Syphilis is an infectious disease caused by a spirochete bacterium called Treponema pallidum. This pathology affects the mucous membranes, skin, internal organs, nervous system and human bones. The disease is primarily transmitted through sexual contact, but it can also be contracted through household means (dishes, personal hygiene items, etc.).
Important . Treponema pallidum is a fairly “gentle” bacterium; it dies within half an hour at a temperature of 48 degrees. Therefore, if there is a person with syphilis in the family, in order to avoid infection, his things should be regularly subjected to heat treatment.
Syphilis has several stages of development:
- The incubation period ranges from several days to several months (on average 3-4 weeks), during which time treponemes multiply and spread throughout the body through the blood and lymph; there are no external manifestations of the disease yet, but the patient is able to infect others.
- Primary syphilis – 1-2 months, a person’s lymph nodes enlarge, and in places where treponemas are introduced into the body (most often these are the external or external genitalia: the glans penis, the mucous membrane of the vagina and cervix, labia, less often - the oral cavity) small ulcers are formed - hard chancre.
- Secondary syphilis – 2-5 years, internal organs and systems, blood are affected, a rash appears on the mucous membranes, the disease either actively manifests itself or subsides.
- Tertiary syphilis - can last for decades, manifested by severe and irreversible disturbances of the nervous system and internal organs and the appearance of tubercles (gummas) on the skin and mucous membranes.
Tertiary syphilis is rare in our time, since in order for the disease to develop into this form, it must either be treated very poorly or not treated at all. This stage leads to disability and death.
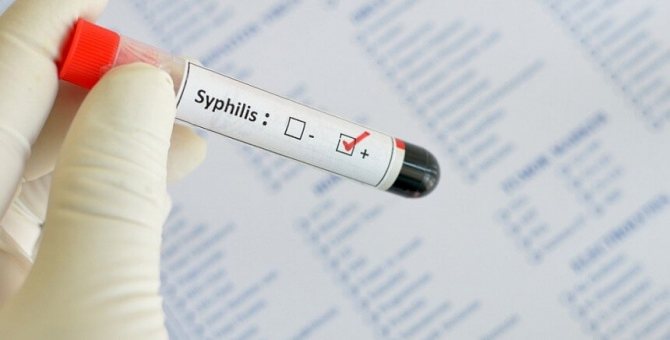
Important! There is also a latent form of syphilis, when the disease does not manifest itself with symptoms and is detected only through tests. Therefore, after questionable sexual intercourse, it is recommended to undergo a medical examination, even if the patient is not worried about anything.
When is a test for syphilis prescribed?
A test for syphilis can be prescribed for three purposes:
- To prevent the spread of the disease among the population.
- If the patient suspects the possibility of infection.
- If you have symptoms of syphilis.
For the purpose of prevention, a blood test for syphilis is prescribed:
- people who want to be donors;
- when applying for a job in children's and medical institutions;
- when a patient is admitted to a hospital or before surgery;
- when planning to conceive or during pregnancy.
The patient himself may suspect the possibility of contracting syphilis after sexual intercourse with a dubious partner or a person with syphilis. In this case, he is concerned about the question “how long before he should be tested for syphilis?” Modern methods make it possible to detect treponema approximately 3-4 weeks after infection. However, for the greatest reliability of the results, it is recommended to undergo the study approximately 1.5 months after the probable infection.
A test for syphilis is indicated if the following symptoms are present:
- rashes in the area of the external genitalia, which are accompanied by pathological discharge from the genital tract;
- swollen lymph nodes;
- rashes on mucous membranes;
- aching bones;
- febrile conditions.
They should under no circumstances be ignored. Some patients do not undergo the study due to reluctance to disclose their suspicions. In this case, you can get tested for syphilis anonymously.
At-risk groups
Usually, everyone is not sent to be tested for syphilis. There is a whole list of risk groups who will need to go for diagnostics. The first to be targeted were those who had unprotected sexual contact with an unfamiliar sexual partner.
But even without this, in medicine there are several categories that will have to undergo research:
- blood and organ donors;
- pregnant women or those planning pregnancy;
- as a preparatory stage before surgery of any type;
- workers with an increased percentage probability of infection.
In the latter case, the rule applies to medical personnel whose duty is to deal with infected patients every day.
Separately, situations are considered when testing is necessary for newborns due to the fact that their mother was still infected at the time of pregnancy. The analysis will eliminate the risks of possible congenital syphilis.
But most often, decoding is required for those who have all suspicious symptoms.
Among them are:
- ulcers in the genital area;
- genital discharge;
- skin rash;
- enlarged lymph nodes;
- bone pain.
If you notice at least a few of the signs listed above, it would be advisable to seek qualified advice from a highly specialized expert.
How to get tested for syphilis?
Nowadays, there are many methods for detecting this disease. For analysis they can take:
- blood from a vein;
- blood from a finger (quite rare, usually when a rapid test for syphilis is performed);
- cerebrospinal fluid;
- discharge from chancre;
- a sample of lymph node tissue (biopsy is performed).
The research method depends on the specific case and the characteristics of the patient’s disease. Therefore, before going for a test for syphilis, you need to go for a consultation with a gynecologist, urologist or dermatovenerologist, who, based on an examination of the patient and his complaints, will select the best option.
Important : No method guarantees an absolutely reliable result, therefore, if the result is positive, a repeat test is prescribed.
For primary diagnosis, a blood test for syphilis is most often prescribed.
How to prepare for syphilis tests?
Preparation for the study involves:
- Refusal from excessively fatty foods a day before the procedure - excess fat in the body can distort the results of the analysis.
- Avoid alcohol on the eve of the study.
- Avoid smoking for at least an hour before donating blood (preferably longer).
- Stop antibiotics at least a week before the test.
Important . The study is carried out on an empty stomach. The last meal should take place no later than 7-8 hours before blood sampling.
general description
The Wassermann test (RW) is the most popular immunological test used to diagnose syphilis since its discovery in 1906.
RW belongs to the group of complement fixation reactions (FFR) and is based on the ability of the blood serum of a syphilis patient to form a complex with the corresponding antigens. Modern RSC methods used to diagnose syphilis differ significantly in their antigens from the classical Wassermann reaction, however, the term “Wassermann reaction” is traditionally retained for them. Antibodies produced by the immune system appear in the blood of an infected person. The causative agent of the disease, Treponema pallidum, contains the antigen cardiolipin, which causes the production of antibodies detected by RW. A positive Wasserman reaction indicates the presence of such antibodies in a person’s blood, and on this basis a conclusion is made about the presence of the disease.
The hemolysis reaction is an indicator of the result of the study in the RSC. The reaction involves two components: sheep red blood cells and hemolytic serum. Hemolytic serum is obtained by immunizing a rabbit with sheep red blood cells. It is inactivated for 30 minutes at a temperature of 56°C. The results of RSC are evaluated depending on the presence or absence of hemolysis in the test tubes. The presence of hemolysis is explained by the fact that if there are no syphilitic antibodies in the test serum, then the antigen-antibody reaction does not occur, and all the complement goes to the sheep erythrocyte-hemolysin reaction. And if there are specific antibodies, the complement is completely spent on the antigen-antibody reaction and hemolysis does not occur.
All ingredients for the Wasserman reaction are taken in the same volume - 0.5 or 0.25 ml. For strong fixation of complement on a specific complex, a mixture of the test serum, antigen and complement is placed in a thermostat at a temperature of 37° for 45-60 minutes. (phase I reaction), after which a hemolytic system consisting of sheep erythrocytes and hemolytic serum is added (phase II reaction). Next, the tubes are again placed in a thermostat for 30-60 minutes until hemolysis occurs in the control, in which the antigen is replaced with physiological solution, and instead of the test serum, physiological solution is added. Antigens for the Wasserman reaction are produced in finished form, indicating the titer and dilution method.
The maximum positivity of the Wasserman reaction is usually indicated by the number of crosses: ++++ (strongly positive reaction) - indicates a complete delay in hemolysis; +++ (positive reaction) - corresponds to a significant delay in hemolysis, ++ (weakly positive reaction) - evidence of a partial delay in hemolysis, + (doubtful reaction) - corresponds to a slight delay in hemolysis. Negative RW is characterized by complete hemolysis in all test tubes.
However, sometimes false positive results are possible - this is due to the fact that cardiolipin is also found in some quantities in the cells of the human body. The human immune system does not create antibodies against its “own” cardiolipin, but there are exceptions to this rule, due to which a positive Wasserman reaction occurs in a completely healthy person. This is especially often observed after severe viral and other diseases - pneumonia, malaria, liver and blood diseases, during pregnancy, i.e. in moments of severe weakening of the immune system.
If a doctor suspects a patient has a false positive result for the Wasserman reaction, he can prescribe a number of additional tests that are usually used in diagnosing sexually transmitted diseases.
Diseases and cases in which a doctor may prescribe a blood test for RW
- Syphilis.
- Suspicion of syphilis in people who are in contact with patients with syphilis.
- Pregnancy.
- Drug addiction.
- Abortion.
- Fever accompanied by enlargement of regional lymph nodes.
- Initial visit to the clinic.
- Admission to hospital for treatment.
- Treatment in a psychiatric or neurological hospital.
- Donation of blood, tissue, sperm, and other body secretions.
- Work in the service sector, trade, medical care, social and educational sectors.
Carrying out the procedure for taking a blood test for RW
Blood for RW is donated only on an empty stomach. The last meal should be no later than 6 hours before the test. The medical worker sits the patient down or places him on the couch and takes 8-10 ml of blood from the cubital vein.
If an analysis needs to be done on an infant, the sample is taken from the cranial or jugular vein.
Preparing for a blood test for RW
You should stop drinking alcohol 1-2 days before the test. It is also not recommended to eat fatty foods - they can distort the result. During the period of preparation for the analysis, you should refrain from taking digitalis medications.
Contraindications
The analysis result will be false if:
- the patient has an elevated body temperature,
- the person is sick with an infectious disease or has just recovered from it,
- a woman is menstruating,
- pregnant in the last weeks before giving birth,
- the first 10 days after birth,
- the first 10 days of a baby's life.
Types of tests for syphilis
Methods for diagnosing syphilis are:
- Direct - aimed directly at identifying the pathogen in the test material (PCR, microscopy, cultural methods, infection of rabbits with the resulting biomaterial), usually carried out if the patient has hard chancre or rash.
- Indirect (serological) - involves the detection of antibodies to the causative agent of syphilis in the blood serum (Wassermann reaction, enzyme-linked immunosorbent assay - ELISA).
Research is also divided into
- Treponemal - detect antibodies in the blood serum to the pathogens themselves.
- Non-treponema - allow you to detect antibodies not to the treponema itself, but to the tissues of the body affected by it.
Analyzes are:
- Qualitative – indicate the presence of treponema in the body.
- Quantitative - allows you to identify the number of bacteria.

Two different tests for syphilis (nontreponemal and treponemal) are usually performed to make the diagnosis. If the first test shows a positive or questionable reaction, its results are clarified using another study.
The most common combinations are the following tests:
- Cardiolipin test (CAT) – is used for the primary diagnosis of syphilis and assessment of the results of treatment; it has replaced the Wasserman reaction, which is now considered somewhat outdated, but was previously actively used;
- ELISA (enzyme-linked immunosorbent assay) - used to confirm the diagnosis or to detect syphilis in the early stages.
Reference . Another common test for syphilis is RPHA (passive hemagglutination reaction). This highly accurate study can be performed to diagnose the disease at any stage. The analysis relates to treponemal, that is, it is aimed at detecting the pathogen itself.
Decoding the analysis results
With primary syphilis, the Wasserman reaction becomes positive at 6-8 weeks of the disease (in 90% of cases), and the following dynamics are noted:
- in the first 15-17 days after infection, the reaction in most patients is usually negative;
- at the 5-6th week of the disease, in approximately 1/4 of the patients the reaction becomes positive;
- at the 7-8th week of the disease, RW becomes positive in the majority.
In secondary syphilis, RW is always positive. Together with other serological reactions (RPGA, ELISA, RIF), it allows not only to detect the presence of the pathogen, but also to find out the approximate duration of infection.
With the development of a syphilitic infection in the 4th week of the disease, after the onset of primary syphiloma, the Wasserman reaction passes from negative to positive, remaining so both in the secondary fresh and in the secondary recurrent period of syphilis. In the latent secondary period and without treatment, RW can turn negative so that when a clinical relapse of syphilis occurs, it becomes positive again. Therefore, in the latent period of syphilis, a negative Wasserman reaction does not indicate its absence or cure, but only serves as a favorable prognostic symptom.
With active lesions of the tertiary period of syphilis, positive RW occurs in approximately 3/4 of cases of the disease. When the active manifestations of the tertiary period of syphilis disappear, it often turns negative. In this case, a negative Wasserman reaction in patients does not indicate that they do not have a syphilitic infection.
In early congenital syphilis, RW is positive in almost all cases and is a valuable method for verifying the disease. In late congenital syphilis, its results correspond to those obtained in the tertiary period of acquired syphilis.
The study of the Wasserman reaction in the blood of patients with syphilis undergoing treatment is of great practical importance. In some patients, despite vigorous anti-syphilitic therapy, the Wasserman reaction does not turn negative - this is the so-called seroresistant syphilis. In this case, it makes no sense to carry out endless antisyphilitic therapy, achieving the transition of positive RW to negative.
From the above it follows that a negative Wasserman reaction is not always a sign of the absence of a syphilitic infection in the body.
A positive Wasserman reaction is possible in people with a number of other diseases and conditions not related to syphilis: tuberculosis, systemic lupus erythematosus, blood diseases (leukemia), leprosy, pemphigus, leptospirosis, malignant neoplasms, typhus, scarlet fever, beriberi disease, sleeping sickness , during pregnancy, before or after childbirth, menstruation, after anesthesia, after drinking alcohol, in drug abusers, taking fatty foods, taking medications, introducing foreign serums. In such cases, other methods (RPGA, ELISA, RIF) are used to clarify the diagnosis. The nonspecific positive Wasserman reaction in malaria is very characteristic, especially during the attack period. Therefore, if RW is positive in a person without clinical manifestations of syphilis and who denies syphilitic infection, malaria should be considered.
All of the above indicates that a positive result of the Wasserman reaction is not yet unconditional evidence of the presence of a syphilitic infection.
Recovery after testing
After taking a blood test, doctors recommend a proper and balanced diet, as well as plenty of fluids. You can afford warm tea and chocolate. It will be useful to refrain from physical activity and under no circumstances drink alcohol.
ELISA test for syphilis
ELISA (enzyme-linked immunosorbent assay) is one of the most accurate tests for syphilis. Allows you to detect syphilis in the blood within 3 weeks after infection. This is a treponemal type of study.
The sensitivity of the test is about 90%. It allows not only to diagnose syphilis, but also to determine whether the patient has ever had this disease. This is a quantitative analysis, that is, with its help you can not only identify treponema, but also its quantitative content in the body.
During the study, blood serum is combined with markers. Serum antibodies form compounds with markers, the nature of which can determine the presence or absence of syphilis.
False results
Regardless of how much testing is done and what particular format of laboratory diagnostics was chosen, there is always a risk of error. In medical practice, it accounts for about 5% of the total number of diagnosed cases.

Usually, victims with an incorrect verdict receive a false positive result. Various diffuse connective tissue diseases can affect poor performance. Even classic rheumatoid arthritis can affect the reliability of your own information. The same applies to systemic lupus erythematosus.
But most often, a more trivial reason such as diabetes or the patient’s recent vaccination becomes an obstacle. An identical picture can be seen if the patient has a number of severe infectious diseases such as mononucleosis or tuberculosis. Viral hepatitis or heart muscle diseases can also reduce the quality of the information provided. This is especially true for endocarditis.
People who suffer from alcoholism in the most advanced stages, or who take drugs, regardless of their specific type, are also at risk of getting an unreal result.
Situations where false negative values appear are much less common. The reason for such confusion will be only one aspect - too early diagnosis. Occasionally, the same clinical picture can be seen in those who are in the late stages of syphilis. This affects the infection at a phase when antibody production has almost completely stalled.
Interpretation of a blood test for syphilis
The results of the study, depending on the chosen method, can be presented in different forms (pros and cons, numbers, etc.). But in general, the breakdown of the test for syphilis, regardless of the type of procedure, is as follows:
- The result is negative - no treponemes are observed in the blood.
- The result is weakly positive (doubtful) - a certain amount of the pathogen is present in the blood, but an accurate diagnosis cannot be made.
- The result is positive - syphilis develops in the body.
In some cases, the result may be a false negative or a false positive.
Reasons for a false negative test for syphilis

A false negative test for syphilis may occur if it was performed too early and treponemes are not yet detected in the blood serum. That is why, if we are not talking about an ELISA test, it is better to undergo the procedure 1.5 months after the alleged infection. If the patient has had questionable sexual contact and the test result is negative, a repeat test is recommended after some time.
Also, a false positive result occurs when the analysis is carried out incorrectly. Or when using express methods for detecting syphilis.
False positive test for syphilis
False-positive tests for syphilis can be in the following cases:
- during menstruation;
- with a recent myocardial infarction;
- for autoimmune diseases;
- for infections (chickenpox, hepatitis, HIV, influenza, acute respiratory infections);
- for liver pathologies;
- for oncological diseases;
- for tuberculosis;
- for pathologies;
- during pregnancy.
Sometimes an incorrect result is obtained after a recent vaccination. That is why, having received a positive test for syphilis, you should not get upset ahead of time, but should undergo additional research.
Blood test
Depending on the specific stage of development the pathology is at, subsequent therapy will differ. But to establish the stage, it is impossible to do without an appropriate clinical trial.
The name of each phase will indicate the severity of the disease. Thus, primary syphilis indicates the formation of a specific ulcer. In professional terminology, it is called chancroid. At the same time, the victim’s lymph nodes become inflamed.

If you donate blood from a vein at the initial stage of the lesion, you will be able to achieve the highest productivity of the subsequent therapy program. But if you ignore the primary alarming symptoms, you can only reach secondary syphilis.
It is characterized by the appearance of a special skin rash. The victim also becomes extremely contagious, posing a significant threat to others. Since the internal reserve of strength goes to fight the infection, the immune system gradually weakens. This suggests that catching hepatitis or any other disease of this kind is becoming much easier.
The latent course, when there are no typical signs of damage, is considered separately. Only a specific laboratory test can detect them. But being asymptomatic does not mean that the victim has ceased to be infectious. Particularly dangerous is the possibility of transmitting the infection from mother to fetus.
The final stage, called tertiary, includes severe skin lesions, destruction of the brain, bones and internal organs. This happens to approximately a third of all those infected, most of whom simply waited until the last minute or were not treated properly.
The basis for modern tactics of examining a prospective patient is not only a survey and examination, as it was a hundred years ago. Now the main tool in establishing an accurate diagnosis is a specific test, which requires the victim’s blood.
We are talking about testing for antibodies of the IgG and IgM classes. The first option indicates possible identified antibodies to the pathogen. It is not for nothing that among doctors it is briefly called simply the “treponemal test.”
The second version involves studying nonspecific antibodies. Here the basis is based on the detection of components that are released from cells destroyed by the causative agent of the disease.
This approach has several names, but they all retain the same general principle:
- nonspecific antiphospholipid test;
- nontreponemal anticardiolipin test;
- reagin test.
All of the above is based on the foundation laid in the RW algorithm, which means the Wasserman reaction.
Both clinical solutions are used not only for diagnosing pathology. They are used during potent therapy to assess the ongoing dynamics of recovery, and after treatment.
The only difference between the two procedures is the results of the examination of a person who has already successfully overcome the disease. Thus, non-treponemal results at the end of a successfully completed drug course will show the absence of a reaction. A negative response is explained by the absence of biological processes associated with the destructive effects of the pathogen on healthy cells of the body.
But the treponemal analogue, even after the period of successful treatment has ended long ago, will forever be positive. It follows that a positive response does not always guarantee relapse.
In addition to the two most popular diagnostics, there are several more that are used a little less frequently for various reasons, but they are still practiced in laboratories.
This is about:
- RPGA;
- RIBT;
- immunoblotting.
If a serological approach is relevant, the strategy can be expanded even further. It usually covers ELISA. But you should learn about the features of bladder cancer and MCI from your attending physician individually.
How is the analysis carried out?
Blood for research can be taken either from a finger or from a vein. The choice of method for collecting material depends entirely on the equipment of the laboratory. Previously, the Wassermann reaction, which is based on the complement fixation reaction, was always used.
In this case, an antigen-antibody structure is formed, which is stained. This type of diagnosis is not always accurate, and there is a possibility of obtaining a false positive result.
The Wasserman reaction is increasingly being replaced by the microprecipitation reaction. In this case, upon completion of all manipulations, white flakes fall out. The method is more accurate and error is almost completely eliminated.
A full diagnosis can be made after detecting DNA sections in the provided material.
Negative result
The specificity of the test is 98%.
The sensitivity of the test depends on the stage of syphilis: for primary syphilis it is 86%, for secondary syphilis - 100%, for latent - 89%, for late - 73%.
Although a negative result indicates the absence of infection, it still does not exclude the presence of early primary syphilis or late tertiary syphilis.
After treatment, only receiving three consecutive negative RPR results after examination by specialists (neurologist, ophthalmologist, otolaryngologist) and liquorological examination according to indications allows the patient to be removed from the register.
Complexes with this research
Preparation for IVF for a man Examination to prepare a man for the IVF procedure 6,060 RUR Composition
Examination during pregnancy. 1st trimester 16,690 RUR Composition
Pregnancy planning. Diagnosis of infections 14 tests for expectant mothers 8,620 RUR Composition
IN OTHER COMPLEXES
- Entry into IVF RUB 23,020
- Preparation for partner childbirth for a man RUB 3,680
- Hospital complex 2,100 RUR
- Men's check-up No. 1 RUB 18,570
- Expanded hospital complex 7,700 RUR