What is the essence of the study
The method is based on the effect of X-rays on the tissues of the human body, subsequent analysis and registration of the degree of radiation absorption by anatomical structures.
The object under study is placed in the diagnostic zone, which is represented by a gantry frame. An X-ray tube and a system of sensors arranged in several rows are built inside the frame.
When scanning starts, the tube rotates at a given speed in the axial plane around the patient and generates radiation in the form of a thin beam.
The beam, when passing through the body, is absorbed by tissues to varying degrees. Blocks of sensors located on the opposite side capture signals, record the difference in the degree of absorption of X-rays and transmit information to a computer data processing station.
On a computer, the doctor studies from 500 to 2000 layer-by-layer sections, reconstructs images using programs, and creates three-dimensional three-dimensional models of organs.
SCT of the spinal column
During spiral scanning, the source of ionizing radiation continuously rotates around the part of the spinal column being examined.
The table with the patient is also continuously immersed inside the diagnostic frame with a “tube-detector” system. With such synchronous movement without time delays, the X-ray beam takes on the shape of a spiral.
Layer-by-layer images obtained during the study are viewed separately and three-dimensional models of the changed areas of the spine are created.
SCT of the spine is informative for visualizing traumatic injuries: fractures of vertebral bodies, arches, articular processes, displacement of fragments into the lumen of the spinal canal.
Multidetector CT of the spinal column
MSCT of the spine is performed in a similar way to spiral CT. The difference is the large number of receiver units that receive the X-ray signal.
As a result, the speed of examination increases, the thickness of sections decreases to 0.5 mm. During one inhalation phase, a complete scan of the entire body is performed.
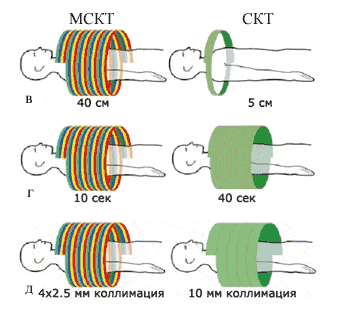
MSCT scans an object with 4-helices in one revolution of the tube, while the rotation speed is 0.5 seconds faster than the MSCT.
Multislice CT diagnoses painful changes in bone structures, intervertebral discs, spinal cord, spinal canal, and soft tissues.
What do the photographs reveal?
The tomograms obtained during the scan determine the condition and integrity of the spinal column, vertebrae, discs, medulla, central spinal canal and soft tissues. The location, extent and nature of the identified changes are determined.
CT scan of the cervical spine
When examining the spinal column at the cervical level, the shape and diameter of the spinal canal, the condition of the brain and vertebrae, the exit of the nerve roots, and the position of the uncinate processes are determined.
Stage 3 spondylosis deformans, common osteochondrosis
The most commonly detected pathology in the cervical spine:
- non-discogenic spinal stenosis;
- paramedian herniated intervertebral discs;
- osteochondrosis;
- protrusion, extrusion of discs;
- hypertrophy of uncovertebral joints;
- injuries.
CT scan of the chest
Examination of the thoracic spine shows inflammatory processes, destruction and fracture of vertebral bodies, damage to the medulla, ligament ruptures, and space-occupying formations.

Dorsal protrusion of intervertebral discs Stage 3 spondylosis deformans, widespread osteochondrosis
Tomography of the thoracic spine reveals:
- compression, explosion fractures of vertebral bodies;
- intervertebral hernia;
- spondylitis;
- spondylosis, osteochondrosis;
- curvature;
- tumor damage to the brain matter and membranes;
- cysts.
CT scan of the lumbosacral segment
A CT scan of the spine at the level of the lumbar vertebrae provides information about the condition of the joints, discs, central canal, nerve roots, paravertebral ligaments, and muscles.
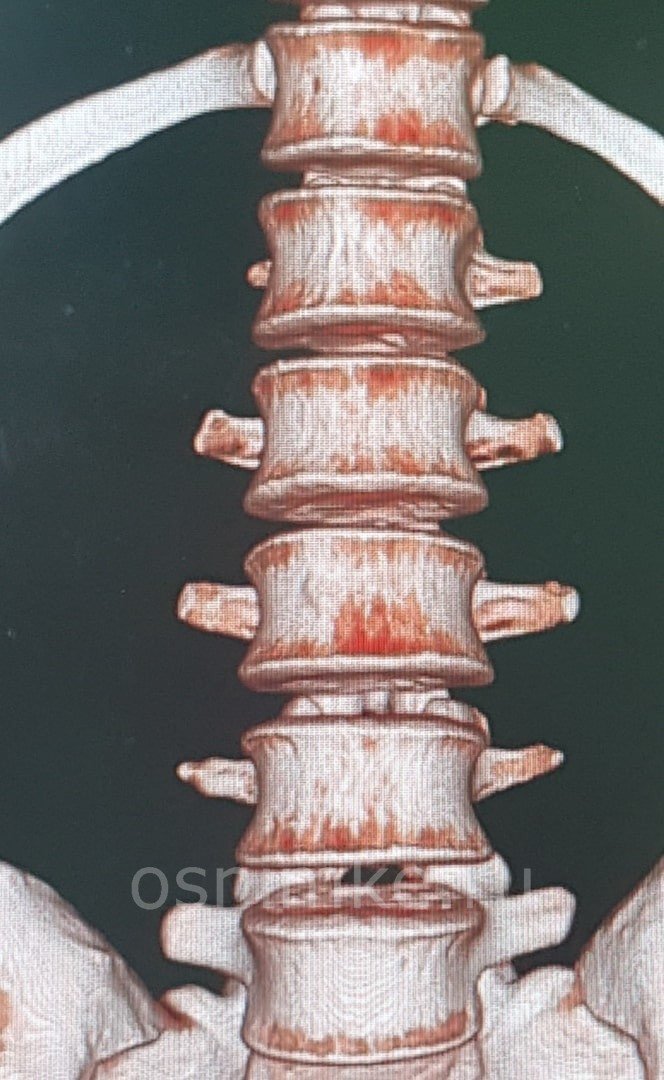
3D reconstruction of the lumbar region, normal
Tomography of the lumbosacral region determines:
- the presence of fractures, cracks of the vertebrae;
- tumor and metastatic lesions;
- hernias;
- spinal canal stenosis;
- degenerative-dystrophic processes;
- damage to the vertebrae in systemic diseases.
Indications
A CT scan of the spine is performed for:
- To study the vertebrae.
- Detection of problems with the spine, such as tumors, fractures, deformities, infection, or narrowing of the spinal canal (spinal stenosis).
- Detection of intervertebral disc herniation.
- Detection of compression fractures associated with osteoporosis.
- Identification of congenital problems with the spine.
- Study of problems identified by radiography.
- Monitoring the effectiveness of spinal surgery.
Indications and prohibitions on the use of CT
Tomography is used to diagnose conditions that require an accurate diagnosis when other instrumental research methods are not informative:
- mechanical damage to the spine and surrounding tissues;
- benign neoplasms: hemangioma, osteoma, osteoblastoclastoma, osteochondroma;
- malignant tumors and metastases: myeloma, Ewing's sarcoma, osteosarcoma, chondrosarcoma;
- inflammatory diseases of the spine of a specific and nonspecific nature: tuberculous spondylitis, osteomyelitis, ankylosing spondylitis;
- inflammatory processes in the spinal cord: purulent epiduritis, myelitis;
- systemic metabolic diseases - osteoporosis;
- developmental anomalies: atlas assimilation, Kimmerly anomaly;
- degenerative-dystrophic processes: hernia, degradation of the ligamentous apparatus, vertebral tissue;
- back pain of unknown origin;
- before preparing for reconstruction operations, monitoring the dynamics of conservative treatment.
CT scanning is not prescribed for pregnant women and children under 14 years of age due to the harmful effects of X-ray radiation on the fetus and growing body.
In emergency cases, this category of people undergoes examination under the protection of special screens. To reduce radiation exposure, reduce the duration of the procedure.
Contrast-enhanced CT scans are performed with caution in patients with diabetes mellitus, hyperthyroidism, and renal failure.
For obese people, devices are selected whose maximum load capacity corresponds to the patient’s body weight.
What is MRI of the spine?
Magnetic resonance imaging is a highly accurate and informative diagnostic method based on the use of modern technologies, and with its help you can examine almost any part of the body, for example, the brain or the spine, on which you will focus special attention. Examination of the spine using the resonance diagnostic method involves the use of a strong magnet that creates a magnetic field, which allows images to be taken
In medicine, MRI of the spine is used incredibly often, since such exposure does not affect health. This is because magnetic resonance imaging is not based on X-rays, but on nuclear magnetic resonance.
It is also worth noting that MRI examination of the spine belongs to the list of procedures performed by a non-invasive method, and its use is necessary for choosing a treatment method for various injuries, as well as diseases of the spine. In addition to the magnetic field, the body is also affected by high-frequency radio waves.
This procedure produces precise images of the spine through computer processing. Thus, after using computer processing, it is possible to obtain clear images that can be studied either directly on the monitor or after they are printed on a special film. Using this method, you can thoroughly study the condition of the vertebrae, as well as determine their shape. MRI also allows specialists to study the spinal cord, or more precisely, its condition, the same can be said about the nerve endings. Here are the main advantages of MRI:
- completely non-invasive, that is, the procedure does not involve any effects on the skin;
- absence of dangerous x-ray radiation;
- the ability to obtain incredibly high-quality and informative images that help make a diagnosis, as well as identify a lot of disorders, which we will talk about a little later;
- the possibility of a complete examination, and specialists are able to identify even pathologies that may be hidden due to bones on x-rays;
- the ability to detect even small changes that may indicate the development of tumors;
- MRI allows specialists to evaluate the effectiveness of various treatment methods, as well as identify possible complications.
Often people who are far from medicine ask the question of which is better: MRI or CT. The fact is that it is impossible to answer it unequivocally, since these procedures are suitable for examining various parts of the body. Computed tomography, like X-rays, helps to easily assess the condition of bone tissue, when (due to the low water content in them) MRI does not have this ability, but it allows you to obtain detailed information about many other things, let's look at the main ailments that can be identified using this diagnostic method.
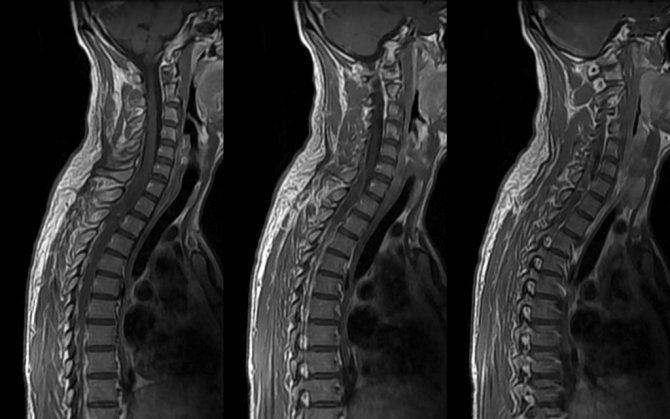
MRI of the spine is a study of the spinal column and surrounding tissues using an electromagnetic field.
How to prepare patients for diagnosis
Examination of the spinal column and surrounding tissues in emergency cases and on a routine basis does not require lengthy preparation or adherence to special diets.
When using contrast enhancement, sedatives and narcotics, abstinence from food and liquids for 4-6 hours is required to prevent aspiration complications.
An allergy test is performed 20-30 minutes before the procedure to determine hypersensitivity to the contrast agent.
If there is a history of allergic reactions to iodine drugs, premedication with methylprednisolone and diphenhydramine is performed.
3-7 days before scanning with contrast, or on the day of the study, venous blood is taken to determine the level of creatinine.
Patients with diabetes mellitus and reduced renal function (GFR less than 50 ml/min) should not take metformin before the procedure.
To prevent the development of lactic acidosis, the drug is resumed two days after a control study of the functional abilities of the kidneys.
Risks
The likelihood of problems occurring with a CT scan is low.
- There is a possibility of an allergic reaction to the contrast agent.
- If the patient is breastfeeding, then in order to prevent the contrast from getting into the baby’s milk, it is recommended to express the milk in advance and not put the baby to the breast for two days after the procedure.
- If the patient has diabetes or is taking metformin, the contrast may cause problems. You should stop taking metformin before the procedure and continue taking it some time after the procedure.
- The patient may experience nausea or vomiting after the test.
- There is a small chance of infection where the needle was inserted or bleeding in the area around the spine.
- An injection into the space around the spinal cord may cause headaches. In rare cases, seizures may occur after contrast material is injected.
- There is a small chance of getting cancer with some types of CT scans.
Scanning procedure
Before diagnosis, the patient or his legal representative signs informed consent for the study.

The doctor conducts an introductory conversation with the patient, explains in general terms the procedure and rules of conduct. The laboratory assistant helps the patient change clothes and remove removable metal elements from the area being examined.
The patient lies down on the tomograph table in a supine position. The upper limbs are raised up and behind the head. A cervical headrest is placed under the neck, and a bolster is placed under the knees to straighten the lumbar lordosis.
A catheter is inserted into the cubital vein to administer contrast. For automated drug delivery, synchronous with scanning, an injector with a flask is attached to the catheter.
The patient is placed on a couch inside the gantry frame. The laboratory assistant places a light beam in the projection of the area under study and, at the doctor’s signal, leaves the room with the tomograph.
The scanning time for a CT scan of the back, during which all anatomical structures are completely captured, is 10-20 minutes.
Upon completion of the diagnosis, the transport table returns to its original position, the patient is placed in a special room for observation for 40-60 minutes.
Computed tomography of the spine: highlights
Benefits of CT scan of the spine
- high information content and accuracy of the study;
- painlessness of the procedure;
- lack of rehabilitation period;
- minimum contraindications to scanning;
- efficiency of research;
- insignificant radiation exposure to the patient;
- the ability to study both bone structures and soft tissues;
Indications for computed tomography of the spine
- spinal injuries: bruises, fractures, deformations, cracks;
- intervertebral disc herniation;
- tumors of various tissue origin;
- osteochondrosis;
- abscesses;
- congenital anomalies;
- pain in the back and lower back of unknown etiology;
- preoperative preparation.
Contraindications to CT scan of the spine
- pregnancy at any stage;
- severe, shock conditions;
- hyperkinesis, mental disorders;
- individual intolerance to the components of the contrast agent;
- renal failure;
- diabetes.
Alternative Methods
- MRI;
- X-ray;
How is a CT scan of the spine performed?
The CT scan procedure is absolutely painless. Unlike MRI, computed tomography is performed quickly, within a few minutes.
During the procedure, the patient is given a contrast agent (if necessary). Immediately after this, a person may feel a metallic taste in the mouth, a surge of warmth, and mild nausea - these sensations are normal and, as a rule, pass after some time.
10-20 minutes after the contrast is administered, the patient lies down on the tomograph table, then the scanning procedure begins. During operation, the device produces a uniform, not very intense noise.
Before the procedure begins, the doctor leaves the CT room and watches the scan through a special glass from the next room. Communication is carried out via intercom. If a child is being examined, the presence of one of the parents is allowed.
Preparing for a CT scan of the spine
No special preparation is required for scanning.
Time for CT scan of the spine
1-5 minutes, with contrast - 20 minutes.
Use of contrast during the procedure
In some situations, at the discretion of the doctor, a CT scan of the spine is performed with a contrast agent, which is administered intravenously immediately before the procedure for better visualization. The contrast agent spreads through the bloodstream throughout the body and accumulates in the tissues, highlighting them in the image.
The use of contrast helps to diagnose vascular diseases and identify malignant neoplasms at the earliest stages.
The use of contrast in the absence of contraindications is absolutely harmless. The substance is completely eliminated from the body within two days. After the procedure, it is recommended to drink more fluid to speed up the process of removing the contrast.
Doctor's report
You can receive a doctor's opinion 1-2 hours after the procedure. To do this, it is not necessary to go to the medical center again - the results of the study can be downloaded in your personal account on our website.
Further treatment is prescribed by a doctor - surgeon, neurologist, therapist or traumatologist. If you wish, we will arrange an appointment with a specialist in any clinic of your choice.
To study The structure of the spine: lumbar region
CT with iodine contrast agents
Contrast agents introduced into the vascular bed are absorbed by normal and pathologically altered tissues to varying degrees.
When scanning with iodine contrast enhancement, the visibility and differentiation of anatomical formations improves, and foci of neovascularization are visualized.
Contrast is not used to diagnose bone structures, since bone tissue has a natural high contrast and is well visualized on images.
Drugs are administered manually or through an automatic contrast supply system. The dose is calculated individually.
Per 1 kg of patient weight, 1 ml of contrast containing 300 mg of iodine is injected. The drug is excreted from the body unchanged within 24 hours.
To speed up the elimination of iodine, it is recommended to drink plenty of fluids in a volume of at least 2-3 liters within 24 hours after diagnosis.
If multiple injuries to the vertebrae and spinal cord are suspected due to polytrauma, contrast is injected into the spinal canal through a puncture.
The method makes it possible to determine the patency of the cerebrospinal fluid pathways, the level and extent of compression of the brain by displaced fragments.
CT diagnostics of tumors of the spine and spinal cord
Spinal cord neoplasms are relatively rare and account for about 2% of all tumors. Traditionally, tumors of the spine and spinal cord are divided into 3 groups:
- Intramedullary – ependymomas, astrocytomas, hemangioblastomas;
- Extramedullary-intradural – meningiomas, neuromas, subarachnoid metastases, embryogenetic neoplasms (dermoids, lipomas, teratomas, epidermoids);
- Extradural – primary (tumors of the spine), secondary (metastatic neoplasms, tumors that grow into the spinal canal).
Ependymomas are benign, slow-growing tumors but have an abundant blood supply. This leads to the development of intratumoral and subarachnoid hemorrhages. In 45% of cases, ependymomas contain cysts. They grow slowly, resulting in radiographically visible bone changes. Non-contrast computed tomography of the spine does not provide the necessary information, since tumor tissue is difficult to distinguish from the spinal cord. With intravenous enhancement, the contrast agent accumulates in the tumor in a variable manner. CT myelography is more informative in diagnosing ependymomas.
T1-weighted magnetic resonance imaging clearly shows thickening of the spinal cord. When the tumor is located at the level of the roots of the cauda equina, radiologists reveal a typical solid structure and the same intensity as the brain in this mode. On T2-weighted images, the appearance of ependymoma is not specific; its solid part has an extremely intense signal, which, however, is less pronounced compared to the cystic or necrotic components. With intravenous amplification, a rapid and fairly uniform increase in signal intensity from the tumor tissue is observed.
The capabilities of computed tomography in the diagnosis of astrocytomas are limited. On tomograms, segmental expansion of the spinal canal can be observed, but bone changes are not typical for astrocytomas. On a CT image, the neoplasm has a heterogeneous structure. After intravenous injection of contrast agent, a heterogeneous increase in the density of tumor tissue is observed. Using computed tomographic myelography, the presence of a spinal cord tumor is often detected by the characteristic thickening of the latter.
Hemangioblastomas are diagnosed using contrast-enhanced CT. In the pictures you can see a tumor node in which the contrast agent intensively accumulates. Neoplasms of the spinal nerve roots, neurofibromas and neuromas, are more often detected when performing computed tomography of the cervical and thoracic spine. In most cases, the tumor is encapsulated and well demarcated, sometimes contains a cystic component and is associated with neurofibromatosis. A CT scan of the spine provides more information about the tumor than an X-ray examination.
Meningioma is a benign, slow-growing tumor. Most often, meningiomas are localized in the thoracic spine. Most of them are elongated and can be located on any surface of the spinal canal. Contrast-enhanced CT scan of the thoracic spine reveals a tumor of increased density and demonstrates secondary bony hyperostosis and calcifications at the base of the meningioma.
Osteochondroma is one of the most common bone tumors. It is localized in the spine in 3-7% of cases. On plain radiographs, the tumor appears as a broad-based or pedunculated mass with a cortical layer that extends into a compact part of the surrounding bone. Computed tomography of the spine more accurately determines the extent of the tumor, the presence of a cartilaginous border and its concomitant effect on the spinal canal. If a patient has osteoma, a CT scan of the spine reveals an area of decreased density that is small in size and round in shape, with or without calcified areas.
Metastatic tumors are predominantly localized in the thoracic spine. Computed tomography is used to identify the volume and extent of osteolytic lesions of vertebral elements, the presence of destruction of the cortical surface and the spread of the process through the epidural space or into the paravertebral tissues. After intravenous contrast, the density of the metastasis, according to computed tomography of the spine, increases. This helps radiology doctors better assess the extent of tumor growth into the paravertebral tissue and epidural tissue.

MRI or CT scan of the spine
The information content of CT in examining the spine is 95-97% and is second only to MRI in diagnosing soft tissues and the medulla of the spinal canal. An alternative research method is radiography. We will consider a comparison of these two methods when examining the spine in this article.
Considering the high reliability of CT, the method is successfully used for making a final diagnosis, planning operations and conservative treatment.
The availability and speed of diagnosis makes tomography the method of choice for identifying diseases affecting the bone structures of the spine.