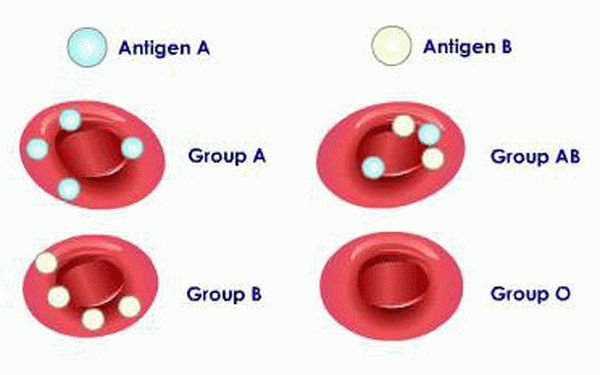
The blood of each person has its own characteristics and characteristics. It is determined by specific proteins - antigens found on the surface of red blood cells, as well as natural antibodies to them contained in plasma.
There are many possible combinations of antigens. Nowadays, the AB0 and Rh systems are used to classify blood. Based on them, four varieties are distinguished: 0, A, B, AB, or in other words - I, II, II, IV. In turn, each of them can be Rh-positive or Rh-negative. Many may have a question about how blood type and Rh factor are inherited.
These characteristics are inherited from parents and are formed in the mother's womb. Antigens on the surface of red cells appear by two to three months, and at the time of birth they are already accurately determined. From about three months, natural antibodies to antigens are detected in the serum, and only by ten years do they reach their maximum titer.
Boy or...
For many centuries, the blame for the lack of an heir in the family was placed on the woman.
To achieve the goal of having a boy, women resorted to diets and calculated favorable days for conception. But let's look at the problem from a scientific point of view. Human sex cells (eggs and sperm) have half the set of chromosomes (that is, there are 23 of them). 22 of them are the same for men and women. Only the last pair is different. In women these are XX chromosomes, and in men they are XY. So the probability of having a child of one sex or another depends entirely on the chromosome set of the sperm that managed to fertilize the egg. To put it simply, the father is entirely responsible for the gender of the child!
Is character inherited?
Many human traits depend on several genes. In addition, some of them, for example, character traits or intellectual abilities, cannot be explained only by the rules of inheritance. Think for yourself, throughout a person’s life, in addition to heredity, he is also influenced by the environment in which he lives. It depends on her whether our inclinations will manifest themselves, and if so, how. But some diseases, which are characterized by behavioral disorders, are inherited (for example, a tendency to depression, or cases of mental retardation associated with a diseased X chromosome).
What else can a child inherit?
Modern technologies make it easier to determine the phenotype (hair and eye color) of the unborn child. It is also now possible to determine the physiological and anatomical characteristics of the baby during its development in the womb. Phenotypic traits also depend on blood type inheritance.
Dominant characteristics include brown eyes and curly hair. Genetic research allows you to determine which trait will be dominant and which will be recessive.
According to statistics, children are least likely to inherit from their parents:
- fair skin;
- blue or gray eyes;
- soft straight hair.

Rarity of inheritance
Patterns of inheritance of the Rh factor by children
Currently, there are 48 antigens of the Rhesus system. The main clinically significant antigen is the Rh (D) antigen (in common parlance this is the “Rh factor”).
Persons who have this antigen on their red blood cells are classified as Rh-positive, and those who do not have this antigen are classified as Rh-negative.
Antigen D is protein in nature and has its own varieties: D-variant antigen and D-weak antigen.
The first differs from the usual one in quantitative changes in the structure (contains fewer structural areas), the second - in qualitative ones (structural areas are located far from each other), which makes it difficult to identify the D antigen and often leads to an incorrect interpretation of the result about Rh-negative blood.
During routine Rh blood testing, it is difficult to distinguish between variant and weak antigens, so to prevent sensitization to the D antigen, recipients containing these antigens are classified as Rh negative and donors are classified as Rh positive.
The gene encoding Rh (D) is dominant, and the d gene is recessive. Thus, in accordance with the patterns of inheritance of the Rh blood factor, Rh-positive individuals have the DD or Dd genotype, and Rh-negative individuals have the dd genotype.
Table “Children’s inheritance of the Rh blood factor from their parents”:
| Parent 1 | Parent 2 | Children |
| DD | DD | D (+) |
| DD | Dd | D (+) |
| Dd | Dd | 75% — D(+), 25% — d (-) |
| Dd | dd | 50% - d (-), 50% - D (+) |
| DD | dd | D (+) |
| dd | dd | d(-) |
Determination of the Rh factor (Rh factor) is carried out during transfusion of blood and its components, during planning and management of pregnancy.
Incompatibility occurs when an Rh-negative patient is transfused with Rh-positive blood or an Rh-negative woman is pregnant with an Rh-positive fetus. In this situation, Rh (-) individuals begin to produce antibodies that destroy red blood cells.
When incompatible blood is transfused, life-threatening transfusion complications develop. During pregnancy, an immunological conflict develops between mother and fetus, which can lead to hemolytic disease of the newborn (HDN) or termination of pregnancy. If a woman has antigen D and the fetal Rh factor is negative, then there is no danger of inheriting diseases or developing complications.
Taking into account the factor of inheritance of a person's Rh factor, currently, starting from the 10th week of pregnancy, it is possible to isolate fetal DNA from the mother's blood and determine the Rh factor. This genetic study provides an answer with 100% probability about the presence or absence of the RHD gene, which is responsible for the synthesis of the D antigen.
Inheritance of blood groups. Inheritance of the Rh factor. Rhesus conflict.
AB0 system.
Antigenic differences in human erythrocytes were first identified in 1900 by K. Landsteiner. Blood groups of the AB0 system (“a”, “b”, “zero”) are controlled by one autosomal gene I (from the word isohemagglutinogen) or ABO, located in the long arm of chromosome 9. In this gene, 3 alleles IA, IB and I 0 have been identified. The IA and IB alleles are codominant to each other, and they are both dominant to the I 0 allele. Thus, when different alleles are combined, 4 blood groups can be formed: 0 or I with genotype I 0 I 0, A or II with genotypes IAIA and IAI 0, B or III with genotypes IBIB and IBI 0 and AB or IV with genotype IAIB in ratio 1:3:3:2 – table. 5.
Table 5. Punnett grid for blood groups of the AB0 system
| Alleles | I.A. | I.B. | I 0 |
| I.A. | IAIA – A(II) | IAIB – AB(IY) | IAI 0 – A(II) |
| I.B. | IAIB – AB(IY) | IBIB – B(III) | IBI 0 – B(III) |
| IO | IAI 0 – A(II) | IBI 0 – B(III) | I 0 I 0 – 0(I) |
Blood groups determine the immunological properties of the agglutinogen antigen localized on the surface of red blood cells and the agglutinin antibody that interacts with them, dissolved in the blood serum.
With the rarest blood group 0(I), which occurs in the population with a frequency of 11% (1:9), antibodies against A
and
V.
_
If a person with blood group 0(I) is added to blood of any other group, agglutination (clumping) of red blood cells will occur and hemolytic shock will develop. At the same time, group 0(I) blood does not contain erythrocyte antigens, and it can be transfused to any recipient, regardless of their blood type. Therefore, people with blood type 0(I) are “universal donors”. In blood groups A(II) and B(III), each of which occurs in approximately a third of the population, antibodies are present in the blood serum, respectively, against either the B
or the
A
. Therefore, people with these blood groups can be transfused with either blood of the same group or blood of group 0 (I). With the fourth blood group AB(IV), antibodies against erythrocyte antigens are not produced in the blood serum. These people can be transfused with blood of any type, thus they are “universal recipients”. However, their blood can only be transfused to people with the same fourth blood group AB(IV). Since knowledge of a person’s blood group according to the AB0 system is a necessary condition for safe blood transfusion, we will once again present the patterns described above in tabular form - table. 7.
Table 7. Compatibility (+) of blood groups according to the AB0 system
| Recipient's blood type | Donor's blood type | |||
| 0(I) | A(II) | B(III) | AB(IV) | |
| 0(I) | + | – | – | – |
| A(II) | + | + | – | – |
| B(III) | + | – | + | – |
| AB(IV) | + | + | + | + |
Rh blood groups
.
Another group antigen system, called the Rh factor (Rh) system, is under more complex genetic control. This system includes three pairs of antigens ( D, C/c, E/e
), encoded by two closely linked, highly homologous genes located on the short arm of chromosome 1 -
RHD
and
RHCE
.
Apparently, these two genes arose during evolution as a result of duplication from a common ancestral gene. The main role in the Rh system belongs to the D
, the product of the
RHD
.
When it is present on the surface of red blood cells, the blood is Rh positive. C/c
and
E/e
antigens are encoded by the
RHCE
and are produced by alternative splicing.
The Rh-negative phenotype is formed in the absence of the D
RHD
gene is deleted . From 0.2% to 1% of people have a special “weak” variant of the
D
, designated
D u
.
This phenotype is caused by mutations in the RHD
.
Carriers of the D u
phenotype are also Rh-negative and can only be transfused with Rh-negative blood.
In fact, the genetic control of AB0 and Rh blood groups is more complex, since there are a large number of genes that have a modifying effect on these systems. Suffice it to say that more than 46 Rh antigens have now been identified. However, regardless of the details of the relationship between these antigens, the basic rule remains unchanged: Rh-negative blood is determined by the absence or deficiency of the D
.
Knowledge of group affiliation according to the Rh system is of great importance for preventing Rh conflict between mother and fetus, which can arise during pregnancy. The frequency of people with Rh positive – Rh(+) is 85%, the remaining 15% are Rh negative – Rh(-). If a Rh-negative woman has a Rh-positive husband, then with a high probability the child will be Rh-positive, and then a Rh-conflict may arise between the fetus and the mother. In 15% of such cases, after the 7th week, when mature red blood cells appear in the fetal blood, specific anti-Rh antibodies may begin to be produced in the blood of pregnant women with Rh(-). Through the placenta they enter the fetal blood and in some cases can accumulate there in large quantities, causing agglutination of red blood cells and their destruction. As a rule, the first pregnancy ends successfully; stillbirths and miscarriages are rare. The likelihood of Rh conflict occurring is especially high during repeated pregnancies of an Rh(-) woman. During childbirth, about 1 ml of fetal blood can enter the mother's bloodstream, and after the first birth, the Rh-negative mother will be sensitized to the baby's Rh-positive antigens. Similar sensitization can occur during abortion, although with less likelihood. During subsequent pregnancies with an Rh-incompatible fetus, the titer of anti-Rh antibodies in the woman’s blood can increase sharply. The consequence of this process may be the destruction of the red blood cells of the fetus and the formation of hemolytic disease, manifested by anemia, jaundice, edema and causing complex intellectual defects, hearing and speech disorders, and movement disorders. Often, newborns with hemolytic disease caused by Rh conflict develop severe cerebral palsy with epileptic disease and significant mental retardation.
The degree of damage to the central nervous system and other organs depends on the level of indirect bilirubin entering the blood from destroyed red blood cells and the duration of hyperbilirubinemia. This process leads to toxic-anoxic brain damage - bilirubin encephalopathy. The most effective treatment for hemolytic disease of newborns is exchange blood transfusion in the first day of life (and sometimes in utero), which helps remove hemolysis products and maternal antibodies from the blood of a sick child.
This is interesting: Inheritance of a mortgaged apartment by minors 2021
To prevent Rh conflict and hemolytic disease in the fetus, a woman with a negative Rh factor during any intrauterine intervention during the first pregnancy (medical abortion, spontaneous miscarriage with subsequent curettage, childbirth) is advised to administer anti-D immunoglobulin. This drug reduces the Rh sensitization of the pregnant woman, that is, her sensitivity to the Rh factor and, accordingly, the formation of Rh antibodies. The administration of anti-D immunoglobulin during repeated pregnancies is not indicated, since the woman is already sensitized, that is, sensitive to the Rh factor, and has Rh antibodies. A woman with Rh(-) should definitely discuss with a geneticist the problems of preventing the birth of a child with the consequences of bilirubin encephalopathy in the form of severe cerebral palsy.
In rare cases, a conflict also arises according to the AB0 system, but it occurs in a much milder form than with a Rh conflict. Therefore, future parents should know their blood group not only according to Rh, but also according to the AB0 system.
Didn't find what you were looking for? Use the search:
Rh blood incompatibility
If the mother's blood is Rh negative and the child's blood is Rh positive, then the fetus may become ill. The mother's body begins to produce antibodies against the child's Rh factor. Antibodies, penetrating into his blood through the placenta, cause the fetus's red blood cells to stick together and then destroy them. With repeated pregnancies, the Rh conflict becomes more and more pronounced, since the mother's Rh antibodies are retained from previous pregnancies and, therefore, the danger to the child increases.
Since the Rh factor appears in the blood of the fetus before the 12th week of intrauterine development, the destructive effect on the child’s blood will be long-lasting and will cause serious disturbances in his life - due to a lack of red blood cells, the fetus develops hypoxia of tissues and organs, severe chronic anemia, and profound disorders metabolism and blood circulation. The child may die in the womb or be born with a hemolytic disease.
Mendel's law
Mendel studied the transmission of genes from parents to offspring, as a result of which he made conclusions about how certain traits are inherited. He formalized these conclusions in the form of laws.
He learned that a child receives one gene from each parent, so a child in a pair of genes has one gene from the mother and the other from the father. In this case, the inherited trait may manifest itself (it is called dominant) or not manifest itself (it is recessive).
With regard to blood groups, Mendel found that genes A and B are dominant (they encode the presence of antigens on the surface of red blood cells), and gene 0 is recessive. This means that when genes A and B are combined, both genes will encode the presence of agglutinogens, and the blood group will be the fourth. If genes A and 0 or B and 0 are passed on to the child, then the recessive gene will not manifest itself; accordingly, in the first case there will be only agglutinogens A (the child will have group 2), and in the second - agglutinogens B (the child will have the third group) .
Inheritance of blood type and Rh factor
Inheritance of a baby's blood type is an important and controversial issue. Since the child does not always receive a group that matches the group of one of the parents, and because of this, disagreements may arise in the family. To avoid unfounded accusations, both parents must understand the issue of the child’s inheritance of genes.
This is interesting: Inheritance of traits in dogs 2021

What is the Rh factor?
Human blood consists of red cells - erythrocytes. In some cases, group D antigens are present on their surface, in such situations they speak of positive Rhesus. These substances are present in the blood of approximately 85% of people, the remaining 15% have a negative Rh factor, that is, they do not have these antigens. There are other antigens in the blood, but their presence is not so important during blood transfusion or pregnancy.
Transfusion of Rh-positive blood to a person with a negative Rh factor leads to the destruction of red blood cells, which causes so-called pathological hemolysis - this is how the immune response to unfamiliar substances manifests itself. People with negative Rhesus need to be careful when receiving blood transfusions
You should also pay attention to your Rh factor when planning pregnancy: negative Rh of the mother and positive of the father can cause Rh conflict and lead to the development of hemolytic jaundice in the child, stillbirth or death of the infant
Rh-positive people can receive blood transfusions with any Rh factor, and pregnant women with such blood should not be afraid of conflict, even if the father is Rh-negative.
What is the effect of parental heterozygosity?
With heterozygous rhesus, a woman often has problems carrying a pregnancy, since in this case the mother and child have a rhesus conflict and a specific protein rejects the fertilized egg as a foreign organism. There is a high risk of miscarriage. Inheritance of blood type and Rh factor in most cases depends on the homozygosity or heterozygosity of the parents.
The appearance of hemolytic jaundice in a child is also the cause of conflict between the blood group of the mother (in the case when the pregnant woman has the first group) and the fetus, or between the Rhesus of the mother and the child.
Where do genetic “damages” come from?
The cells of our body are constantly dividing so that old and dead ones are replaced by new ones. Each time a new cell is formed, the hereditary material contained in the DNA is copied. When copying, errors (mutations) often occur: either a fragment of DNA is lost, or one of its sections is copied incorrectly. Our immune cells find these breakdowns and eliminate them. When this does not happen, the mutant cells pass on erroneous information to their daughter cells when they subsequently divide. Such errors can cause genetic diseases and cancer tumors in the “host” body, and mutations in germ cells (sperm and eggs) can be transmitted to children.
Fortunately, prudent nature created two copies of genes (all chromosomes, with the exception of sex chromosomes in men, as we remember, are paired). If the mutation occurs in one recessive gene, nothing bad will happen. A genetic disease will begin if he “meets” a second exactly the same gene or a “breakdown” occurs in the dominant gene.
Emotions, obesity and even suicidal tendencies
Due to epigenetic inheritance, many characteristics can be passed on to us depending on the environmental factors and lifestyle choices of our parents. Men who take up smoking before puberty are more likely, for example, to have sons who are overweight or obese in the future.
Epigenetics provides more and more evidence that from generation to generation, we can pass on not only functions such as eating habits and weight, but also tendencies towards certain emotions. Mainly due to trauma, intense experiences that are reflected in the cellular memory that our ancestors pass on to us, although genes may not necessarily be involved.
World-renowned neuroscientist Michael Mainey of McGill University in Montreal, who has devoted himself to studying the brains of suicides, has been trying for years to determine why suicide is more common in some families. He was able to notice that areas of the brain of suicidal individuals involved in emotions, genes involved in stress, and the weakening of these genes were associated with psychological immunity and stress management. Interestingly, compared to the brains of accident victims who did not have psychological problems or depression, etc., there were obvious differences in suicidal minds. Why is this happening?
Blood group compatibility
It is noteworthy that some doctors performed blood transfusions back in the 17th century. However, this had little to do with medical research and actual treatment of people. For example, the French doctor Jean-Baptiste Denis treated aggressive patients with mental disorders by transfusing them with the blood of lambs. According to the doctor, the gentleness of the cute animal was supposed to soften the patient’s violent temper. Fortunately, the court prohibited such methods of treatment. However, Themis’s decision was made only after one of Denis’s charges died after a dangerous manipulation.
In the 19th century, blood transfusion was actively pursued in England. The first successful blood transfusion in Russia was carried out in 1832. As a result of the manipulation, G. Wolf managed to save a patient with uterine bleeding that occurred after a difficult birth.
Naturally, transfusions often ended in complications, because no one determined the compatibility of blood groups. The conditions for compatibility of blood of different patients were considered only at the beginning of the 20th century.
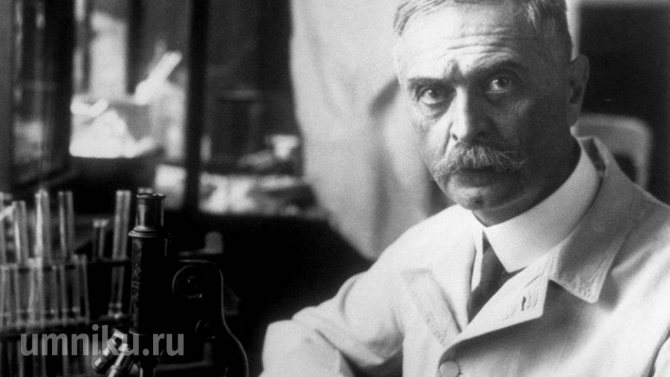
Karl Landsteiner
The Austrian immunologist Karl Landsteiner first drew attention to the individual differences in human blood. He confirmed his assumptions experimentally, mixing the blood serum of some patients with red blood cells from other donors. The reactions of the components clumping together, which manifested themselves in some cases, made it possible to identify 4 blood groups, which became the basis of the AB0 system
Later, in 1930, Landsteiner received the Nobel Prize for his invaluable discoveries.
The aggregation reactions of components, which manifested themselves in some cases, made it possible to identify 4 blood groups, which became the basis of the AB0 system. Later, in 1930, Landsteiner received the Nobel Prize for his invaluable discoveries.
The compatibility of the blood groups of the donor and the patient is clearly presented in the table:

Blood groups: transfusion compatibility table
Thus, the owner of the first blood group is a universal donor, and the owner of the fourth is a universal recipient.
What are Rh antibodies and how do they affect the fetus?
Rh antibodies are compounds of a protein structure that are produced in the mother's body in response to the ingestion of Rh-positive red blood cells from the fetus (the expectant mother's immune system perceives these red blood cells as foreign). If Rh antibodies are detected in the mother's bloodstream, the obstetrician makes a diagnosis: Rh sensitization. This occurs with artificial or spontaneous termination of an uterine or ectopic pregnancy. Rh antibodies can also appear after the first birth if the born child is Rh positive (during childbirth, the baby’s blood enters the mother’s bloodstream, causing a corresponding reaction). Sensitization of the body of a Rh-negative woman is also possible through transfusions of Rh-incompatible blood (even if such transfusions were carried out in early childhood).
The process of immunization of a pregnant woman begins with the formation of Rh antigens in the red blood cells of the fetus. Since antigens of the Rh system are contained in the blood of the fetus from 7-8 weeks of pregnancy, in some cases early sensitization of the mother’s body is possible. However, in the vast majority of cases, the first pregnancy in a Rh-negative woman (in the absence of previous sensitization of the body) proceeds without complications. The risk of developing Rh sensitization increases with subsequent pregnancies, especially if the first pregnancy is terminated, bleeding during the first pregnancy, with manual separation of the placenta, and also if the birth is performed by caesarean section or is accompanied by significant blood loss. This is explained by the fact that with the listed complications, there is a high probability of a large number of Rh-positive red blood cells entering the maternal bloodstream and, as a result, the formation of a large number of Rh antibodies. In addition, during the first pregnancy, the immune system of the expectant mother encounters Rh-positive red blood cells of the fetus for the first time. Therefore, not so many antibodies are produced: approximately as much as is needed to destroy fetal red blood cells entering the mother’s blood. In addition, these antibodies belong to class M immunoglobulins, which are large in size and poorly penetrate through the placenta to the fetus. But after childbirth, “memory cells” remain in the woman’s body, which in subsequent pregnancies will be able to “organize” the rapid and powerful production of antibodies against the Rh factor. These will be antibodies of a different type - class G immunoglobulins, which are smaller in size than immunoglobulins M, and therefore penetrate the placenta more easily and are more aggressive. Therefore, the reaction of the female immune system to the Rh antigen of the fetus during the second and third pregnancy is much faster and more severe than during the first. Accordingly, the risk of fetal damage is higher.
According to medical literature, after the first pregnancy, immunization occurs in 10% of women. If a woman with Rh-negative blood avoids Rh immunization after her first pregnancy, then the next pregnancy with an Rh-positive fetus, the probability of immunization again is 10%.
Rh sensitization does not harm the health of the expectant mother, but it can pose a danger to the child. Once in the bloodstream of the fetus, Rh antibodies destroy its red blood cells, causing anemia (decreased hemoglobin), intoxication, and dysfunction of vital organs and systems. This condition is called hemolytic disease (hemolysis - destruction of red blood cells).
The breakdown of red blood cells leads to damage to the kidneys and brain of the fetus. As red blood cells are continuously destroyed, his liver and spleen try to speed up the production of new red blood cells, while increasing in size. In the end, they too fail. Severe oxygen starvation sets in, and a new round of severe disorders begins in the child’s body. In the most severe cases, this ends in intrauterine death at various stages of pregnancy; in milder cases, the Rh conflict manifests itself after birth as jaundice or anemia of the newborn. Most often, hemolytic disease quickly develops in a child after birth, which is facilitated by the entry of a large number of antibodies into the baby’s blood when the integrity of the placental vessels is disrupted.
Treatment of hemolytic disease is complex and complex; sometimes the baby requires a replacement blood transfusion. Doctors inject him with Rh-negative blood of his type and carry out resuscitation measures. This operation must be performed within 36 hours after the baby is born.
BIOLOGY TICKETS / from 21 to 30 / 24
1. No. 24
Inheritance of blood groups.
Inheritance of the Rh factor. Rhesus conflict. Inheritance of blood groups.
The laws of inheritance of blood groups are based on the following concepts. At the ABO gene locus, there are three possible variants (alleles) - 0, A and B, which are expressed in an autosomal codominant manner. This means that individuals who have inherited genes A and B express the products of both of these genes, resulting in the AB (IV) phenotype. Phenotype A (II) can be present in a person who has inherited from parents either two genes A, or genes A and 0. Accordingly, phenotype B (III) - when inheriting either two genes B, or B and 0. Phenotype 0 (I) appears when inheritance of two genes 0. Thus, if both parents have blood group II (genotypes AA or A0), one of their children may have the first group (genotype 00). If one of the parents has blood type A(II) with a possible genotype AA and A0, and the other has B(III) with a possible genotype BB or B0, children can have blood groups 0(I), A(II), B(III) ) or AB (IV).
Inheritance of the Rh factor is encoded by three pairs of genes and occurs independently of the inheritance of blood type. The most significant gene is designated by the Latin letter D. It can be dominant - D, or recessive - d. The genotype of a Rh-positive person can be homozygous - DD, or heterozygous - Dd. The genotype of a Rh negative person may be dd.
Hemolytic disease of the fetus and newborn is a condition that occurs as a result of incompatibility of the blood of mother and fetus for certain antigens. Most often, hemolytic disease of the newborn develops due to Rh conflict. In this case, the pregnant woman has Rh-negative blood, and the fetus has Rh-positive blood. During pregnancy, the Rh factor with the red blood cells of the Rh-positive fetus enters the blood of the Rh-negative mother and causes the formation of antibodies to the Rh factor in her blood (harmless to her, but causing the destruction of the fetal red blood cells). The breakdown of red blood cells leads to damage to the liver, kidneys, brain of the fetus, and the development of hemolytic disease of the fetus and newborn. In most cases, the disease develops quickly after birth, which is facilitated by the entry of a large number of antibodies into the baby’s blood when the integrity of the placental vessels is disrupted.
2. No. 62 Evolution and ontogeny. Biogenetic law of Müller-Haeckel.
biogenetic law
a pattern in living nature formulated by the German scientist E. Haeckel (1866) and consisting in the fact that the individual development of an individual (
ontogenesis
) is a short and rapid repetition of the most important stages of the evolution of the species (
phylogeny
). Facts indicating recapitulation (for example, laying in embryos terrestrial vertebrate gill slits, embryologist F. Müller in 1864 supported the principle of recapitulation with data from the history of the development of crustaceans.
Around B. z. A long and heated discussion ensued. Haeckel’s original idea of the direct order of reproduction of stages in the history of the species in the development of an individual also turned out to be untenable. It was shown (including by Haeckel himself) that heterochronies
,
heterotopia
, embryonic adaptations,
reduction
and other processes profoundly change the course of ontogenesis, excluding the possibility of direct recapitulation of ancestral characteristics.
3. No. 102 Hookworms. Systematics, morphology, development cycle, routes of infection, laboratory diagnostics, prevention, pathogenic effect. Geographical distribution.
Ankylostoma duodenale and Necator americanus
both species belong to the family.
Hookworms. They differ from each other in the shape of the oral capsule and the characteristics of their geographical distribution. The crooked head has four chitinous teeth in the oral cavity, and the necator has two wide, crescent-shaped cutting plates. Both parasites are widely distributed throughout the tropical and subtropical zones, but necator is more common in zones with hotter climates. Otherwise, both types are so similar that even the diseases caused by them are not differentiated and are called hookworm.
The size of hookworms is about 10 mm. The head end is bent to the ventral side; eggs are oval, transparent, up to 60 microns long.
Life cycle
hookworms are unique and indicate their close connection with free-living ancestral forms. Eggs that fall into the soil develop quickly, and larvae soon emerge from them, which, molting twice, become invasive after a few months and can enter the human body either with soil-contaminated vegetables and fruits, or through active penetration through the skin.
This feature provides the possibility of the existence of underground foci of hookworm disease in mines located in temperate zones. The main condition for the occurrence of such outbreaks is high soil moisture and contamination with feces. Once in the blood, the larvae make a path through the vessels that is characteristic of all types of helminths of this group. Final localization
- the duodenum, to the villi of which they are attached by oral capsules, damaging them and feeding on blood and cells of the mucous membrane. Both parasites secrete anticoagulant substances into wounds and can cause intestinal bleeding and allergization of patients.
Laboratory diagnostics
- as with all geohelminthiasis.
Prevention
- in addition to the general measures described above, it is mandatory to wear shoes in areas where these diseases are common.
Rh factor inheritance
a person with the second blood group may have AA antigens, where the first A is dominant, the second A is recessive. A may have AB, where the first A is a dominant, determining his existing blood type, and B is a suppressed trait that does not manifest itself in any way. But, it can be inherited and appear in the offspring if it encounters a recessive trait similar to itself. So what kind of blood inheritance will the future child receive?
The blood type of a child based on his parents is calculated by the laws of inheritance; according to the same laws, there are impossible options:
- One of the partners has the fourth blood group; a baby with the first group will never be born in this family, regardless of the blood type of the second parent.
- If, on the contrary, one of the parents has blood group 1, this family will never have children with group 4.
There are other cases when the child’s blood type does not match the parents’, but this is a completely natural result of mixing the 2nd group and the 3rd. This is a unique variation in which children can have any blood type.
The table clearly demonstrates the possible blood groups of a child.
Inheritance of blood groups
Another classification that is of utmost importance is the Rh factor. Blood rhesus is a protein compound found on the membranes of red blood cells. Its purpose in the body is not entirely clear, however, about 85% of the world's population has this protein as part of cell membranes. This population is called Rh-positive, those percentages that do not have it are, accordingly, Rh-negative.
However, all of the above is true for an Rh-negative mother and an Rh-positive baby. If the mother has Rh and the baby has Rh, there is no conflict. Therefore, examination and blood testing for the Rh factor is mandatory for a pregnant woman. Rh protein is passed on to the child according to the same general rules of genetic inheritance. In most people, factor D (the presence of protein) is dominant, and factor d (its absence) is recessive.
Inheritance of Rh factor
- The most common situation is DD DD, in this case there is no threat to pregnancy
- With the DD Dd option, there will also be no problems with the Rh protein
- Situation Dd Dd is risky, but percentage-wise safer than the following
- Dd dd, here the occurrence of Rh conflict occurs in half of the cases.
Parents often wonder whether the blood type of parents and children can be different? Yes, this is possible. The fact is that inheritance of a child’s blood type occurs according to the law of genetics, where genes A and B are dominant, and genes O are recessive. The baby receives one gene each from his mother and father. Most genes in humans have two copies.
| Parents' blood types | Possible blood type of the child | |||
| II | I (100%) | — | — | — |
| I II | I (50%) | II (50%) | — | — |
| I III | I (50%) | — | III (50%) | — |
| I IV | — | II (50%) | III (50%) | — |
| II II | I (25%) | II (75%) | — | — |
| II III | I (25%) | II (25%) | III (50%) | IV (25%) |
| II IV | — | II (50%) | III (25%) | IV (25%) |
| III III | I (25%) | — | III (75%) | — |
| III IV | — | II (25%) | III (50%) | IV (25%) |
| IV IV | — | II (25%) | III (25%) | IV (50%) |
It is worth paying attention to a number of patterns in the inheritance of traits. Thus, the blood type of children and parents must match 100% if both parents have the first. In cases where parents have groups 1 and 2 or groups 1 and 3, children can equally inherit any trait from one of the parents
In cases where parents have groups 1 and 2 or groups 1 and 3, children can equally inherit any trait from one of the parents.
The situation with Rh inheritance is much simpler: the D antigen is either present or absent. A positive Rh factor is dominant over a negative one. Accordingly, the following subgroups are possible: DD, Dd, dd, where D is a dominant gene and d is a recessive gene. From the above it is clear that the first two combinations will be positive, and only the last one will be negative.
In life, this situation will look like this. If at least one parent has DD, then the child will inherit a positive Rh factor, if both have DD, then a negative one. If the parents have Dd, there is a possibility of having a child with any rhesus factor.
Inheritance table of Rh blood factor
Rh inheritance
It is possible to say exactly which Rh factor a child will inherit only in one case: if both parents have a negative Rh status. All offspring of this couple will be Rh negative. In all other cases, Rh can be anything.
The question arises why the Rh factor is inherited this way if both the man and the woman are Rh positive. In fact, the explanation is very simple. The fact is that positive Rh is determined by the D gene, which can have different alleles: one dominant (D), the other recessive (d). That is, a person with Rh(+) has the genotype DD (homozygous) or Dd (heterozygous). The genotype of a person with Rh(-) is designated as dd. Thus, the probability that a couple with Rh(+) will have a child with negative Rh is 25%. This can happen if both the mother and father have a heterozygous genotype - Dd. Possible Rh factor options in this case are DD, Dd, Dd, dd. Heterozygosity is caused by the birth of Rh-conflicting children in an Rh-negative woman.
You can independently determine the likelihood of offspring with a particular Rh. For example, the mother is negative, that is, she has the dd genotype, the father is positive, that is, she has the DD or Dd genotype. Possible options: Dd, Dd, Dd, dd, Dd, Dd, Dd, dd. If in this case the man is homozygous (DD), then the offspring of this couple will be Rh-positive with a probability of 100%. If a man is heterozygous (Dd), the chance of having Rh(-) in children is 50 percent.
Possible variants of the Rh factor that a child can inherit, depending on the Rh factor of the man and woman, are presented in the table below.
This is interesting: Inheritance by law by spouse 2021
| Mother's Rh factor | Father's Rh factor | (+) | (-) |
| (+) | any | any | |
| (-) | any | (-) |
What blood type does the child inherit?
What is blood type? Is it unchanged?
Blood groups are natural immunogenetic characteristics of the blood of mammals and humans. Which differ from each other in the characteristics of combinations of group isoantigens (agglutinogens) in red blood cells (erythrocytes) and their corresponding antibodies in plasma. Blood type is a hereditary trait; it begins to form from the very beginning of embryo development and remains constant throughout a person’s life.
However, medical practice knows exceptions to this rule. Changing the blood type is possible in severe forms of blood cancer, bone marrow transplantation, multiple blood transfusions in combination with bone or brain surgery.
Classification of blood groups and their designation
The erythrocytes (red blood cells) of each person contain a large number of antigens, which at the cellular and molecular level form group systems unrelated to each other. Each system consists of a pair or several pairs of antigens.
The world practice of medical laboratories includes more than 29 group blood systems. The most commonly used are: AB0, Kell, Duffy, Kid, Rh factor, MNSs.
In Russia and the CIS countries the AB0 system is used.
The AB0 group system, as a permanent feature, distinguishes the presence of isoantigens in erythrocytes and the presence of normal group antibodies (agglutinins) in the blood plasma.
AB0 system includes:
- 2 isoantigens, designated “A” and “B”
- 2 agglutinins, designated α and β
The ratio of A to anti-A (α) and B to anti-B (β) forms the four blood groups.
The first blood group is designated: 0 (I)
The second group is designated: A (II)
The third group is designated: B (III)
The fourth group is designated: AB (IV)
Determining group affiliation is very important in surgical practice when transfusing whole blood or its components. In obstetrics and gynecology when planning pregnancy and monitoring pregnant women
Rh factor or Rh system
Blood rhesus is a specific protein (antigen) that is located on the surface of red blood cells.
People whose red blood cells contain Rh are Rh positive.
People whose red blood cells do not contain Rh are Rh negative.
The Rh blood system is very complex, it contains more than 40 antigens, which are designated by different symbols and letters. The most common types of Rh antigens found in people are: D, C, E, e.
How is the Rh factor inherited?
If mom and dad have a positive Rh factor, most likely the child will inherit it. However, there is the possibility of inheritance through an indefinite number of generations, that is, a couple with a positive Rh factor may have a child with a negative Rh factor. A couple with a negative Rh factor can give birth to a baby with a positive Rh factor. If the parents have different Rh factors, the probability of the child being Rh positive is 75%, and the child’s Rh factor is negative – 25%.
How is blood type inherited?
The genetic law says: a child inherits from his parents not one of their blood groups, but a set of genes that determines it.
According to the AB0 system, a combination of three factors is potentially possible in red blood cells: A, B and 0. But only two genes can be inherited, for example, two A or two B, A0, B0 or AB.
The law of inheritance of Georg Mendel, the founder of species genetics, defines genes A and B as dominant (predominant), and gene 0 as recessive (oppressed, suppressed).
The first blood group can be inherited by a child when two recessive genes “00” are combined.
The second blood group can be inherited by a child with a combination of the parental genes “AA” and “A0”.
The third blood group is inherited by a child when a combination of the “BB” and “B0” genes is merged.
But the combination, so to speak, of equal genes A and B leads to the inheritance of a rare fourth blood group.
As can be seen from this law of genetics, a child can develop a blood type that neither of the parents has.
Thus, what blood type the child inherits can be guessed from the table below.
What should parents have?
If the Rh factor matches the parents, then the child acquires it with a probability of up to 100%. The test results for a baby born to people with a positive factor should be the same. In the case when the indicators of the parents differ, the blood of the offspring is formed with a dominant indicator. The probability of receiving Rh with a “+” or “-” sign is 50%.
The factor is determined simultaneously with the blood group according to the ABO system. The gene responsible for this trait is located on chromosome number 9. The indicator is formed under the influence of chromosomes responsible for other hereditary traits. The genetic code is passed on from parents, who receive it from grandparents.
Important information: Which blood group is suitable for all people (recipients) for transfusion and is there a universal one?
What is Rh conflict
The conflict manifests itself in the process of rejection of the fetus during gestation by a mother with a different Rh blood indicator. This means that the mother’s immune system mistakes the baby for a foreign body that is life-threatening. The body tries to get rid of it, which increases the risk of miscarriage. Such incompatibility occurs quite rarely, but can lead to a number of complications.
The fetus's red blood cells die under the influence of the mother's antibodies, which negatively affects the child's health and increases the risk of jaundice in the newborn. The likelihood of developing the following diseases also increases:
- pathologies of the central nervous system;
- damage to the brain and other internal organs - liver, spleen.
This can be avoided by controlling the amount of antibodies in the body. Regular testing of the expectant mother will help determine the risk of conflict. If necessary, specialists vaccinate her by intravenously injecting a drug containing anti-Rhesus immunoglobulin.
This can be done in the early stages, when the blood cells in the fetus have not yet formed. The presence of antibodies is checked from the 8th week of pregnancy. Every Rh-negative woman in labor needs constant medical supervision. In some cases, in the later stages, doctors may perform an early delivery to save the lives of the mother and baby.