary to do a special analysis. D-dimer and determination of its level in the blood will prevent this complication. Positive results are also possible with:
- liver diseases;
- rheumatic diseases;
- severe inflammation;
- pregnancy;
- cancer;
- injuries.
In all these conditions, there are prerequisites for the activation of blood clotting. During pregnancy, the hemostatic system prepares to stop bleeding after childbirth, which is reflected in an increase in the level of d-dimer in the blood. There are a large number of tests that allow you to assess the state of hemostasis. D-dimer began to be determined in the 90s. This analysis quickly took the place of the main method for diagnosing thrombosis and DIC syndrome, which increased the number of favorable outcomes.
Indications for prescribing a D-dimer test
List of main indications for the study:
- suspicion of DIC syndrome;
- deep vein thrombosis of the lower extremities;
- comprehensive diagnosis of pulmonary embolism (PE);
- taking certain hormonal medications (oral contraceptives, hormone replacement therapy);
- predicting the risk of acute thrombosis in chronic heart failure, coronary heart disease, transient cerebrovascular accidents;
- condition after severe injuries;
- preparation for surgery and the postoperative period;
- therapy with anticoagulants and thrombolytic drugs for heart attacks and strokes.
Determining the presence of D-dimer during pregnancy is very important, especially if the following complications occur:
- late toxicosis of pregnancy (preeclampsia), preeclampsia, eclampsia;
- threats of miscarriage;
- a history of unsuccessful pregnancies or premature births.
This analysis can be prescribed by a cardiologist, obstetrician-gynecologist, phlebologist, general and vascular surgeon.
D-dimer indices are increased
Since a fragment of the fibrinogen molecule of the D-dimer type is a marker of the activity of the hemocoagulation capabilities of blood plasma, this testing is not a routine study in clinical laboratories.
The level is elevated in the following pathologies in the body:
- Disease thrombosis of arteries with a large diameter;
- Pulmonary artery thromboembolism disease (PE);
- Pathology of the hematopoietic system DIC syndrome.
In addition to these pathologies that threaten human life, there are physiological conditions and pathologies that provoke an increase in this marker:
- The period of intrauterine development of a child;
- Malignant neoplasms in the body;
- Thrombolytic therapy;
- Infectious pathologies of the body;
- Inflammation at the very peak of the disease;
- Damage to liver parenchyma cells;
- Thrombophilia during pregnancy;
- Pathology thrombophilia in infertility in women;
- Ischemia of the heart muscle (CHD);
- Myocardial infarction;
- Large subcutaneous hematomas;
- Injury to muscle tissue and tissue of internal organs;
- Surgical intervention in the body;
- Old age of the patient;
- Before pregnancy, restructuring in the hemostasis functioning system.
Reduction with medications if d-dimer is higher than normal
Treatment for elevated d-dimer index consists of taking anticoagulants, which block the formation of blood clots (thrombi). The purpose of these drugs is to influence the synthesis of fibrin.
If you stop the production of this substance, then the final product of its breakdown, di-dimer, will not be in the blood plasma.
Strict adherence to the individual dosages prescribed by the doctor will prevent the risk of bleeding.
Self-administration of anticoagulants is strictly prohibited. It is also prohibited to take the drugs together with the consumption of alcoholic beverages and blood-thinning drugs.
Principles
Principles of the D-dimer test
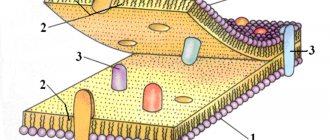
Coagulation—the formation of a blood clot or thrombus—begins when clotting proteins are activated: either by contact with a damaged blood vessel wall (the “extrinsic pathway” of coagulation) or under the influence of coagulation factors contained in the blood plasma (the “intrinsic pathway” of coagulation). Both activation pathways lead to the generation of thrombin, an enzyme that converts the soluble blood protein fibrinogen into fibrin, in turn fibrin forms fibrin fiber. Another enzyme generated by thrombin, factor XIII, then cross-links the fibrin fiber, resulting in the formation of an insoluble gel that serves as a scaffold for blood clot formation.
The enzyme plasmin circulating in the blood, the main enzyme of fibrinolysis, breaks down the fibrin gel in several places. The resulting fragments of “high molecular weight polymers” are cleaved by plasmin several times longer and leave behind intermediate and then small polymers (fibrin breakdown products). However, the cross-links between the two D fragments remain unchanged. A typical D-dimer containing fragment consists of two D domains and one E domain from the original fibrinogen molecule.
D-dimers are usually not present in human plasma unless the coagulation system has been activated, such as in the case of advanced thrombosis or disseminated intravascular coagulation. The D-dimer assay depends on the binding of monoclonal antibodies to a specific epitope on the D-dimer fragment. There are several different D-dimer analyzers available for commercial use, using different anti-D-dimer monoclonal antibodies. For some of them, the distance to the D-dimer at which binding to the monoclonal antibody is possible is known. Antibody binding is then quantified using one of various laboratory techniques.
What do we know about D-dimer?
What does it represent?
D dimer is a protein molecule that has some relation to the blood coagulation and anticoagulation system.
So, the process of blood clotting begins. One of the stages of blood clotting is the formation of an intermediate substance - thrombin. Thrombin promotes the conversion of fibrinogen to fibrin. This point is worth dwelling on in more detail.
Fibrinogen is a protein molecule consisting of several peptide chains. Under the influence of thrombin, 4 fibrinopeptides are cleaved: 2 fibrinopeptide A and 2 fibrinopeptide B. As a result, fibrin monomers are formed, which make up the insoluble fibrin polymer molecule. This polymer is a clot that prevents blood flow.

The fibrinogen molecule has D and E regions. By connecting with each other, they form a strong network of monomers, forming a polymer complex.
In response to the formation of a clot, the body starts the reverse process - the breakdown of fibrin. This process is called fibrinolysis.
The process of fibrin breakdown is triggered by plasminogen. It is activated in response to fibrin formation. Plasminogen is the precursor of plasmin. Plasmin “cuts” the network of fibrin polymers into various sections - products of fibrin degradation. These include the D dimer.
That is, the mechanism that can explain where D-dimer comes from in the body looks something like this:
- thrombin triggers the conversion of fibrinogen to fibrin;
- as a result of fibrin formation, the fibrinolysis system is activated;
- During the breakdown of fibrin, various products are formed, which include D-dimer.
What functions does it perform?

D-dimer has no specialized functions in the body. However, this indicator has great diagnostic value; it indicates at what level the processes of clot formation and its splitting occur.
After D-dimers are formed during the breakdown of fibrin, they circulate in the bloodstream for 24 hours and are then excreted from the body. This allows this indicator to be used to assess the body's ability to form blood clots.
Historical facts about D-dimer
D-dimer was first described back in the seventies of the twentieth century. However, the practical use of this indicator to assess the risk of blood clots began only in the nineties.
D-dimer in the first trimester
Experts have not established clear D-dimer levels that are normal today. Each private laboratory takes its own numbers as the norm, and each of them may have different units of measurement - mg/l, μg/ml and others.
The lack of clear standards for D-dimer during pregnancy is due to the fact that this analysis is not included in the mandatory list of examinations of pregnant women. The result may vary significantly at different times. Moreover, even a result different from the norm will not clearly indicate any threat to the life and health of the mother and baby.
However, if the indicator is increased several times, then there is good reason to worry and undergo additional examinations. Often this situation is possible in various pathological conditions that can accompany pregnancy. Among them:
- Infectious processes.
- Dyslipidemia.
- Heart rhythm disturbances.
- Placental abruption.
- Oncological processes.
- Pathologies of the biliary (bile) system.
- Traumatic injuries.
- Surgical interventions.
- Rheumatic and autoimmune processes.
A slight increase in D-dimer levels in the first trimester is not a reason to begin treatment for coagulopathy, since this may be a normal physiological phenomenon. The indicator begins to increase from the very first days of pregnancy, and its norm at this time can range from 500 to 700 ng/ml.
It is possible that it decreases, but for expectant mothers this is an extremely rare occurrence.
It is important to understand that such a result does not pose any threat to the life of the woman and the fetus, because only an increase in D-dimer entails consequences. Additional diagnostic measures, as well as consultation with a hematologist, are necessary if the indicator significantly decreases below normal
This result may indicate pronounced pathological processes of hemostatic function, which, in turn, during childbirth can lead to heavy bleeding.

d-dimer standards
The norm for a healthy person is the complete absence or minimal value of d-dimer. This protein appears only when fibrin clots, which a healthy person does not have, dissolve. Acceptable normal values are 0.55 μg FEU/ml or 250 ng/ml.
When conducting the analysis, the following points are taken into account:
- The study indicates the presence of blood clots, but does not even hint at their location.
- If there are characteristic clinical symptoms and the indicator is normal, the doctor prescribes an additional study. This eliminates errors that are possible during blood collection or storage.
- If two negative results are obtained, the diagnosis of thrombosis is removed.
- The result of the analysis depends on the age of the patient. The higher it is, the higher the D-dimer index. After 50 years, the formula is used: the number of years multiplied by 10 in ng/ml.
Reasons for the increase
A high content of protein fragments indicates a constant process of blood clot disintegration. The circulatory system tries on its own to fight the resulting clots that close the lumens of the blood vessels.
An increase in D-dimer may occur with:
- deep vein thrombosis;
- disseminated intravascular coagulation;
- pulmonary embolism;
- neoplasms;
- pathologies of the cardiovascular system;
- thrombolytic treatment;
- inflammatory processes;
- liver diseases;
- operations;
- injuries.
The content of a specific protein may increase during pregnancy, as well as in older people.
Reasons for the downgrade

D-dimer is an indicator whose concentration is never lower than normal, since its limit value is zero. And the result cannot be lower than this value. Therefore, a low value implies a falsely low result due to laboratory error.
On a note! A decrease in the higher previously measured result may be observed after taking heparin and using indirect anticoagulants.
Indications
D-dimer testing is indicated when deep vein thrombosis (DVT), pulmonary embolism (PE), or disseminated intravascular coagulation is suspected. The possibility of diagnosing aortic dissection is being studied. For DVT and PE, there are different calculation systems that are used to determine the “prior” clinical probability of these diseases; the most famous were introduced by Wells et al (2003).
- If there is or is likely to be a serious clinical indication, D-dimer levels will have little effect and anticoagulant therapy should be initiated regardless of the test results. In the case of deep vein thrombosis or PE, additional tests may be performed.
- for low to moderate clinical indications or likelihood: a negative D-dimer blood level virtually eliminates thromboembolism: the extent to which the D-dimer test reduces the likelihood of thrombotic disorders depends on the characteristics of the particular test used in the clinical setting: the most common D test -dimers with a negative result indicates a probability of thromboembolism of less than 1%, while the probability of a preliminary assessment is less than 15-20%.
- If D-dimers show a high result, then ultrasound examinations of the veins of the legs (ultrasonography) or lungs (scintigraphy) are performed to confirm the presence of a blood clot. Depending on the clinical situation, anticoagulant therapy can be started immediately or after additional studies.
In some clinics, laboratory tests are performed after the form showing the estimated value is completed, and only if the estimated value is low or average. This reduces unnecessary testing for patients with a high likelihood of DVT and PE. Performing the D-dimer test first avoids many imaging studies and is also less invasive. Therefore, a D-dimer test is recommended as an initial diagnosis.
What it is?
A lot during pregnancy depends on the proper functioning of the circulatory system. The volume of blood in the body of the expectant mother increases, because two living organisms – mother and baby – need to be provided with all the necessary substances, nutrition, and vitamins. Through the umbilical cord through the placenta, the child receives the mother’s blood, enriched with oxygen and nutrients, and gives back to her blood, saturated with carbon dioxide and the products of its metabolism.

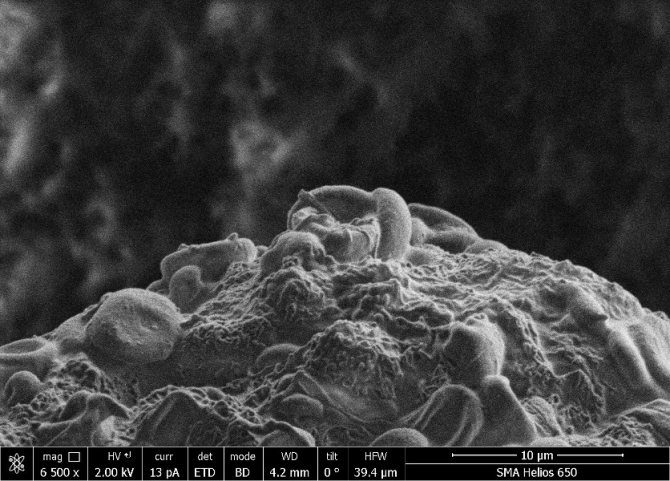
Special blood cells are responsible for the thickness of blood and its ability to clot. Their task is to prevent bleeding and blood loss, to quickly “close” the wound site. This ability of platelets is extremely important during childbirth. If blood did not have such an amazing ability, then the birth of a placenta after a baby would always be accompanied by severe massive bleeding, dangerous to the woman’s life.
Too much can clog blood vessels, so nature provides not only the process of thrombosis, but also fibrinolysis - the dissolution of blood clots. A D-dimer test can tell you how these processes occur in the blood of a pregnant woman.

A D-dimer is a small protein fragment that is formed during fibrinolysis. are formed thanks to fibrin, which is acted upon by a special enzyme, thrombin, in case of danger associated with bleeding (in case of injury, trauma, childbirth). As a result, blood cells begin to quickly bind together into a clot, closing the wound and preventing blood loss. This is a protective mechanism that saves a person's life.
Once the danger has passed, the resulting blood clots are no longer needed. The body needs to get rid of them so that the blood vessels do not become clogged. To do this, another protein comes into play - plasmin, it starts the process of fibrinolysis. Under its influence, clots gradually dissolve and break down, the vessels are cleaned, and their patency is completely restored. And the part of the substance that is formed after the breakdown of febrin is called D-dimer.

Calculate gestational age
Advantage of the test

Determination of D-dimer - a quick and affordable test
Diagnosis of hemostasis using D-dimer has been used since the 1990s, and during this time it has established itself as a highly effective technique for quickly determining thrombus formation processes in the circulatory system.
To identify thrombosis and concomitant diseases, there are various methods: contrast angiography, ultrasound Dopplerography of veins, lung scintigraphy and other techniques. But these studies are not available to every clinic, and do not always accurately determine the presence of blood clots.
Tests based on blood samples that diagnose other markers of the hemocoagulation system take significantly longer to reveal results. For example, diagnosing fibrinopeptide requires excluding all cross-reacting fibrinogen from the plasma sample.
Another advantage of the D-dimer test is that it is independent of the blood sample collection technique. Also, the result is not affected by platelet admixture, which accompanies the diagnosis of other indicators.
A distinctive feature of D-dimers is their resistance to decay; the duration of circulation of molecules in the bloodstream is about 300 - 400 minutes.
Preparing for analysis
To ensure the reliability of the research result, the following preparation rules should be observed:
- 12 hours before taking blood, you should stop eating and drinking alcohol, and you should also try not to smoke;
- on the eve of the study, it is worth excluding excessive physical activity;
- on the day of taking blood for analysis, you are allowed to drink clean still water;
- The possibility of taking medications on the eve of the study should be discussed with your doctor. It is advisable to stop taking medications, especially if they affect blood clotting;
- If you are prescribed other medical or diagnostic procedures, try to get your blood tested before they are performed.
Blood for D-dimer analysis is taken from a vein. In our clinic, blood is drawn using modern vacuum systems into a pre-labeled test tube, which eliminates the unreliability of the test result.
D-dimer: what is it?
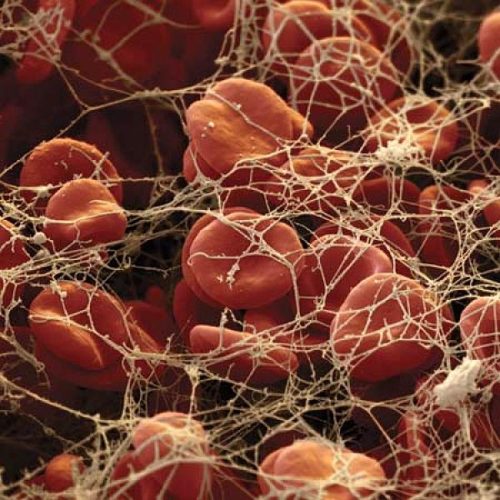
D-dimer is a consequence of the decomposition of the fibrin protein (a small fragment of it). It appears in the blood as a result of fibrinolysis - the destruction of a blood clot. The element received its name because of the two connecting D-parts of the fibrinogen protein. An increase in fibrin protein in the blood causes the formation of blood clots, an excessive amount of them leads to blockage of veins and even arteries with blood clots. To maintain the required level of fibrin, the body produces an enzyme such as plasmin, which helps dissolve this protein. The result of this reaction is D-dimer.
Note!
The test determines the possibility of thrombosis with a 98% probability.
If the indicator does not exceed the established norm, the likelihood of blood clots is practically excluded; if it is positive, it is necessary to conduct a more detailed examination for other diseases.
The D-dimer test helps rule out intravascular coagulation syndrome. Education is influenced by the following factors:
- large size of the destroyed blood clot;
- the use of thrombolytic drugs increases concentration;
- the use of anticoagulant agents reduces the rate.
In a young man without obvious pathologies, the marker is stable and does not cross the value of 0.25 ng/ml. An increase in D-dimer indicates the onset of coagulation or fibrinolysis pathology, which occurs when:
- blood clotting syndrome inside blood vessels;
- pulmonary embolism;
- vein blockage;
- abnormalities of the cardiovascular system;
- extensive surgical interventions;
- thermal burns.
An increase is noted in pregnant women, elderly people, patients with cancer, rheumatoid arthritis and bedridden patients.
D-dimer correction

Treatment for D-dimer depends on the cause of its increase
Correction of the indicator directly depends on the treatment of the conditions that caused the increase in its level. During therapy, changes in the D-dimer value are examined to assess the state of hemostasis.
Treatment of DVT includes heparin and indirect anticoagulants. If therapy is ineffective, a thrombolysis procedure may be prescribed; another direction in treatment is the introduction of a vena cava filter into the vena cava to catch blood clots. In some cases, there is a need for surgical removal of blood clots.
The diagnosis of pulmonary embolism requires mandatory placement of the patient in a hospital, where, if necessary, artificial ventilation of the lungs, cardiopulmonary resuscitation, and administration of substances stimulating cardiac activity are performed. The patient is given anticoagulant and, in some cases, thrombolytic therapy based on medications. Surgery is possible if treatment is ineffective.
In acute DIC, medical procedures are aimed at saving the patient’s life. Anti-shock measures, plasma transfusions, and artificial ventilation of the lungs are being carried out. To restore the hemostatic system, heparin, the introduction of blood clotting factors into the blood, plasmapheresis procedures, and therapy with drugs to improve microcirculation in organs are used.
Cardiovascular diseases associated with the formation of blood clots include a whole group of pathologies, each of which requires careful analysis. Treatment may include the use of antithrombotic drugs and anticoagulants, but in most cases, urgent surgical intervention is required.
Flaws
The dimmer is designed to regulate the power of the light sources for which it is designed. The dimmer output voltage does not have a sinusoidal shape. This can cause step-down transformers (devices designed to convert the supplied voltage to the required voltage) to not work properly. Dimmers can cause electromagnetic interference (including at radio frequencies). The output voltage adjustment depends nonlinearly on the load resistance value. Fluorescent lamps and light sources equipped with additional devices, such as electronic ballasts, transformers, drivers, etc., are incompatible with dimmers, except for those specifically intended for use with a dimmer (the packaging of the light source states that it can be used with a dimmer - there is an inscription “dimmable” or dimmable). Despite the undeniable convenience of using a dimmer to regulate brightness, its efficiency (efficiency) is low when working with incandescent lamps at low brightness. The dependence of the luminous flux on the input voltage is determined by the exponential function. So, at a voltage equal to 50% of the rated voltage and a power consumption equal to 25% of the rated value, the luminous flux is 8.25%. Instead of using a dimmer to reduce power (for example, for night or emergency lighting), lower wattage incandescent lamps should be used
Or you should replace dimmers and incandescent lamps with dimmer circuits and LED light sources. When working with moving mechanisms/tools and when using low-inertia light sources (LEDs, gas-discharge lamps, etc.), dimmers should be used with caution. This can create a dangerous illusion of immobility of the moving parts of the mechanism/tool, which can lead to injury.
Additional Research
If a change in the level of D-dimer in the blood of a pregnant woman is detected, an extensive examination of hemostasis indicators is prescribed. Common studies include a coagulogram, which includes determining the following indicators:
- Blood clotting time is the rate of thrombus formation, the main indicator for assessing blood clotting.
- Prothrombin index or PTI is the ratio of the patient’s blood clotting time to the generally accepted standard.
- Thrombin time is the rate of conversion of soluble fibrinogen to insoluble fibrin. An increase above the norm indicates liver pathology with a violation of the functional state of the organ.
- Activated partial thromboplastin time, or aPTT, is the rate of thrombus formation after the addition of calcium. The indicator allows you to monitor and adjust the treatment of changes in hemostasis.
- Antithrombin III - the concentration of a glycoprotein in the blood is determined, which is an anticoagulant and prevents the formation of blood clots. The indicator makes it possible to assess the risk of developing massive bleeding during childbirth.
- Activated recalcification time or AVR is an indicator of changes in blood clotting against the background of thrombophilia, thrombocytopenia. A marked decrease in AVR requires urgent treatment, as it indicates a life-threatening condition for the patient, in particular large or prolonged bleeding.
- Soluble fibrin-monomer complexes or SFMC - the concentration changes when there is a threat of developing disseminated intravascular coagulation syndrome. The indicator helps in diagnosing complicated pregnancy and renal failure.
- Fibrinogen is the concentration of a dissolved clot precursor compound in the blood.
Normal values for all coagulogram parameters in pregnant women are usually higher. This is due to physiological characteristics and must be taken into account by the doctor when interpreting the study results.

D-dimer in pregnant women is elevated in several diseases
To identify the causes of changes in blood coagulation parameters, a diagnostic objective examination is prescribed. It includes clinical blood and urine tests, biochemical blood tests, ultrasound, electrocardiogram, electroencephalogram and other techniques. X-ray examination, including computed tomography, is not prescribed for a pregnant woman. This is due to the negative impact of ionizing radiation on the developing fetus.
Research methods

The doctor issuing the referral tells the patient where to donate blood. This is done in a clinic at the place of residence or in private laboratories that do coagulation blood tests.
There are several methods for determining D-dimer:
- Immunoenzymatic. It is highly accurate. The disadvantage is the difficulty of use in severe conditions.
- Latex agglutination. A simple but not very accurate method. Can be used in emergency situations. The results are usually distorted by rheumatoid factor.
- Other methods. There are immunochromatography and immunochemiluminescence. These are precise techniques that allow you to detect the smallest concentrations of protein in the blood. Disadvantage: expensive equipment.
Abstract values
Every person's body contains varying amounts of D-dimer. In the male half of the population and non-pregnant females, its concentration should not exceed 500ng/ml. The D-dimer level is important for determining the risk of developing heart attacks and strokes.
Determination of D-dimer in pregnant women should be carried out in each trimester, and the norm will be different at each stage.
In general, there is a trend towards a physiological increase in D-dimer concentrations during pregnancy:
- in the first three months, the level of D-dimer should be one and a half times higher than normal, that is, 750ng/ml;
- over the next three months the indicators double – 1000 ng/ml;
- the last three months are characterized by a threefold increase in the level - 1500 ng/ml.

Analysis transcript
Conditions when D-dimer increases
The detection of D-dimer above reference values indicates conditions accompanied by increased fibrin formation and high plasmin activity.
A slight increase in the concentration of D-dimer in the blood can be observed with:
- minor injuries;
- cardiovascular diseases (myocardial infarction);
- infectious diseases;
- malignant neoplasms;
- pregnancy;
- surgical intervention.
There are also a number of pathologies in which the level of D-dimer in the blood will be significantly higher than the reference values:
- early stage of DIC syndrome;
- pulmonary embolism (D-dimer is a highly sensitive indicator);
- blood clots in the veins;
- blood clots in the arteries.

D-dimer only indicates whether or not there is a blood clot in the vessels. But in order to determine its localization, other research methods are needed.
Sometimes there are false negative results: the thrombus formation process is increased, but the D-dimer is within acceptable values. This occurs when the size of the blood clot is very small or there are disturbances in the plasmin system.
Conditions in which D-dimer levels are low
When the D-dimer level is within acceptable values, this means that the patient does not currently have blood clots in the body. Looking at the numbers of reference values, you can see that there is not always a lower limit. When D-dimer is not detected, or its concentration is so low that it is difficult to detect, this indicates that the body does not currently have a tendency to form blood clots.
That is, the detection of low concentrations of D-dimer does not have important diagnostic value.
Normal D-dimer level in pregnant women
Since thrombosis is associated with a genetic predisposition, you should visit a geneticist at the pregnancy planning stage. Every woman, at her first visit to the antenatal clinic and registration, must do a d-dimer test.
If the pregnant woman is not at risk and the first examination determined normal marker values, repeat analysis is not necessary.
At the beginning of pregnancy, d-dimer levels in the blood of expectant mothers increase insignificantly. In some women, due to individual characteristics, the level may not change at all. In the third trimester, towards the end of pregnancy, the concentration of the marker increases greatly, which is a normal condition.
Table of the norm of d-dimer in a blood test during pregnancy by week:
| Gestational age | D-dimer norm |
| 1-12 weeks | From 0 to 0.55 µg/l |
| 12-21 weeks | From 0.2 to 1.5 µg/l |
| 21-30 weeks | From 0.3 to 1.7 µg/l |
| 30-35 weeks | From 0.3 to 3 mg/l |
| 35-40 weeks | From 0.4 to 3.1 µg/l |
If during pregnancy the d-dimer levels are very high, then after giving birth the woman is recommended to do a control test. Usually after 1.5-2 months the marker values return to normal. Before this period, it is not advisable to examine the blood; the female body has not yet returned to normal, the result will be false. When marker values were normal during pregnancy, repeat testing is not required.
Increased D-dimer during pregnancy
Most often, during pregnancy, the d-dimer marker does not exceed the normal limit or increases slightly for natural reasons. Pathologically elevated d-dimer during pregnancy can be observed in the following cases:
- Diabetes types 1 and 2;
- Kidney and liver diseases;
- Late complications of pregnancy - edema, high blood pressure, active excretion of protein in the urine, convulsions;
- Functional disorders of the heart;
- Allergic conditions;
- The presence of two or more embryos;
- Infectious diseases, injuries;
- Surgical operations;
- Premature placental abruption.
Abnormal results reveal the exact cause of the increase in d-dimer. To bring the marker back to normal, therapeutic treatment is prescribed. With a slight increase, therapeutic measures can be carried out at home. If there is a significant deviation from normal boundaries, a pregnant woman needs observation in a hospital. Timely adjustment of the marker directly reduces the likelihood of serious illnesses and helps a woman bear a healthy child.

Low D-dimer during pregnancy
If a blood marker test determines a low normal value, very often this goes unnoticed, since pregnancy complications do not arise and no serious violations occur. There are no specific reduction standards, there are only approximate limits. However, additional consultation with specialists is still necessary.
During pre-examination, blood clotting disorders are detected for the following reasons:
- Hereditary hemophilia;
- Insufficient intake of vitamin K1 and K2 into the body;
- Liver oncology;
- Overdose of blood thinners;
- Low hemoglobin.
In order to return the indicators to normal, a woman is recommended to enrich her diet with foods containing vitamin K - these are all green leafy vegetables, raw turnips, broccoli, cucumbers, cabbage and cauliflower. Vitamin K can be given by injection. If there is a significant decrease in indicators and there is a threat of fetal loss, donor platelets are transfused.
D-DIMER AS A MARKER OF THROMBUS FORMATION AND ITS APPLICATION IN CLINICAL PRACTICE.
A laboratory test for determining D-dimer based on the frequency of measurements is one of the most popular studies in the practical study of the blood coagulation system. It ranks fourth in terms of the number of prescriptions after prothrombin time (PT), activated partial thromboplastin time (APTT) and fibrinogen. Since the discovery of D-dimer (1970s) and the beginning of its use in clinical practice (1990s), the blood test for D-dimer has firmly entered the arsenal of frequently used tests by doctors of many specialties to diagnose diseases associated with pathological thrombus formation. D-dimer is the end product of a process that occurs in the human body as fibrinolysis. In 1893, the term “fibrinolysis” was proposed to be used by the French physiologist Dastre, and in 1905, a scientist from Germany Morawitz suggested that some enzymes take part in fibrinolysis. This was confirmed by Dr. Sherry (USA) in 1959, who proved that the activator of fibrinolysis is plasmin, formed from its precursor plasminogen. In 1973, two research groups simultaneously reported the discovery of a unique fragment obtained from the hydrolytic cleavage of fibrin protein by the enzyme plasmin in human serum (1). Later, this fragment was called D-dimer and it began to be used as a tool for diagnosing various diseases. Many clinical conditions are characterized by an increase in the concentration of D-dimer in the blood plasma (Table 1).
| Pathological | Not pathological |
| Condition after injury (7) | Smoking (2) |
| Preeclampsia/eclampsia (8.9) | Age (healthy older adults) (3) |
| Oncopathology (10) | Normal pregnancy (4) |
| Disseminated intravascular coagulation (11) | Postoperative condition (5.6) |
| Sickle cell anemia (12) | Invasive manipulations |
| Arterial and venous thromboembolism (13,14) | Inactivity or prolonged immobilization |
| Atrial fibrillation (15) | Long-term use of estrogen drugs |
| Acute coronary syndrome (16) | |
| Stroke (17-19) | |
| Acute gastrointestinal bleeding (20) | |
| Nephrotic syndrome | |
| Infections, sepsis, inflammation | |
| Pulmonary embolism (21) | |
| Kidney diseases (23) | |
| Acute renal failure | |
| Liver diseases (22) | |
| Myocardial infarction | |
| Stress (24) |
Mechanism of D-dimer formation.
Currently, fibrinogen breakdown products are used to diagnose thrombosis (Fig. 1). Fibrinogen, under the action of thrombin, forms fibrin monomers by cleaving two small fragments (fibrinopeptides A and B). During this process, the negative charge E of fibrinogen (red circles) is converted to a positive charge, allowing fibrin monomers to spontaneously polymerize into a polymer that is stabilized by hydrogen bonds. Thrombin also activates factor XIII (a transglutaminase enzyme), which stabilizes the fibrin parent polymer by catalytically forming cross-linked covalent bonds between adjacent D domains (green circles). Tissue plasminogen activator (t-PA), a serine protease, converts inactive plasminogen into active plasmin, which breaks down fibrin into many small fragments called fibrin degradation products (FDPs). D-dimer, formed from two adjacent cross-linked monomers, is one of the main PDFs. In contrast to the final products of fibrinogen cleavage, which are presented in the form of separate fragments D and E, when cleavage of fibrin fibers cross-linked by factor XIIIa, larger fragments are formed - D-dimers, DED trimers, since plasmin is not able to cleave the covalent bond between D-domains.
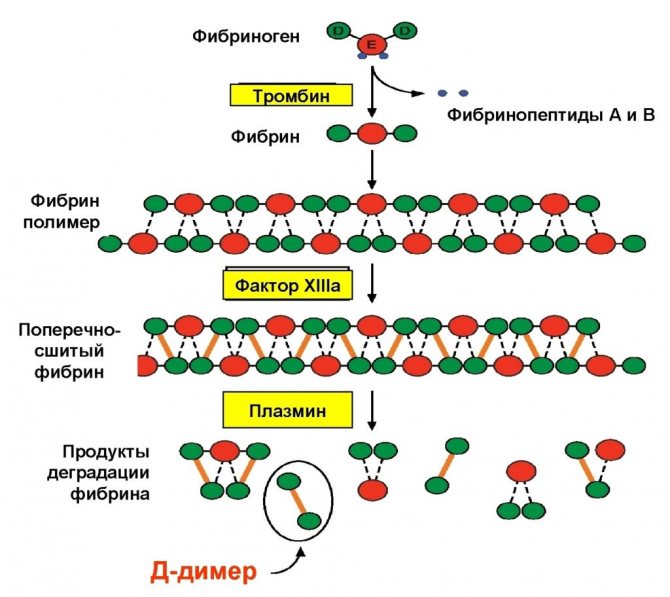
Fig.1. Mechanism of D-dimer formation.
Thus, the action of the fibrinolytic system is aimed at the lysis of fibrin, and, with excessive activation, fibrinogen. The result is a mixture of fibrin/fibrinogen degradation products. The products of fibrin degradation are large fragments of D-dimers and trimers, and the products of fibrinogen degradation are individual oligopeptides with a small molecular weight. Only degradation products of cross-linked fibrin contain D-Dimers. The following rule applies:
| Clot + Fibrinolysis = D-dimer formed No clot + Fibrinolysis ≠ D-dimer not formed |
D-dimer refers to both markers of activation of coagulation and fibrin formation, and markers of activation of fibrinolysis. The half-life of D-dimer is approximately 8 hours, clearance is through the kidneys and the reticuloendothelial system. Determination of D-dimer is the most common laboratory marker of activation of coagulation and fibrinolysis.
Methods for determining D-dimer.
1. Qualitative and semi-quantitative methods:
– Agglutination reaction of latex particles (plasma);
2. Quantitative:
– Immunochromatography; Point-of-Care (diagnosis at the point of treatment).
– ELISA (enzyme-linked immunosorbent assay; enzyme-linked immunosorbent method);
– Immunodiffusion on porous membranes;
– Immunoturbidimetry.
Brief description of the methods.
1. Methods for determining D-dimer based on latex agglutination.
Latex beads coated with monoclonal antibodies against D-dimer are added to the plasma containing D-dimer and the time of appearance of macroscopic agglutination on the slide is noted. These are inexpensive and easy to carry out studies. They have moderate sensitivity but higher specificity for deep vein thrombosis (DVT) and pulmonary embolism (PE).
2. Immunochromatography method.
The relative insensitivity of latex agglutination tests led to the development of more sensitive tests based on immunochromatographic rapid diagnostics. This method combines the speed of research (from 2 minutes) with high sensitivity. The particular value of the immunochromatographic method for DVT was noted.
3. ELISA method.
ELISA methods for testing D-dimer have high sensitivity but relatively low specificity. The low specificity of these methods causes false positive results in a significant number of cases. The method consists of adding microplates coated with antibodies to the D-dimer of the plasma under study to the wells. After incubation, enzyme-labeled antibodies are added and, after stopping the reaction, a colorimetric measurement is performed. This method is labor-intensive and time-consuming to carry out, and also requires special equipment. These circumstances make it impractical for routine use in clinical practice.
4. Immunodiffusion on porous membranes .
In recent years, immunoenzyme methods for determining D-dimer have been developed, which allow obtaining results within 10 minutes. They use porous membranes coated with antibodies that capture D-dimer. The patient's plasma is filtered through a membrane and then labeled antibodies are added to the filtrate to detect bound D-dimer
5. Immunoturbidimetry.
One of the options for the latex method for determining D-dimer is the micro-latex agglutination method or the immunoturbidimetric method. When patient plasma containing D-dimer is added to the reagent, the optical density of the solution increases, which is directly proportional to the concentration of D-dimer in the test sample. Commercial kits for the determination of D-dimer have been developed for automatic analyzers (biochemical and coagulometers), which allows studies of this analyte to be carried out routinely.
Two types of D-Dimer units.
1. D-Dimer Units (DDU) - for methods using purified D-Dimer as a calibrator.
2. Fibrinogen Equivalent Unit (FEU ) – fibrinogen equivalent units (FEU), for methods that use PDF, formed under the influence of plasmin, as a calibrator.
The unit size is indicated by the test manufacturer (ng/ml, μg/ml, μg/l).
Reference values of D-dimer.
Threshold values for D-Dimer depending on measurement units:
1. DDU ≤ 0.25 µg/ml (250 ng/ml or 250 µg/l);
2. FEU ≤ 0.5 μg/ml (500 ng/ml or 500 μg/L).
The numerical values are easily converted into each other, since the mass of one FEU unit is equal to half the DDU. For example, 0.5 µg/ml FEU = 0.25 µg/ml DDU.
If the concentration of D-Dimer in plasma is less than the specified threshold values, then the presence of thrombosis in the patient can be excluded.
Limitations in determining D-dimer.
The D-dimer test is not a standardized marker. To date, there are about 30 commercial test systems for determining D-dimer, between which certain differences are observed, since each manufacturer establishes its own standardization method.
The main reasons for the limitations of the method are:
– the use of various monoclonal antibodies (more than 20), differing in specificity and sensitivity;
– lack of International Reference Preparation;
– lack of a standard calibrator;
– different units of measurement used for different methods.
The lack of standardization of different D-dimer test systems means that results, reference intervals and cut-off values cannot be extrapolated across different methods. When quantitatively measuring the D-dimer of the same patient with different test systems, different results are obtained, which are not correct to compare.
Reasons for differences in D-Dimer tests.
1. D-dimer antigen is not homogeneous, but consists of compounds containing fragments D and E with different molecular weights (Fig. 2.)
2. When analyzing D-dimer, various antibodies, buffers, measuring equipment, and standards are used.
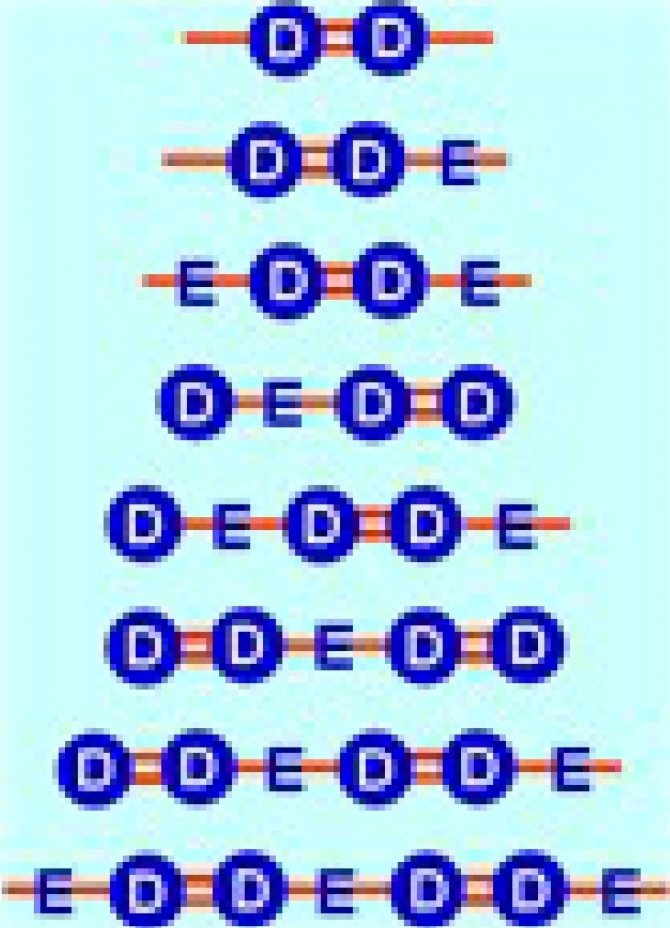
Fig.2. D-dimer antigen, consisting of many fragments D and E.
This variability in the types and units of measurement of D-dimer has led to confusion in some laboratories, especially when it was necessary to establish a threshold to exclude venous thromboembolism.
It must be remembered that there are 2 different types of units for D-dimer (Fig. 3):
1. D-dimer unit – DDU with m.m. 195 kDa;
2. Fibrinogen equivalence unit – FEU with m.m. 340 kDa
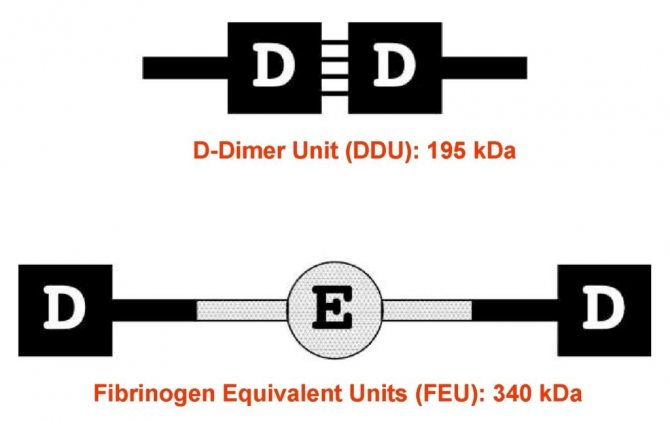
Fig.3. Two types of units for D-dimer (DDU and FEU).
Because D-dimer is expressed in mass units, the type of units involved is very important in establishing the threshold to rule out venous thromboembolism and in interpreting the results.
Thus, methods for determining D-dimer are based on its interaction with monoclonal antibodies to specific epitopes in the D-domains of fibrin molecules. These specific antibodies bind to D-dimers containing DD covalent bonds, but do not react with fibrinogen and soluble fibrin monomers. D-dimers found in plasma are an indicator of the breakdown of fibrin, but not fibrinogen and fibrin monomers.
Clinical significance of D -dimer .
Clinical applications D-dimer measurement is indicated for:
– exclusion of venous thromboembolism (VTE);
– diagnosis and monitoring of disseminated intravascular coagulation (DIC);
– determination of the duration of anticoagulant therapy.
The issue of using D-dimer remains debatable when:
– prognosis of the course of diseases of the cardiovascular system;
– predicting adverse pregnancy outcomes;
– additional assessment of the risk of thromboembolism in other pathologies.
1. Venous thromboembolism..
Venous thromboembolism is a fairly common pathology that combines deep vein thrombosis and pulmonary embolism. The formation of any thrombus in the vascular bed always leads to the activation of fibrinolysis and the appearance of fibrin breakdown products in the blood. The sensitivity of the D-dimer test in the diagnosis of venous thromboembolism is very high - 90-100%. This test may be performed to confirm the presence of thrombosis. When assessing the results of the study, it should be taken into account that an increase in the level of D-dimer in the blood only indicates the formation of fibrin and its lysis, however, in which part of the vascular bed, in what volume and for what reason this happened must be decided in each specific case with the help of clinical and visualization methods (Doppler ultrasound). The level of D-dimer in PE is practically independent of the localization of the pulmonary thrombus. The D-dimer test has a high negative prognostic level - 97-100%. It is valuable not so much for confirming the fact of thrombosis, but for excluding it. A negative test result almost always indicates the absence of blood clots in the bloodstream. Therefore, the main goal of the D-dimer study is to exclude the presence of blood clots in the vascular bed in the differential diagnosis of DVT and PE.
There are certain limitations to the use of D-dimer in VTE (25-27) (Table 2).
| D-dimer cannot be used to diagnose VTE | D-dimer should be used with caution |
| patients with VTE symptoms > 14 days | patients with recurrent VTE |
| patients taking heparin or oral anticoagulants. | patients aged > 50 years |
| hospitalized patients | |
| pregnant women | |
| up to 30 days after surgery | |
| patients with blood diseases, diabetes mellitus |
Table 2. Limitations when using the D-dimer test for VTE.
It should be noted that D-dimer may be negative in PE if the clot is old (2 weeks or more after clot formation) and if the clot is very small. D-dimer may be falsely elevated in the presence of a high IgM titer. If the threshold value is exceeded, confirmation of the diagnosis is necessary using Doppler ultrasound, spiral computed tomography or contrast venography. Another strategic approach for diagnosing VTE is a preliminary assessment using clinical anamnestic scoring scales (Wells scale) (28-31).
2. Disseminated intravascular coagulation.
Disseminated intravascular coagulation (DIC) is a common pathology with high morbidity and mortality. It is characterized by systemic activation of the hemostatic system with intravascular fibrin formation and increased fibrinolysis (32,33). If patients are not treated appropriately, platelets, clotting factors, and inhibitors become depleted, which can result in life-threatening bleeding and/or thrombosis. DIC is most common in patients with infectious inflammatory diseases, malignant neoplasms, trauma, or obstetric pathology. The classification of DIC divides this pathology into asymptomatic (pre-DIC), organ failure, bleeding and subtypes of massive bleeding. ISTH (International Society of Thrombosis and Haemostasis) has harmonized guidelines for the diagnosis and treatment of DIC (34,35). D-dimer is included in the ISTH guidelines as a recommended laboratory test for the evaluation of patients with DIC.
3. Anticoagulant therapy.
Anticoagulants of indirect action.
After completion of treatment with indirect anticoagulants (ANDA) in patients (including the elderly), quantitative determination of D-dimer levels provides valuable information for individual assessment of the risk of venous thromboembolism. Using statistical methods, age-dependent cut-off levels for D-dimer in relation to the risk of VTE were determined, the components when using various test systems are 250-700 µg/l FEU for patients under 70 years of age and 450-1000 µg/l FEU for patients over 70 years of age (36) (Fig. 4).
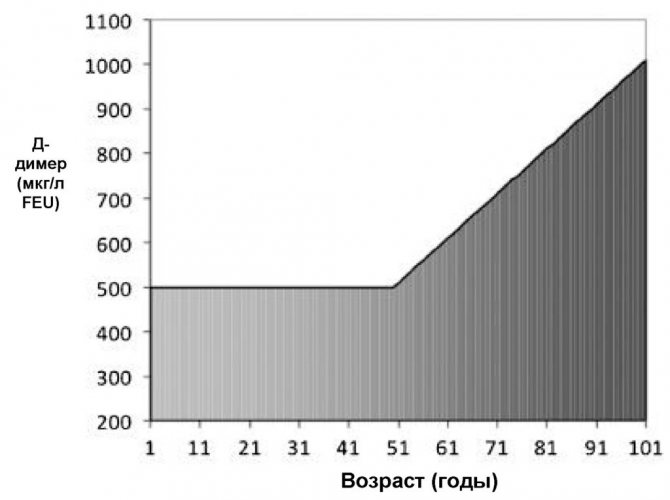
Fig.4. Changes in D-dimer concentration depending on age.
At 30 days after warfarin discontinuation, normal D-dimer levels had a very high negative predictive value for recurrent VTE, especially in patients with congenital thrombophilia or new-onset spontaneous thrombosis, and elevated D-dimer levels corresponded to a higher risk of VTE. At the same time, a negative D-dimer test result 2 weeks after the end of a 3-month course of warfarin treatment was associated with a 3.5% risk of recurrent VTE within a year, and a positive result with a risk of 8.9%. These data indicate the important role of D-dimer in determining the optimal duration of AED treatment for reliable prevention of recurrent venous thrombosis.
Heparin therapy.
The effectiveness of heparin therapy is determined by changes in the level of D-dimer dynamics. A decrease in D-dimer indicates a correctly selected dose of heparin in patients with activation of hemostasis of any etiology. The test is also informative for treatment with low molecular weight heparins. Administration of clexane for 2-3 weeks leads to a decrease in the level of D-dimer by 1.5-2 times, and 10-day use of enoxyparine contributed to a decrease in the level of this analyte by 23%.
4. Cardiovascular system.
Circulating D-dimer levels are increased in patients with coronary artery disease, acute ischemic events, including myocardial infarction and unstable angina. In patients with chest pain, elevated D-dimer levels are an early marker of coronary artery ischemia and an independent prognostic factor for myocardial infarction (37). In a study of 18 biomarkers of coronary heart disease risk in a cohort of more than 27,000 postmenopausal women, only D-dimer levels were significantly increased and were a risk factor independent of other markers (38). The work of Marcucci R. et al. (39) showed that the content of D-dimers is significantly higher in patients with functional class IV of chronic heart failure (CHF) compared to patients with functional classes II and III. This study, which included 214 patients with functional classes II–IV, convincingly proved that an increase in D-dimers is a significant predictor of mortality in CHF.
5. D-dimer level during pregnancy.
In pregnant women, due to the activation of the synthesis of plasma hemostatic factors in the liver, even normally, a moderate thrombophilic situation is observed. By the time of birth, D-dimer levels may be 3-4 times higher than baseline (40) (Table 3).
| Units | Not pregnant | 1st trimester | 2nd trimester | 3rd trimester |
| ng/ml | < 500 | 50 – 950 | 320 – 1290 | 130 – 1700 |
Table 3. Plasma D-dimer levels in normal pregnancy.
Shifts in hemostasis parameters reach a maximum in the 3rd trimester of pregnancy, which has physiological significance and is aimed at reducing blood loss during childbirth. Positive D-dimer results in late pregnancy significantly complicate risk assessment and diagnosis of DVT and especially PE. A significant (5-10 times) increase in the level of D-dimer is observed in pregnancy pathologies (recurrent miscarriage, gestosis, premature placental abruption). This leads to the appointment of additional diagnostic procedures. In such cases, the combined use of ultrasound and D-dimer analysis is of particular importance. The cut-off level of D-dimer in relation to the risk of venous thromboembolism in pregnant women in the 3rd trimester appears to be significantly higher.
6. Assessment of the risk of thromboembolism in other diseases.
Elevated levels of D-dimer are observed in diseases such as benign and malignant tumors, infections, trauma, ischemia, bleeding or thrombosis. For many of these pathologies, researchers have attempted to use D-dimer levels as a diagnostic and prognostic test. For example, D-dimer levels have been studied as poor prognosis and/or risk factors in patients with malignancies, gastrointestinal bleeding and necrosis, intracerebral hemorrhage, sickle cell disease, migraine with severe headaches, traumatic brain injury, tuberculosis, Cushing's disease, asthma and many other diseases. Of all these diseases, cancer has attracted the greatest interest. Overall, the risk of venous thrombosis in cancer patients is 7% due to the prothrombotic effect of malignancy and associated risk factors such as immobilization, medications, and surgery (41,42). However, elevated D-dimer levels in cancer patients limit the diagnostic value of the result when used alone. Numerous studies have shown the unfavorable prognostic significance of elevated plasma D-dimer levels in patients with breast, colon, lung, ovarian, prostate, and other cancers (43–52).
Conclusion.
D-dimer is a reliable and sensitive test for the process of thrombus formation, and an increase in its content in the blood plasma indicates the presence of blood clots. In clinical practice, D-dimer is used as a marker of the body's ability to hypercoagulate and endogenous fibrinolysis. A positive D-dimer test has a negative prognostic value for patients with DVT and PE. This test is used to monitor anticoagulant therapy and is a sensitive marker in the diagnosis of DIC syndrome. It is advisable to prescribe a D-dimer test during pregnancy to exclude the diagnosis of DVT. D-dimer plays a significant role as one of the potential risk factors for the development of coronary heart disease. Therefore, D-dimer can be considered one of the most valuable laboratory tests for diagnosing and monitoring conditions associated with thrombosis.
LITERATURE
1. Gaffney PJ D-dimer. History of the Discovery, Characterization and Utility of this and other Fibrin Fragments. Fibrinolysis // l993.-7.-Suppl 2: P. 2-8.
2. Lowe GD, Yarnell JW, Rumley A, et al. C-reactive protein, fibrin D-dimer, and incident ischemic heart disease in the Speedwell Study: are inflammation and fibrin turnover linked in pathogenesis? Arterioscler Thromb Vasc Biol 2001;21:603–10.
3. Pieper CF, Rao KM, Currie MS, et al. Age, functional status, and racial differences in plasma D-dimer levels in community-dwelling elderly persons. J Gerontol Med Sci 2000;55:M649–57.
4. Eichinger S. D-dimer testing in pregnancy. Semin Vasc Med. 2005;5(4): 375–378.
5. Larsen JF, Ejstrud P, Svendsen F, et al. Randomized study of coagulation and fibrinolysis during and after gasless and conventional laparoscopic cholecystectomy. Br J Surg 2001;88:1001–5.
6. Nguyen NT, Owings JT, Gosselin R, et al. Systemic coagulation and fibrinolysis after laparoscopic and open gastric bypass. Arch Surg
2001;136:909–16.
7. Engelman DT, Gabram SGA, Allen L, et al. Hypercoagulability following multiple trauma. World J Surg 1996;20:5–10.
8. Kobayashi T, Tokunaga N, Sugimura M, et al. Coagulation/fibrinolysis disorder in patients with severe preeclampsia. Semin Thromb Hemost 1999;25:451–4.
9. Kobayashi T, Tokunaga N, Sugimura M, et al. Predictive values of coagulation/fibrinolysis parameters for the termination of pregnancy complicated by severe preeclampsia. Semin Thromb Hemost 2001;27:137–41.
10. Raimondi P, Bongard O, de Moerloose P, et al. D-dimer plasma concentration in various clinical conditions: Implication for the use of this test in the diagnostic approach of venous thromboembolism. Thromb Res 1993;69:125–30.
11. Lane DA, Preston FE, Van Ross ME, et al. Characterization of serum fibrinogen and fibrin fragments produced during disseminated intravascular coagulation. Br J Haematol 1978;40:609–15.
12. Tomer A, Harker LA, Kasey S, et al. Thrombogenesis in sickle cell disease. J Lab Clin Med 2001;137:398–407.
13. Di Nisio M, Squizzato A, Rutjes AW, Buller HR, Swinderman AH, Bossuyt PM. Diagnostic accuracy of D-dimer test for exclusion of venous thromboembolism: a systematic review. J Thromb Haemost. 2007;5(2):296–304.
14. Acosta S, Nilsson TK, Björck M. Preliminary study of D-dimer as a possible marker of acute bowel ischaemia. Br J Surg 2001;88:385–8.
15. Nakagawa K, Hirai T, Shinokawa N, et al. Relation of fibrillatory wave amplitude with hemostatic abnormality and left atrial appendage dysfunction in patients with chronic nonrheumatic atrial fibrillation. Jpn Circ J 2001;101:13–21.
16. Bayes-Genis A, Mateo J, Santalo M, et al. D-Dimer is an early diagnostic marker of coronary ischemia in patients with chest pain. Am Heart J 2000;140:379–84.
17. Berge E, Friis P, Sandset PM. Hemostatic activation in acute ischemic stroke. Thromb Res 2001;101:13–21.
18. Nina P, Schisano G, Chiapetta F, et al. A study of blood coagulation and fibrinolytic system in spontaneous hemorrhage. Correlation with Hunt-Hess grade and outcome. Surg Neurol 2001;55:197–203.
19. Koch HJ, Horn M, Bogdahn U, Ickenstein GW. The relationship between plasma D-dimer concentrations and acute ischemic stroke subtypes. J Stroke Cerebrovasc Dis. 2005;14(2):75–79.
20. Vreeburg EM, Levi M, Rauws EA, et al. Enhanced mucosal fibrinolytic activity in gastroduodenal ulcer hemorrhage and the beneficial effect of acid suppression. Aliment Pharmacol Ther 2001;15:639–46.
21. Jimenez Castro D, Perez-Rodriguez E, Montaner L, et al. Diagnostic value of D-dimer in pulmonary embolism and pneumonia. Respiration 2001;68:371–5.
22. Cioni G, Cristani A, Mussini C, et al. Incidence and clinical significance of elevated fibrin(ogen) degradation product and/or D-dimer levels in liver cirrhosis patients. Ital J Gastroenterol. 1990;22(4):70–74.
23. Noha M., Hiba B. D-dimer Levels in Patients Presenting Chronic Kidney Disease in Sudan. American Journal of Medicine and Medical Sciences 2021, 6(3): 120-122.
24. von Kanel R, Bellingrath S, Kudielka B. Association of vital exhaustion and depressive symptoms with changes in fibrin D-dimer to acute psychosocial stress. J Psychosom Res. 2009. 67(1): 93-101.
25. Thachil J, Fitzmaurice DA, Toh CH. Appropriate use of D-dimer in hospital patients. Am J Med. 2010;123(1):17–19.
26. Lippi G, Bonfanti L, Saccenti C, Cervellin G. Causes of elevated D-dimer in patients admitted to a large urban emergency department. Eur J Intern Med. 2014;25(1):45–48.
27. Spring JL, Winkler A, Levy JH. The influence of various patient characteristics on D-dimer concentration in critically ill patients and its role as a prognostic indicator in the intensive care unit setting. Clin Lab Med.
2014;34(3):675–686.
28. Rodger MA, Le Gal G, Wells P, et al. Clinical decision rules and D-Dimer in venous thromboembolism: current controversies and future research priorities. Thromb Res. 2014;134(4):763–768.
29. Streiff MB. Predicting the risk of recurrent venous thromboembolism (VTE). J Thromb Thrombolysis. 2015;39(3):353–366.
30. Sartori M, Cosmi B, Legnani C, et al. The Wells rule and D-dimer for the diagnosis of isolated distal deep vein thrombosis. J Thromb Haemost. 2012;10(11):2264–2269.
31. Novielli N, Sutton AJ, Cooper NJ. Meta-analysis of the accuracy of two diagnostic tests used in combination: application to the ddimer test and the wells score for the diagnosis of deep vein thrombosis. Value Health.2013;16(4):619–628.
32. Levi M. Diagnosis and treatment of disseminated intravascular coagulation. Int J Lab Hematol. 2014;36(3):228–236.
33. Wada H, Matsumoto T, Aota T, Yamashita Y. Progress in diagnosis and treatment for disseminated intravascular coagulation. 2015;56(2):169–176.
34. Wada H, Thachil J, Di Nisio M, et al. Harmonized guidance for disseminated intravascular coagulation from the International Society on Thrombosis and Haemostasis and the current status of anticoagulant therapy in Japan: a rebuttal. J Thromb Haemost. 2013;11(11):2078–2079.
35. Wada H, Matsumoto T, Yamashita Y. Diagnosis and treatment of disseminated intravascular coagulation (DIC) according to four DIC guidelines. J Intensive Care. 2014;2(1):15.
36. Lippi G, Favaloro EJ, Cervellin G. A review of the value of D-Dimer testing for prediction of recurrent venous thromboembolism with increasing age. Semin Throm Hemost 2014;40(6) 634-639.
37. Koenig W, Rothenbacher D, Hoffmeister A, Griesshammer M, Brenner H. Plasma fibrin D-dimer levels and risk of stable coronary artery disease: results of a large case-control study. Arterioscler Thromb Vasc Biol. 2001;21(10):1701–1705.
38. Kim HC, Greenland P, Rossouw JE, et al. Multimarker prediction of coronary heart disease risk: the Women's Health Initiative. J Am Coll Cardiol. 2010;55(19):2080–2091.
39. Marcucci R., Gori A. et al. Markers of hypercoagulability and inflation predict mortality in patients with heart failure // Ibid. 2006. Vol. 4. P. 1017–1022.
40. Abbassi-Ghanavati M, Greer LG, Cunningham FG. Pregnancy and laboratory studies: a reference table for clinicians. Obstet Gynecol. 2009 Dec;114(6):1326-31.
41. Arora M, Wun T. Adverse impact of venous thromboembolism on patients with cancer. Semin Thromb Hemost. 2014;40(3):313–318.
42. Stricker H. Venous thromboembolism and cancer: pathophysiology and incidence. Vasa. 2014;43(4):239–243.
43. Blackwell K, Hurwitz H, Liebe´ rman G, et al. Circulating D-dimer levels are better predictors of overall survival and disease progression than carcinoembryonic antigen levels in patients with metastatic colorectal carcinoma. Cancer. 2004;101(1):77–82.
44. Kilic M, Yoldas O, Keskek M, et al. Prognostic value of plasma D-dimer levels in patients with colorectal cancer. Colorectal Dis. 2008;10(3):238–241.
45. Khoury JD, Adcock DM, Chan F, et al. Increases in quantitative D-dimer levels correlate with progressive disease better than circulating tumor cell counts in patients with refractory prostate cancer. Am J Clin Pathol. 2010;134(6):964–969.
46. Ay C, Dunkler D, Pirker R, et al. High D-dimer levels are associated with poor prognosis in cancer patients. Haematologica. 2012;97(8):1158–1164.
47. Yamamoto M, Yoshinaga K, Matsuyama A, et al. Plasma D-dimer level as a mortality predictor in patients with advanced or recurrent colorectal cancer. Oncology. 2012;83(1):10–15.
48. Liu L, Zhang X, Yan B, et al. Elevated plasma D-dimer levels correlate with long term survival of gastric cancer patients. PLoS One. 2014;9(3):e90547.
49. Zhang X, Liu ZQ, Zhang W, Xu Q. A retrospective analysis of plasma Ddimer dynamic variation in terminal stage cancer patients: implications for disease progression. Int J Clin Exp Med. 2014;7(8):2395–2401.
50. Sakurai M, Satoh T, Matsumoto K, et al. High pretreatment plasma Ddimer levels are associated with poor prognosis in patients with ovarian cancer independently of venous thromboembolism and tumor extension. Int J Gynecol Cancer. 2015;25(4):593–598.
51. Wang Y, Wang Z. Predictive value of plasma D-dimer levels in patients with advanced non-small-cell lung cancer. Onco Targets Ther. 2015;8:805–808.
52. Fukumoto K, Taniguchi T, Usami N, et al. The preoperative plasma D-dimer level is an independent prognostic factor in patients with completely resected non-small cell lung cancer. Surg Today. 2015;45(1):63–67.