How does urobilinogen get into urine?
The destruction of red blood cells - erythrocytes - followed by the breakdown of hemoglobin protein leads to the formation of bilirubin. The pigment enters the bloodstream along with albumin as free (indirect) bilirubin. At the next stage, it is captured by hepatocytes (liver cells) and transformed into direct (bound) bilirubin. This water-soluble form enters the intestines along with bile.
There, bilirubin is converted to urobilinogen. Microorganisms inhabiting the intestinal lumen contribute to the entry of part of urobilinogen into the bloodstream. Much of it is again sent to the liver, bilirubin is formed. A small amount of urobilinogen from the blood enters the urine.
An abnormally high or too low content of urobilinogen in the urine means that a disorder has occurred associated with the patency of the biliary tract, liver activity has decreased, and the microbial balance inside the intestine has been disrupted.
Diseases with accelerated breakdown of red blood cells (hemolytic anemia, hemorrhagic diathesis, intestinal bleeding, large hematomas) can also cause an increase in the level of urobilinogen in a general urine test.
General information
As a result of the breakdown of hemoglobin in red blood cells, bilirubin is released, which is a very toxic component. By binding to glucuronic acid (this process occurs in the liver), bilirubin loses the ability to negatively affect the body. Together with bile, it enters the intestine, where it is fermented, oxidized, metabolized (breaks down), resulting in the appearance of urobilinogen.
The resulting bile pigment is partially sent through the bloodstream to the kidneys and excreted in the urine, giving it a characteristic yellow color. The remaining part of urobilinogen, when moving into the large intestine, is transformed into stercobilin and excreted in the feces, giving them a natural brown tint.
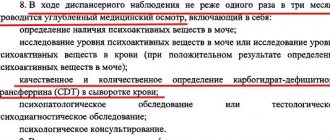
Normally, a small amount of urobilinogen is always present in the urine, although it may not be detected in the laboratory. The increase in concentration is due to:
- intensive breakdown of hemoglobin in erythrocytes and, as a consequence, the formation of large amounts of bilirubin;
- functional pathologies of the liver, for example, the inability to “process” bilirubin;
- various pathological processes in the intestines, as a result of which bilirubin metabolism is disrupted.
The absence of urobilinogen in the urine indicates that bilirubin does not enter the intestinal lumen. As a rule, a similar situation is observed with blockage of the bile ducts, fistulas, hepatitis, liver failure, destructuring of liver tissue, etc.
What analysis shows urobilinoids in urine
The level of urobilinogen is determined during a general clinical analysis (CCA). But you can suspect an increase or decrease in their number by visually assessing the color of the biological fluid. With a high content of urobilinoids, the color of urine changes - it becomes dark; with a low concentration of bile breakdown products, it becomes almost colorless.
Both phenomena should be a reason to see a doctor and undergo an examination. First you will have to pass the OAM. The result form will indicate the amount of urobilinogen (UBG, URO). Based on this, the doctor will prescribe further diagnostics or allay concerns regarding the patient’s health condition.
How to prepare and how the analysis is carried out
The urobilinogen test does not require preliminary preparation. The only thing doctors ask is that on the eve of urine collection, avoid foods that can change its color. These are beets, carrots, pumpkin. You should also not use medications (unless absolutely necessary) that give urine an unnatural color - analgin, acetylsalicylic acid, otherwise the analysis for urobilinogen will be biased.
To collect urine, prepare a disposable container purchased at a pharmacy or a well-washed dry jar with a volume of up to 200 ml with a lid. In the morning after sleep, you need to rinse the area of the external genitalia and dry it with a clean towel. Fill the container with 80-100 ml of urine.
The material is delivered for analysis no later than 2 hours after collection.
UBG in urine analysis: normal
The normal content of URO in urine for all age and gender categories of people should not exceed 34 mmol/l - this is an insignificant presence of pigment. Figures above the normative ones in the decoding of the analysis indicate diseases that directly or indirectly affect the transformation and excretion of bile pigments.
The absence of urobilinogen is also not considered normal. At least traces of it should be found in the urine.

Doctors advise expectant mothers to pay special attention to the color of urine. The appearance of a dark shade should alert you.
The norm for women during pregnancy does not exceed the usual. It ranges from 25-34 mmol/l urine.
In newborns, physiological jaundice, caused by the active breakdown of hemoglobin, is accompanied by a slight increase in the level of urobilinogen in the urine. As the jaundice disappears, urine values normalize. But in children in the first months of life, the intestines are not yet populated with a sufficient number of bacteria necessary to transport urobilinogen into the blood. Therefore, the urine of babies is almost colorless.
In men, women and children, insufficient fluid intake or rapid loss of fluid leads to dehydration. Urine becomes more concentrated, the content of urobilinogen increases.
Urobilinogen norms
Values not exceeding 34 mmol/l are considered normal.
Factors of influence
- In pregnant women, fluctuations in urobilinogen concentration are allowed throughout pregnancy. However, the appearance of “brown urine” is considered as a variant of liver pathology and requires consultation with a specialist;
- In newborns, an increase in the level of urobilinogen in the urine is observed in combination with physiological jaundice. The condition stabilizes after the symptoms disappear;
- In children 3-4 months of age, urobilinogen may be completely absent due to functional inferiority of the intestine. The introduction of complementary foods normalizes the intestinal microflora, as a result of which the concentration of urobilinogen in the urine returns to normal;
- With dehydration and/or insufficient fluid intake, the concentration of urine increases, along with which the level of urobilinogen also increases;
- Against the background of severe dysbacteriosis, beneficial bacteria that convert bilirubin into urobilinogen die, so the concentration of the latter in the urine decreases.
What does urobilinuria mean?
An increase in urine urobilinogen levels to 34-50 mmol/l and above is a sign of liver dysfunction. But it can also be caused by problems not related to the hepetobiliary system - severe heart pathologies, intestinal diseases. Sometimes urobilinuria is associated with non-pathological factors.
Exceeding the norm of urine urobilinogen on the analysis form is indicated by pluses:
- slight weakly positive (+);
- positive (++);
- significant excess (+++).
Physiological reasons
Increased urobilin in urine is found during fasting, after eating large amounts of fatty foods. Urobilinuria occurs due to dehydration. If you make timely adjustments to your diet and replenish fluid reserves, the composition of your urine will return to normal. This means that the increased urobilinogen will decrease.
Diseases of the liver and digestive tract
Most often, the reason that urobilinoids in the urine are elevated is due to too active synthesis or breakdown of bilirubin. In liver diseases, the mechanism for releasing bound pigment is disrupted in hepatocytes. Water-soluble bilirubin is released back into the blood and then leaves the body in urine. The problem arises with liver failure, hepatitis of autoimmune, viral, and alcoholic origin.
The detection of high levels of urobilinogen in urine is also associated with obstacles to the outflow of bile. The main causes of urobilinuria:
- benign and malignant tumors;
- cirrhosis of the liver;
- narrowing of the bile ducts, blockage with stones;
- blockage of the hepatic vein by a thrombus.

Changing the ratio of flora to the benefit of pathogenic microorganisms during dysbacteriosis reduces the flow of pigment into the bloodstream. The cause of the disorder can also be intestinal inflammation - enterocolitis (affects the thick section), ileitis (the disease affects the ileal segment).
Pregnancy
During pregnancy, the normative content of urobilinoids is the same as before conception. But pigment levels may increase slightly due to stress on the kidneys. The filtering organ does not cope with its function sufficiently; more urobilinogen enters the urine.
Disruption of the intestines, associated first with the restructuring of the hormonal system, and in the later stages with the pressure of the uterus on this part of the digestive tract, is accompanied by constipation in many pregnant women. Stagnation of feces causes the proliferation of putrefactive microflora, which impairs the absorption of urobilinogen. Then its increased amount is recorded during a urine test.
Toxicosis in the early stages can cause a jump in urine urobilinogen in a pregnant woman. Bouts of vomiting, increased kidney activity and the desire to urinate more often all lead to fluid loss.
Other reasons
High urobilinogen in the urine is found in people with infections - tuberculosis, scarlet fever. They cause disturbances in the pathology of the spleen, destruction of red blood cells after transfusion, and hemolytic anemia. Urinary urobilinogen may be increased due to the following reasons:
- heart failure, heart attack with subsequent deterioration of liver function;
- intoxication with synthetic chemicals, mushrooms, medications, alcohol, salts of heavy metals.
Urobilinogen in pregnant women and children
For expectant mothers, the same reference values are determined as for everyone else. A temporary increase in urobilinogen levels is allowed, which is associated with the growth of the uterus and an increase in the load on the kidneys and gastrointestinal tract.
Important!
In case of sudden darkening of urine, it is necessary to urgently take a test for urobilinogen to exclude liver pathologies or acute intoxication. The likelihood of developing diseases of the hepatobiliary system increases in women with a hereditary predisposition.
In most cases, the concentration of urobilinogen increases due to dehydration. At the same time, urine becomes denser and richer. Dehydration can be caused not only by insufficient fluid intake, but also by changes in the daily diet, taking dietary supplements and vitamins, as well as some other medications. Dehydration is also observed in the early stages of pregnancy (toxicosis of the first half). This condition is accompanied by a significant increase in urobilinogen in the urine (2-3 times).
In children, urobilinogen normally should not exceed 3.2 mmol/l. In case of increased concentration, differential diagnosis of the following diseases is carried out:
- cholelithiasis;
- hepatitis of various etiologies;
- physiological jaundice (destruction of specific hemoglobin and associated red blood cells);
- liver cirrhosis in acute or chronic form;
- dysbacteriosis (often observed in children of the younger age group);
- anemia (anemia, low blood hemoglobin);
- colitis and enterocolitis caused by pathogenic bacteria or helminths;
- poisoning with food, drugs, etc.
Possible reasons for the decrease in the indicator
Urobilinogen is not detected if the common bile duct is blocked. Bile does not enter the intestines and stagnates. URO in the analysis decreases, but the amount of bilirubin increases. Obstructive jaundice occurs. Then, along with the dark color of the urine, the skin and whites of the eyes will also acquire a yellowish tint.
The cause of obstruction of the outflow of bile is cholelithiasis, an oncological tumor affecting the head of the pancreas.
A decrease in the concentration of urine pigment is observed in some kidney pathologies associated with impaired ability of the organ to filter blood. Low urobilinogen content in urine is also caused by glomerulonephritis and neoplasms.
Treatment methods
In some cases, laboratory technicians indicate that there are traces of urobilinogen in the child’s urine. What this means should be explained in as much detail as possible by the attending physician. In certain situations, exceeding the norm may be associated with increased load on the kidneys, for example, if the patient has diarrhea.
Such cases are considered episodic and do not require any medical intervention, since the patient’s condition indicates normal kidney function, and not the progression of chronic diseases. If the results always show an increase in urobilinogen, then treatment is required.
Often, pediatric patients are prescribed to engage in physical therapy or gymnastics, and it is recommended to visit the pool. Thanks to this load, all unnecessary substances will be actively and independently eliminated from the body. A mandatory component of therapy is diet.
The child needs to balance the daily diet and make sure that plant and dairy foods predominate in it. Thanks to this, you can quickly restore the normal state of intestinal microflora. It is very useful to drink tincture of wormwood, tansy or immortelle.
As you can see, the process of determining the concentration of urobilinogen in urine, as well as the subsequent adjustment of indicators, is quite simple.
However, an experienced doctor should prescribe examination and treatment. Share:
How to reduce pigment content
If a high urobilinogen value is detected, the analysis must be repeated. If he confirms urobilinuria, then the therapist, gastroenterologist or hepatologist prescribes a diagnosis. She should identify the cause of high urobilin. Based on the examination, treatment is prescribed.
In therapy they use:
- hepatoprotectors – Esliver, Essentiale;
- antiviral for hepatitis - Arviron, Zepatir, Baraklyud, Leukinferon;
- choleretic agents – Odeston, Allohol, Flamin;
- vitamin and mineral complexes;
- immunomodulators.
Inflammatory processes affecting the intestines require antibiotic therapy. For dysbacteriosis, medications containing live lactobacilli are prescribed. To reduce the degree of poisoning, which resulted in an increase in the concentration of urobilinogen in the urine, sorbents (Sorbex, Enterosgel) are prescribed. They must be taken in parallel with increasing the volume of fluid you drink.

Absorption of urobilinogen occurs with the participation of bacteria inhabiting the intestines. Changing the ratio of flora to the benefit of pathogenic microorganisms during dysbacteriosis reduces the flow of pigment into the bloodstream.
To reduce the concentration of pigment, doctors recommend eating lean boiled meat, fresh fruits, vegetables, and cereals. Fermented milk products with a low fat content will help improve intestinal function.
Formation of matter
The human gastrointestinal tract has its own, unique microflora. Under the influence of beneficial organisms, bilirubin is transformed into urobilinogen, some of which is stercobilinogen. This component leaves the body during bowel movements.
Next, a mass with such a composition comes into contact with the blood. During the movement of biological fluid, it penetrates the liver. After it is filtered by the organ, the substance is converted back into bilirubin. The next stage of transformation is the interaction of the substance with bile, and finally its removal from the body.

The principle of formation and movement of matter in the body. Source: vashnevrolog.ru
In its pure form, this substance is considered quite dangerous, and neutralization involves the process of combining bilirubin with albumin (protein). Then this mixture enters the circulatory system and participates in various biochemical processes. And if a child has increased urobilinogen in the urine, it means that it was found to contain more than 4 mg per day.
An increase in the concentration of this substance can occur with the progression of certain pathologies, for example, toxic damage to the liver has occurred, there is hemolytic jaundice, or there are chronic diseases.
Traces of urobilinogen in a child’s urine occur when the gastrointestinal tract is disrupted, after food poisoning. A reduced level also indicates the formation of stones in the bile ducts, which impede the process of transporting bile to the intestines.