How it works?
The function of organs and tissues is assessed by the metabolism in them. The most universal (but not the only) “fuel” for cells is glucose. During a PET scan, the patient is injected with a small amount of glucose (less commonly, other substances) labeled with a radioactive atom, such as fluorine-18. It is accumulated by tissues with the maximum level of metabolism, which is characteristic of malignant neoplasms.
In the nucleus of a radioactive fluorine atom, beta decay occurs: one of the protons turns into a neutron, emitting an antimatter particle - a positron. In the path of positrons there are electrons - particles of matter. In a collision, an electron and a positron are mutually destroyed. Their mass is converted into energy according to Einstein's famous formula E=mc2, and this energy leaves the tissue in the form of gamma rays. At this moment, the body becomes a source of weak radiation, with tumors that have accumulated more of the drug emitting the most actively. Their gamma radiation is recorded by a device that assesses where the tumor and metastases are located and what their size is.
The problem is that all other tissues will remain practically not “highlighted”, which is why it is impossible to say exactly where they are located with sufficient clarity only based on the PET results.
To do this, CT is performed simultaneously with PET, which visualizes the structure of tissues with millimeter precision, but does not say anything about their functions. Sometimes contrast agents are used in CT scans. After the scan, the PET and CT results are sent to a computer, which superimposes them on top of each other in a three-dimensional image and gives the doctor accurate information about where the changed cells are located.
How positrons unmask a tumor. The principle of positron emission tomography.
The tumor absorbs the drug with a radioactive isotope.
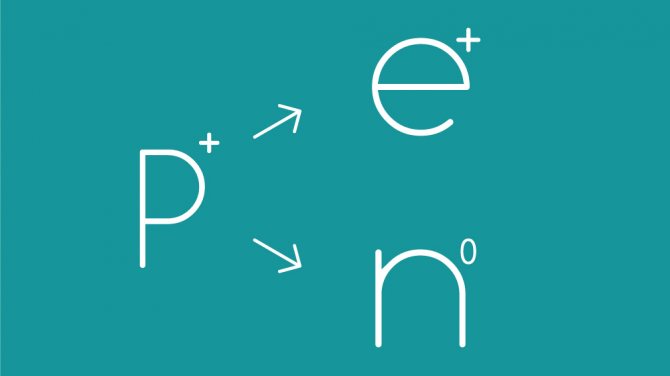
The proton p+ in the nucleus of an atom of a radioactive element turns into a neutron n0, emitting a positron e+.
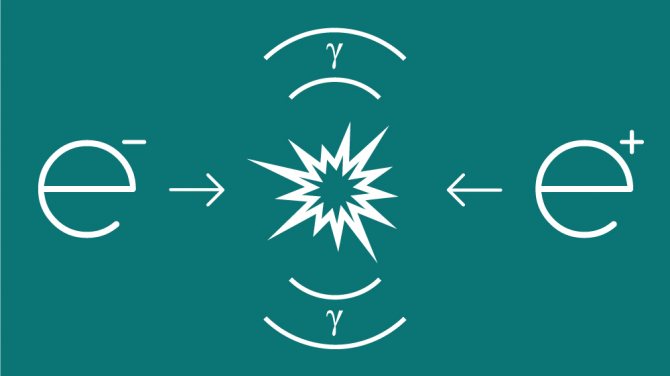
A positron e+ collides with an electron e-, and both particles annihilate, turning into a stream of gamma radiation.

The device detects gamma radiation emitted by the tumor.
Graphics: Roman Vyshnikov.
Visualization, normal isotope distribution and scanning artifacts
Isotope attenuation is a major problem in PET, since the totality of the paths of both 511 keV photons must, by definition, “cover” the entire width of the patient's body. However, this problem is well solved with the help of correction algorithms - programs that are built into the scanning protocol. With the advent of PET/CT systems, it is likely that even more refined correction algorithms will appear. Artifacts in PET arise due to the fact that the human body is not a sphere, but an ellipse, so errors are possible. Artifacts may be caused by the following:
- Patient movement during the examination
- Contamination from the injection site
- Previous radionuclide study (shortly before PET)
- Attenuation of radiation and geometric distortions
- Interference and errors (poorly developed statistical research methodology)
- Muscle artifacts of 18-FDG distribution
Some patients who are stressed or nervous during the test may experience abnormal uptake of 18-FDG into muscle tissue. The usual localization of such a grip is the muscle groups of the neck, shoulder girdle and upper extremities. Artifacts due to patient movement, contamination from the injection site, and previous radionuclide studies can be minimized by simple techniques (eg, wrapping the patient, teaching the patient before the test, grooming). Dr. Barry Siegel from the Mallinckrodt Institute of Radiology, St. Louis, USA, noted that artifacts due to geometric distortions, statistical errors and radiation attenuation can be somewhat reduced by multiple repeated image reconstructions (as opposed to the old methods of reconstructing images from their projections ), resulting in data that can be better “tailored” to individual patient characteristics.
Normal 18-FDG uptake occurs largely in the brain and bladder and, to a lesser extent, in the liver, bone marrow, and kidneys. The uptake of the isotope by the myocardium may be heterogeneous, which depends on the patient’s physique and concomitant coronary pathology. To reduce the uptake of the isotope by the myocardium, the patient should not eat during the night before the morning study, or eat only a light breakfast if the study is scheduled for the second half of the day. Dr. Mark W. Groch from Northwestern University USA showed that monitoring of blood glucose levels is necessary before administering 18-FDG, the target level is 15 mmol/l. Patients with a glucose level of more than 20 mmol/l are not examined, and those who have a glucose level in the range of 15-20 mmol/l are examined only after consultation with specialists.
Why is such precision needed?
It is necessary for carrying out any type of antitumor therapy. Using PET-CT, the surgeon will know exactly where the boundaries of the tumor and its metastases are, which will allow them to be completely removed without affecting healthy organs (unless, of course, the tumor has grown into vital structures). The radiologist will be able to figure out exactly where to focus the radiation to kill cancer cells while causing minimal damage to normal tissue. Using a repeat PET-CT scan, you can evaluate how effectively radiation and chemotherapy stop the growth and spread of cancer and, if necessary, adjust treatment tactics.
But it is necessary to inject radioactive substances - is this dangerous?
Any studies using ionizing radiation, including the usual x-ray and fluorogram, are associated with a certain risk. The main thing is to ensure that it is insignificant. To do this, when conducting PET, substances are used that are eliminated from the body as quickly as possible - within a few hours - and do not have time to cause harm. Due to this, the radiation exposure to the body from PET is even less than from X-ray radiation from CT.
Modern diagnostic technologies are created and approved for use only on the condition that the benefit from them obviously outweighs the risk to the patient. PET-CT in this case is no exception.
How to get a quota for PET CT
Quota – the right to receive a free service. According to No. 326-FZ dated November 29, 2010 “On compulsory health insurance in the Russian Federation” and the new list of free services in the direction of February 29, 2016, every holder of a compulsory medical insurance policy in the Russian Federation has the right to undergo a PET CT examination for free. Relevant for cancer patients and patients with hematological diseases. An unlimited number of quotas can be issued to one patient. That is, PET CT can be performed free of charge during the entire period of treatment for certain diseases.
The only downside to the quota is a queue of patients and long waits, sometimes for weeks.
To obtain a quota, a referral from the attending physician certified by the chief physician of the medical institution is required.
How to prepare for the examination?
Several hours before the PET-CT scan, you should not eat food, drinks (except water) or exercise - this may affect the results. Before the examination, it is necessary to remove all metal objects (watches, jewelry, glasses, dentures, etc.); it is better to leave them at home, except for the most necessary ones.
It is also necessary to tell your doctor about your existing diseases and all medications and dietary supplements you are taking. Women should be sure to report even the slightest possibility of pregnancy. Depending on your condition, your doctor may give you individual instructions to follow.

Side effects of positron emission tomography
The state of health after PET/CT is not disturbed or disturbed, however, with some diseases it is difficult for the patient to remain motionless for a long time. The most common side effects of the diagnosis are weakness and dizziness due to dietary restrictions and the duration of the study. The administered medications are non-toxic, prepared under sterile conditions and meet the requirements of state standards. If you follow your doctor's recommendations, PET/CT has no negative consequences.
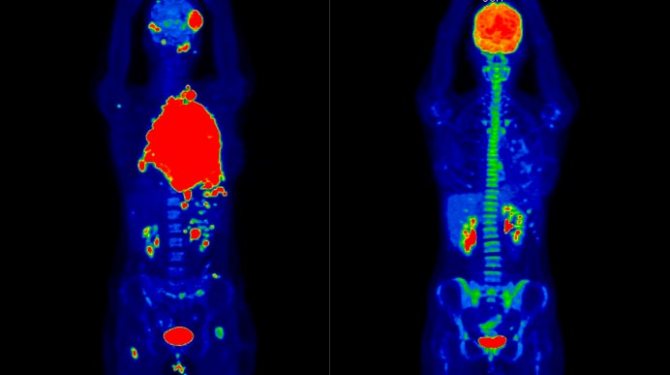
A 19-year-old female patient was diagnosed with diffuse large B-cell lymphoma. The image on the left is the results of a PET/CT study to assess the extent of the malignant process (red areas) before treatment, on the right are the results after two courses of chemotherapy.
Sources
- Romanò CL., Petrosillo N., Argento G., Sconfienza LM., Treglia G., Alavi A., Glaudemans AWJM., Gheysens O., Maes A., Lauri C., Palestro CJ., Signore A. The Role of Imaging Techniques to Define a Peri-Prosthetic Hip and Knee Joint Infection: Multidisciplinary Consensus Statements. // J Clin Med - 2021 - Vol9 - N8 - p.; PMID:32781651
- Lauri C., Iezzi R., Rossi M., Tinelli G., Sica S., Signore A., Posa A., Tanzilli A., Panzera C., Taurino M., Erba PA., Tshomba Y. Imaging Modalities for the Diagnosis of Vascular Graft Infections: A Consensus Paper among Different Specialists. // J Clin Med - 2020 - Vol9 - N5 - p.; PMID:32429584
- Heinzel A., Marienhagen J., Yekta-Michael SS., Mottaghy FM., Krzemien J., Lemos M. Pilot study of a newly developed eLearning tool to teach CT and PET/CT in radiology and nuclear medicine. // Nuklearmedizin - 2021 - Vol59 - N2 - p.79-84; PMID:32268393
- Schütz UHW. . // Orthopade - 2021 - Vol48 - N1 - p.5-43; PMID:30656385
- Tsukazan MTR., Terra RM., Detterbeck F., Santoro IL., Hochhegger B., Meirelles GSP., Fortunato G., Prado GF. Management of lung nodules in Brazil-assessment of realities, beliefs and attitudes: a study by the Brazilian Society of Thoracic Surgery (SBCT), the Brazilian Thoracic Society (SBPT) and the Brazilian College of Radiology (CBR). // J Thorac Dis - 2021 - Vol10 - N5 - p.2849-2856; PMID:29997949
- Müller von der Grün J., Bon D., Rödel C., Balermpas P. Patterns of care analysis for head & neck cancer of unknown primary site: a survey inside the German society of radiation oncology (DEGRO). // Strahlenther Onkol - 2021 - Vol194 - N8 - p.750-758; PMID:29761228
- Vogel WV., Lam MG., Pameijer FA., van der Heide UA., van de Kamer JB., Philippens ME., van Vulpen M., Verheij M. Functional Imaging in Radiotherapy in the Netherlands: Availability and Impact on Clinical Practice . // Clin Oncol (R Coll Radiol) - 2021 - Vol28 - N12 - p.e206-e215; PMID:27692741
- Putora PM., Bedenne L., Budach W., Eisterer W., Van Der Gaast A., Jäger R., Van Lanschot JJ., Mariette C., Schnider A., Stahl M., Ruhstaller T. Oesophageal cancer: exploring controversies overview of experts' opinions of Austria, Germany, France, Netherlands and Switzerland. // Radiat Oncol - 2015 - Vol10 - NNULL - p.116; PMID:25994051
- Wang XY., Yang F., Jin C., Fu D.L. Utility of PET/CT in diagnosis, staging, assessment of resectability and metabolic response of pancreatic cancer. // World J Gastroenterol - 2014 - Vol20 - N42 - p.15580-9; PMID:25400441
- Sinkó D., Landherr L. . // Magy Onkol - 2012 - Vol56 - N4 - p.230-4; PMID:23236592