An erythrocyte is a formed element of blood that, using hemoglobin, is capable of transporting oxygen to the tissues and carbon dioxide to the lungs. This is a simple cell in structure, which is of great importance for the life of mammals and other animals. The red blood cell is the most abundant cell type in the body: approximately a quarter of all cells in the body are red blood cells.
General principles of the existence of red blood cells
An erythrocyte is a cell derived from the red germ of hematopoiesis. About 2.4 million of these cells are produced per day, they enter the bloodstream and begin to perform their functions. During the experiments, it was determined that in an adult, red blood cells, the structure of which is significantly simplified compared to other cells of the body, live 100-120 days.
In all vertebrates (with rare exceptions), oxygen is transferred from the respiratory organs to the tissues through hemoglobin in erythrocytes. There are exceptions: all representatives of the family of “white-blooded” fish exist without hemoglobin, although they can synthesize it. Since at the temperature of their habitat, oxygen dissolves well in water and blood plasma, these fish do not require more massive oxygen carriers, which are erythrocytes.
Erythropoiesis
The development of red blood cells is a tightly regulated process to maintain sufficient oxygen delivery to the tissue. One of the important physiological functions of the bone marrow is erythropoiesis. In healthy adults, the bone marrow produces about 2.4 million red blood cells per second, which are released into the peripheral blood. Depending on demand, red blood cell production can be significantly adjusted and increased.
A complex network of oxygen sensors, cytokines such as erythropoietin, and other factors, including regulators of iron metabolism, are involved in the control of steady-state and stress-induced erythropoiesis. Thereby ensuring proper oxygen supply to peripheral tissues. This regulatory network can adapt to physiological demands such as oxygen concentration or pregnancy, as well as pathological conditions such as blood loss. However, in some pathological conditions this regulatory network is overloaded or dysfunctional, leading to polycythemia or anemia.
Note! In older people, the bone marrow and other organs undergo aging. As a result, erythropoietin synthesis and red blood cell production may be reduced. However, even in very old people, red blood cell production and erythropoietin synthesis are usually sufficient to maintain hemoglobin levels within reasonable limits.
Every second, 2-3 million red blood cells are produced in the bone marrow and enter the bloodstream. Also known as red cells, they are a significant cell type, with each cubic millimeter of blood containing 4-6 million cells. Checking your red blood cell count is usually part of a complete blood count. It can be used to look for diseases such as anemia, dehydration and leukemia.
Erythrocytes of chordates
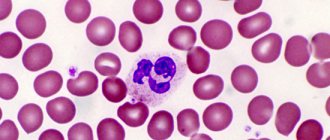
A cell such as an erythrocyte has a different structure depending on the class of chordates. For example, in fish, birds and amphibians, the morphology of these cells is similar. They differ only in size. The shape of red blood cells, volume, size, and the absence of certain organelles distinguish mammalian cells from others found in other chordates. There is also a pattern: mammalian red blood cells do not contain unnecessary organelles and a cell nucleus. They are much smaller, although they have a larger contact surface.
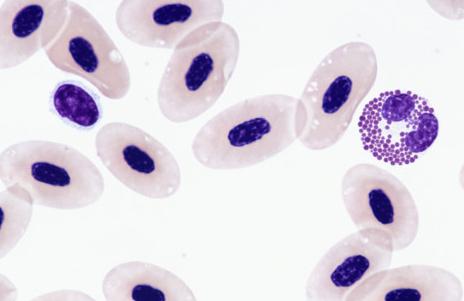
Considering the structure of frog and human erythrocytes, common features can be identified immediately. Both cells contain hemoglobin and are involved in oxygen transport. But human cells are smaller, oval and have two concave surfaces. The red blood cells of frogs (as well as birds, fish and amphibians, except salamanders) are spherical, they have a nucleus and cellular organelles that can be activated when necessary.
Human red blood cells, like the red blood cells of higher mammals, do not have nuclei or organelles. The size of goat red blood cells is 3-4 microns, human - 6.2-8.2 microns. In Amphiuma (tailed amphibian), the cell size is 70 microns. Obviously size is an important factor here. The human red blood cell, although smaller, has a larger surface due to two concavities.
The small size of cells and their large number have made it possible to greatly increase the ability of blood to bind oxygen, which now depends little on external conditions. And such structural features of human red blood cells are very important, because they allow you to feel comfortable in a certain habitat. This is a measure of adaptation to life on land, which began to develop in amphibians and fish (unfortunately, not all fish in the process of evolution had the opportunity to populate land), and reached the peak of development in higher mammals.
Red cell formation

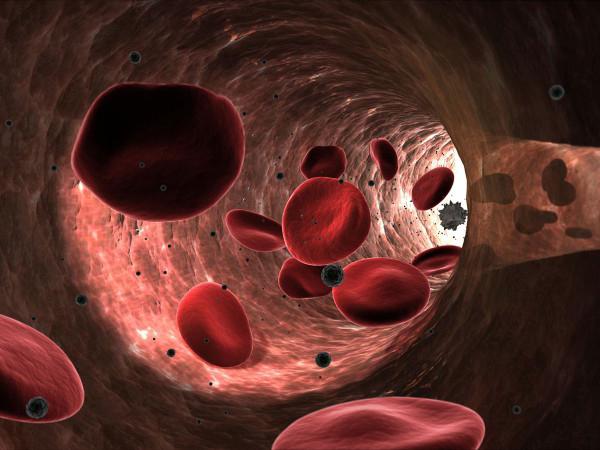
The production of red blood cells is controlled by erythropoietin, a hormone produced primarily by the kidneys. Red blood cells begin as immature cells in the bone marrow and, after about seven days of maturation, enter the bloodstream. They are the cellular component of blood, millions of which in the circulation of vertebrates give the blood its characteristic color and carry oxygen from the lungs to the tissues.
A mature human red blood cell is small, round and bivalve, appearing dumbbell-shaped in profile. The cell is flexible and takes on a bell shape as it passes through very small blood vessels. It is covered by a membrane made of lipids, has no nucleus, and contains hemoglobin and an iron-rich oxygen-binding protein.
The structure of human red blood cells
The structure of blood cells depends on the functions assigned to them. It is described from three angles:
- Features of the external structure.
- Component composition of an erythrocyte.
- Internal morphology.
Externally, in profile, an erythrocyte looks like a biconcave disk, and in front, like a round cell. The normal diameter is 6.2-8.2 microns.
More often, blood serum contains cells with slight differences in size. With iron deficiency, the run-up decreases, and anisocytosis (many cells with different sizes and diameters) is recognized in the blood smear. With a deficiency of folic acid or vitamin B12, the red blood cell enlarges to a megaloblast. Its size is approximately 10-12 microns. The volume of a normal cell (normocyte) is 76-110 cubic meters. µm.
The structure of red blood cells in the blood is not the only feature of these cells. Their number is much more important. Small sizes made it possible to increase their number and, consequently, the contact surface area. Oxygen is more actively captured by human red blood cells than by frogs. And it is most easily released into tissues from human red blood cells.
Quantity is really important. In particular, an adult human contains 4.5-5.5 million cells per cubic millimeter. A goat has about 13 million red blood cells per milliliter, while reptiles have only 0.5-1.6 million, and fish have 0.09-0.13 million per milliliter. In a newborn child, the number of red blood cells is about 6 million per milliliter, while in an elderly child it is less than 4 million per milliliter.
Structure of the CCP
Red blood cells have a structure that is strikingly different from other blood components, since they do not have a nucleus or chromosomes. This form of red blood cells makes it possible for the cells to squeeze through the thinnest capillaries and deliver oxygen to any cell. The size of a red blood cell is 7–8 microns.
The chemical composition of the bodies is as follows:
- 60% water;
- 40% dry residue.
The dry remainder of the component in the blood consists of 90–95% hemoglobin. The remaining 5–10% is occupied by lipids, carbohydrates, fats and enzymes, which ensure the function of red blood cells in the body.
The structure of red blood cells
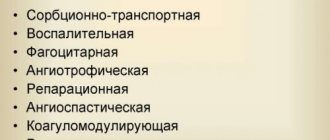
Functions of red blood cells
Red blood cells - red blood cells, the number, structure, functions and developmental features of which are described in this publication, are very important for humans. They implement some very important functions:
- transport oxygen to tissues;
- transport carbon dioxide from tissues to the lungs;
- bind toxic substances (glycated hemoglobin);
- participate in immune reactions (immune to viruses and, due to reactive oxygen species, can have a detrimental effect on blood infections);
- able to tolerate certain medications;
- participate in the implementation of hemostasis.
Let us continue to consider a cell such as an erythrocyte, its structure is maximally optimized for the implementation of the above functions. It is as light and mobile as possible, has a large contact surface for gas diffusion and chemical reactions with hemoglobin, and also quickly divides and replenishes losses in the peripheral blood. This is a highly specialized cell, the functions of which cannot yet be replaced.
Cell formation and life cycle
Red blood cells are formed from precursor cells that originate from stem cells. If for some reason the bone marrow is not able to produce CCT, these functions are taken over by the liver and spleen.
Red blood cells originate in flat bones - the skull, ribs, pelvic bones and sternum. The lifespan of red blood cells will depend on the general indicators of the functioning of the body, so it is impossible to definitively answer the question of how long red blood cells live. On average it is 3–3.5 months.
Every second, about 2 million cells disintegrate in the human body, and new ones are produced in return. Cell destruction, as a rule, occurs in the liver and spleen - instead of them, bilirubin and iron are formed.
Red cells can disintegrate not only due to physiological aging and death. The life cycle can be significantly shortened due to the following factors:
- under the influence of various toxic substances;
- due to hereditary diseases - the most common cause is spherocytosis.
The structure of erythrocytes is disc-shaped; when they disintegrate, the contents go into the plasma. But if hemolysis (the breakdown process) is too extensive, it can lead to a decrease in the number of moving bodies, causing hemolytic anemia.
Red blood cell membrane
A cell such as an erythrocyte has a very simple structure, which does not apply to its membrane. It is 3-layer. The mass fraction of the membrane is 10% of the cell membrane. It contains 90% proteins and only 10% lipids. This makes red blood cells special cells of the body, since in almost all other membranes lipids predominate over proteins.
The volumetric shape of red blood cells can change due to the fluidity of the cytoplasmic membrane. Outside the membrane itself there is a layer of surface proteins containing a large number of carbohydrate residues. These are glycopeptides, under which there is a bilayer of lipids, with their hydrophobic ends facing in and out of the erythrocyte. Under the membrane, on the inner surface, there is again a layer of proteins that do not have carbohydrate residues.
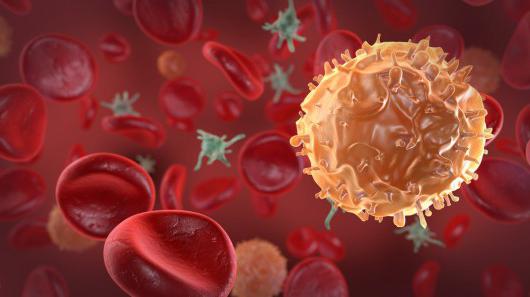
Receptor complexes of erythrocytes
The function of the membrane is to ensure the deformability of the red blood cell, which is necessary for capillary passage. At the same time, the structure of human red blood cells provides additional capabilities - cellular interaction and electrolyte current. Proteins with carbohydrate residues are receptor molecules, thanks to which red blood cells are not “hunted” by CD8 leukocytes and macrophages of the immune system.
Red blood cells exist thanks to receptors and are not destroyed by their own immunity. And when, due to repeated pushing through the capillaries or due to mechanical damage, red blood cells lose some receptors, spleen macrophages “extract” them from the bloodstream and destroy them.
Normal in blood
It should be understood that the total number of red blood cells in women or men by age and the norm in the circulatory system are not the same thing.
The total number includes three types of red blood cells:
- those still developing in the bone marrow;
- those that will soon leave the bone marrow;
- those that already travel through the blood system.
Red blood cells in the blood of women are contained in smaller quantities, which is due to the loss of a certain amount of blood during the menstrual cycle. The normal content of red blood cells in the blood of women is 3.9–4.9 × 10^12/l.
The normal rate of red blood cells in men is 4.5–5×10^12/l. Higher rates are due to the production of male sex hormones, which produce their synthesis.
In children, red cells should normally be contained in the following quantities:
- in newborns - 4.3-7.6 × 10^12/l;
- in a two-month-old baby - 2.7–4.9 × 10^12/l;
- by year - 3.6–4.9×10^12/l;
- in the period from 6 to 12 years - 4–.5.2 × 10^12/l.
During adolescence, red blood cell counts are compared with adult norms. More specific figures by age will be provided by a table that can be found on the Internet.
Internal structure of a red blood cell
What is an erythrocyte? Its structure is no less interesting than its functions. This cell is similar to a bag of hemoglobin, bounded by a membrane on which receptors are expressed: clusters of differentiation and various blood groups (Landsteiner, Rhesus, Duffy and others). But inside the cell is special and very different from other cells in the body.
The differences are as follows: red blood cells in women and men do not contain a nucleus, they do not have ribosomes and the endoplasmic reticulum. All these organelles were removed after the cell cytoplasm was filled with hemoglobin. Then the organelles turned out to be unnecessary, because pushing them through the capillaries required a cell with minimal dimensions. Therefore, inside it contains only hemoglobin and some auxiliary proteins. Their role has not yet been clarified. But due to the absence of the endoplasmic reticulum, ribosomes and nucleus, it has become light and compact, and most importantly, can be easily deformed along with the fluid membrane. And these are the most important structural features of red blood cells.
Red blood cell life cycle
The main features of red blood cells are their short life. They cannot divide and synthesize protein because the nucleus has been removed from the cell, and therefore structural damage to their cells accumulates. As a result, erythrocytes tend to age. However, the hemoglobin that is captured by splenic macrophages during red blood cell death will always be sent to form new oxygen carriers.
The life cycle of a red blood cell begins in the bone marrow. This organ is present in the lamellar substance: in the sternum, in the wings of the ilium, in the bones of the base of the skull, and also in the cavity of the femur. Here, from a blood stem cell, under the influence of cytokines, a precursor of myelopoiesis with a code (CFU-HEMM) is formed. After division, it will give the ancestor of hematopoiesis, designated by the code (BOE-E). From it, a precursor of erythropoiesis is formed, which is designated by the code (CFU-E).
This same cell is called the colony-forming cell of the red blood sprout. It is sensitive to erythropoietin, a hormonal substance secreted by the kidneys. Increasing the amount of erythropoietin (according to the principle of positive feedback in functional systems) accelerates the processes of division and production of red blood cells.
Red blood cell count
A red blood cell count is a blood test that is used to determine the number of red cells in the blood. The test is important because blood cells contain hemoglobin, which carries oxygen to body tissues. Their magnitude influences how much oxygen tissues receive in order to function. If the amount is too high or low, symptoms and complications may occur.
Low red blood cell count, symptoms may include:
- fatigue;
- shortness of breath;
- dizziness, weakness;
- increased heart rate;
- headache;
- pale skin.
High level of red blood cells, the following symptoms may occur:
- joint pain;
- itchy skin, especially after a shower or bath;
- sleep disturbance.
This is interesting! When blood is centrifuged to force the cells to settle, the volume of red blood cells is 42 to 54% of the total volume in men and 37 to 47% in women. The values are slightly lower in children.
Basic functions of red blood cells
Red blood cells play an important role in hemostasis and thrombosis, both of which mean blood clotting and can act as a procoagulant. This means that it helps in converting inactive prothrombin into the active enzyme thrombin, which is necessary for blood clotting.
The main functions of red blood cells are:
- In the transport of oxygen from the lungs to the body's tissues and carbon dioxide as waste, from the tissues and back to the lungs.
- Red cells are also the second largest contributor after sodium to blood osmolarity, which is important for fluid balance in the body.
- A deficiency of red blood cells can cause swelling because the blood is then unable to absorb the usual amount of water from the tissues around the capillaries.
Life cycle of red blood cells
The production of red blood cells in the bone marrow occurs at a staggering rate of over 2 million cells per second. In order for this production to occur, the amount of raw materials must be present in sufficient quantities. These include nutrients necessary for the maintenance of any cell, such as glucose, lipids and amino acids.
However, the production of red blood cells also requires several micronutrients:
- Iron. Each heme group in a hemoglobin molecule contains an ion of the trace element iron. On average, less than 20 percent of the iron consumed is absorbed. Heme iron from animal foods, such as meat, poultry and fish, is absorbed more efficiently than from plant foods. The bone marrow, liver and spleen can accumulate iron in the protein compounds ferritin and hemosiderin. Ferroportin transports iron across the plasma membranes of intestinal cells and from its storage sites into tissue fluid, where it enters the blood.
- Copper. The trace element is a component of two plasma proteins, hepestin and ceruloplasmin. Without them, hemoglobin cannot be adequately produced. Located in the intestinal villi, hephaestin allows iron to be absorbed by intestinal cells. In a state of copper deficiency, the transport of iron for heme synthesis is reduced, ultimately leading to organ damage.
- Zinc. It functions as a coenzyme that facilitates the synthesis of the heme portion of hemoglobin.
- B vitamins. They facilitate DNA synthesis. They are important for the synthesis of new cells, including red blood cells.
On a note! Red blood cells live up to 120 days in the circulation, then worn-out cells are removed by a type of myeloid phagocytic cell called macrophages. They are located mainly inside the bone marrow, liver and spleen.
Functions of hemoglobin and its compounds

Hemoglobin is a respiratory pigment that binds to oxygen or carbon dioxide. This allows oxygen to be delivered throughout the body to tissues and organs and carbon dioxide to be removed. Hemoglobin is mainly composed of iron, which, when combined with oxygen, gives blood its red color. In the arterial circulation, hemoglobin has a high affinity for oxygen and a low affinity for carbon dioxide, organic phosphates, as well as hydrogen and chlorine ions.
When red blood cells die, hemoglobin is broken down: the iron is transferred to the bone marrow by proteins called transferrins and used again in the production of new blood cells. Most hemoglobin forms the basis of bilirubin, a chemical that is excreted in bile and gives feces its characteristic yellow-brown color.
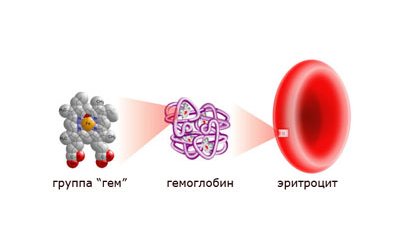
Hemoglobin compounds
One hemoglobin molecule contains 4 heme groups, each of which contains one iron atom. Heme, which makes up only 4 percent of the molecule's mass, is composed of a ring-shaped organic compound known as a porphyrin with an iron atom attached to it. It binds oxygen as blood moves between the lungs and tissues. Each hemoglobin molecule contains four iron atoms, which, accordingly, can connect four oxygen atoms. The next part of the hemoglobin molecule is organic, containing several protein chains.
Destruction of red blood cells
For approximately 100-125 days, the cell circulates in the blood, constantly carries oxygen and removes metabolic products from tissues. It transports carbon dioxide bound to hemoglobin and sends it back to the lungs, simultaneously filling its protein molecules with oxygen. And as it gets damaged, it loses phosphatidylserine molecules and receptor molecules. Because of this, the red blood cell comes under the macrophage’s sights and is destroyed by it. And the heme obtained from all the digested hemoglobin is again sent for the synthesis of new red blood cells.