Lactostasis is stagnation of milk in the breasts of a nursing woman. The mammary gland swells, a lump is palpable in it. The skin over the stagnant ducts often becomes hyperemic. This disease can develop into mastitis (a purulent inflammatory process). It is impossible to delay the treatment of this pathology. At the first sign of congestion, it is important to contact an experienced lactation consultant.
Ointments and creams
When a woman develops lactostasis during breastfeeding, she is ready to smear her breasts with anything in order to quickly get rid of this problem. Nursing mothers note the effectiveness of such products:
- Vishnevsky ointment. In case of primary lactostasis, manifested by moderate breast tenderness, spasms of the ducts or other moderate symptoms, it is permissible to use compresses with balsamic liniment according to Vishnevsky. At the same time, the woman is recommended to take a warm shower to relieve spasms of the milk ducts.
- Arnica ointment. Homeopathic ointment containing various plant extracts. This remedy relieves swelling well and reduces pain. The milk begins to flow better and relief comes quickly. Apply the product with gentle massage movements. Before the next feeding, it is not necessary to wash your breasts, but simply wipe them with a napkin.
- Dimexide. Sometimes this drug is prescribed in the form of compresses for milk stagnation. But more often they try to do without it. Dimexide quickly enters the systemic bloodstream, and after 2 minutes it is found in milk secreted even by a healthy gland to which the product was not applied. The breakdown products of dimexide negatively affect the health of the baby.
- Progestogel. Hormonal drug based on progesterone. The gel is applied to the skin of the mammary gland using a special dispenser applicator. There is no need to rub or massage your breasts. It helps reduce swelling of the breast tissue and also reduces milk production. During treatment, a transition to artificial mixtures is indicated.
- Traumeel S. A multicomponent homeopathic drug that eliminates inflammation, pain, improves blood and lymph circulation, and also heals wounds on the nipple. When using it, you do not need to give up breastfeeding. But before feeding, the mammary gland should be washed.
- Solution "Malavit". This is a natural multi-component product. The drug relieves swelling, inflammation, itching, and pain. When treating congestion in the mammary gland, Malavit is used for compresses. It is kept for 30 minutes and repeated 3-4 times throughout the day.
- Levomekol. Not all mammologists welcome the use of Levomekol, since it contains chloramphenicol. If breastfeeding is continued during therapy, this will have a bad effect on the baby’s health. If this remedy is still used, it is recommended to switch to artificial feeding or temporarily express milk.
- Heparin ointment. This remedy can relieve pain, relieve inflammation, and also resolve seals. When treating mastitis or lactostasis, the ointment is used to resolve areas of compaction, and also as a prophylactic agent that protects against the emergence of new pathological areas.
- Troxevasin. For congestive processes in the chest, it is used in complex therapy to eliminate symptoms. When using Troxevasin, the function of the milk ducts is normalized by improving the venous outflow from the breast. Troxevasin gel is applied to the mammary gland 2 times a day until acute symptoms subside.
Along with external medications, a patient with lactostasis may be prescribed oral tablets or injectable medications. If lactostasis is complicated by purulent mastitis with the formation of abscesses, Dostinex is prescribed to stop lactation. This is a tablet dosage form. The dosage for each patient is selected individually. When using Dostinex, an irreversible cessation of lactation is observed.
Oxytocin during congestive processes can also be included in therapeutic regimens. At night, the natural hormone oxytocin is released, which promotes lactogenesis. If its secretion is insufficient, replacement therapy is resorted to. Oxytocin is administered intramuscularly, 1 ml once a day. Against the background of increased lactogenesis, muscle fibers relax and milk begins to actively move through the milk ducts, which helps to relax tense breasts.
Ointments for lactostasis are widely used due to their local action and pronounced effect. The skin should be dry and clean before applying the ointment.
How to increase lactation and overcome lactostasis

Mother's milk is the most valuable food for a baby: breastfeeding improves the child's immunity. However, for many breastfeeding mothers, breast milk disappears 2-3 months after birth. How to prevent a decrease in lactation?
lactation, breastfeeding, lactostasis
Breast milk contains all the nutrients and enzymes a newborn needs. It is easily absorbed by the child’s body, increasing his immunity against diseases. Thanks to a number of hormones, mother's milk regulates the growth and development of the baby, so problems with lactation affect the child in the most negative way. There is a dangerous trend when many nursing mothers lose breast milk 2-3 months after birth. However, experts say that most young mothers can organize breastfeeding.
Only 3% of women are incapable of full lactation and they need to start supplementing their children early, the remaining 97% can feed their baby with breast milk indefinitely.
Antibiotics
If the patient has an initial stage of lactostasis, without high fever and acute pain, then antibacterial therapy is not needed. This is because pathogenic microorganisms are not involved in the process. If, through minor injuries to the nipple, a secondary infection occurs and mastitis begins, then the woman is prescribed an antibacterial agent from the group of beta-lactam antibiotics of the penicillin series.
These products have a wide spectrum of action and are allowed for use during breastfeeding, since they are quickly eliminated from the body and do not have time to harm the baby. Women are often prescribed Amoxiclav, which is available in tablets, suspension or injection solution.
Occasionally, while taking this antibacterial agent, manifestations of an allergic reaction, dyspepsia, sleep problems, increased irritability, and liver pathologies may be observed. To treat lactostasis, the drug is prescribed in a dosage of 500 mg twice a day for 5-7 days.
Antipyretic drugs for lactostasis with fever
In some cases, women are able to bring down the temperature by expressing or applying the baby to the breast. To make an accurate diagnosis (lactostasis/mastitis), it is advisable not to drink an antipyretic immediately, but to first observe the temperature dynamics after emptying the breast.
If the diagnosis is made, then the nursing mother can take paracetamol or ibuprofen. They are NSAIDs, so they can be used as symptomatic remedies at elevated temperatures against the background of stagnant processes or in the complex treatment of inflammation of the mammary gland. It is not recommended to take more than 200 mg of ibuprofen or 325 mg of paracetamol at one time.
Lactostasis: methods of combating
It is necessary to create all conditions for emptying the mammary gland. For this purpose, pumping is used - the process is long (from 30 to 60 minutes) and not always pleasant. Therefore, you should be patient.
There are two methods of breast expression:
by hand and using a breast pump.
The manual method is more effective, physiological and gentle (if done correctly).
Whereas when using a breast pump, some areas of the mammary gland are not developed, while others are unnecessarily injured. In addition, using a breast pump if you have cracked nipples is not recommended. Because the cracks become injured due to the created vacuum and begin to bleed. Therefore, their healing slows down.

Heat and compresses
In the absence of a febrile state or purulent inflammation due to milk stagnation, a woman can use the following recommendations:
- short warm showers before feeding or pumping;
- before starting feeding, briefly use local dry heat;
- After finishing feeding, use a cold compress on the chest to relieve swelling after feeding.
A woman should remember that any heating and long-term compresses stimulate blood circulation in the area of stagnation, and this increases the inflammatory process. For lactostasis, experts do not recommend compresses with products containing ethanol or its derivatives (alcohol, vodka, chlorophyllipt, camphor alcohol). Against this background, the outflow of milk becomes difficult, and an abscess develops.
If you have lactostasis, you should not stop breastfeeding, and it is also not recommended to use heating pads and various alcohol or ointment compresses/bandages.
Physiotherapeutic treatment
Physiotherapy helps improve lymphatic drainage and blood circulation. And this allows you to eliminate swelling, pain, as well as the inflammatory process. When starting physiotherapeutic treatment, it is important to exclude contraindications: acute mastitis, mastopathy, oncopathology or any suspicion of an infectious process that is accompanied by a febrile state. Any physiotherapeutic treatment should be carried out after breast examination using ultrasound for lactostasis.
Popular procedures:
- Darsonval. Areas of compacted milk ducts are dosed with pulsed current. After a full course of procedures, it is possible to completely resolve the compacted lesions. This is a good method for advanced cases of lactostasis.
- UHF. This is a targeted thermal effect on the pathological lesion, which improves lymphatic drainage and eliminates swelling. The duration of the session does not take much time, but to achieve a positive result you need to undergo 8-10 procedures.
- Magnetotherapy. This is one of the types of hardware physiotherapy used to treat conditions associated with stagnation of milk in the mammary gland. It is recommended to combine magnetic therapy with local heating and regular procedures for expressing milk. Magnetic therapy lasts 10-20 minutes.
The patient may be prescribed several sessions of electrophoresis with magnesia, dimexide, Malavit solution or other antiseptic or anti-inflammatory drugs. This accelerates their effect and improves the effect on the mammary gland.
Massage
Breast massage for lactostasis allows you to achieve the following results:
- The tone of the muscle fibers of the milk ducts is normalized. And when they are stimulated, milk is released better and the lactation process is normalized.
- It is possible to locally influence pathological foci and normalize the outflow of milk directly from these areas.
- Due to improved blood circulation and lymph outflow from the mammary gland, breast swelling is eliminated.
To achieve the best results, you must correctly perform all components of the massage, and then express milk. Everything must be done carefully and without pressure. Do not allow injury to the mammary gland or severe pain in it. Basic massage techniques for lactostasis: stroking, rubbing and kneading. In this case, movements should be as smooth as possible.
Use the fingers of both hands. Massage movements are directed from the upper chest to the nipples. Such manipulations promote the outflow of milk in the direction of the milk ducts. Then stroking is performed around the chest towards the armpits, where lymph drainage should occur. At the end of the massage, be sure to express milk and apply a warm heating pad to relax muscle fibers and improve blood circulation.
It is advisable to use massage procedures together with medicinal ointments. It is recommended to massage twice a day for a week.
A little about the problem of lactostasis
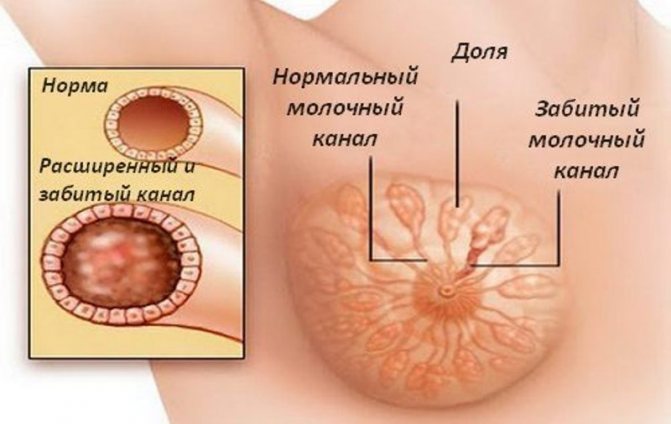
The development of lactostasis in women during breastfeeding occurs due to the cessation of the natural outflow of milk through the ducts of the gland. Doctors consider this condition physiological and do not classify it as a pathology. But in the absence of proper treatment, lactostasis provokes mastitis - an active inflammatory process in the gland.
As soon as a woman begins to feel a nagging pain in her chest and notices the appearance of lumps, she needs to consult a specialist. After 3-4 days of this state, the immune system begins to react to the accumulation of milk in the ducts and perceives it as a foreign body. The temperature rises and the infectious process starts.

Pain during breastfeeding may be symptoms of lactostasis
Traditional methods of treatment
With lactostasis, some women prefer traditional methods of treatment. Popular recipes:
- Cabbage compress. A popular home remedy. Cabbage leaf helps relieve swelling, improves milk flow, and also normalizes local blood circulation. To prepare a compress, take a cabbage leaf from the middle of the head, wash it in warm water and apply it to the mammary gland. Put a bra on top. It is advisable to leave this compress on all night.
- Honey. This tasty medicinal component is used to prepare various recipes. Honey cake is popular among women. They take semi-solid honey, form it into a cake and apply it to the chest. Cover the top with cling film and leave for 2 hours.
- Beet. To prepare a compress, take 1 medium-sized beetroot, grate it and apply the resulting mass to the mammary gland, applying it to a piece of gauze. Keep this compress for 20 minutes. Thanks to this procedure, an anti-inflammatory effect is achieved.
An interesting remedy is salted milk, which is used to relieve swelling. To prepare, take 50 ml of warm milk and add 15 g of table salt to it. After the salt has completely dissolved, gauze is moistened in the solution and applied to the mammary gland if there are no damage to the skin.
A well-fed baby means a happy mother
High-quality lactation and minimizing the risk of lactostasis largely depend on the calmness of the nursing mother. The less she worries during breastfeeding, the more milk the baby will get. This means that he will be full and healthy.
Brigham Young University has determined how many American babies are breastfed. One interesting finding is that the higher the mother's education level, the more likely her child will be to eat naturally.
Olesya Butuzova, pediatrician: “I completely agree that the main help for lactostasis is the child. You need to put your baby to your breast as often as possible. And at night, practice co-sleeping, during which the baby sucks little by little, but almost constantly. Remember also that you should not squeeze your breasts with tight bras or clothes, this can indirectly contribute to increased lactostasis.”
Expert: Olesya Butuzova, pediatrician Author: Elena Nersesyan-Brytkova
The material uses photographs belonging to shutterstock.com
Treatment regimens
Lactostasis or non-purulent forms of mastitis can be treated according to the following scheme:
- Milk must be expressed from both mammary glands up to 8 times a day (every 3-4 hours). This manipulation is performed first on the healthy and then on the diseased breast.
- To improve milk production, 0.5 ml of oxytocin is administered to the patient 5 minutes before expressing from the pathological gland. And also three times a day, 20 minutes before the pumping procedure, the woman is administered 2 ml of drotaverine.
- Every day the patient is given retromammary novocaine blockades with the addition of a broad-spectrum antibacterial agent (half the daily dose).
- Antibacterial therapy combined with intramuscular administration of antihistamines and B vitamins.
- Semi-alcohol bandages are recommended for the affected breast, and compresses with warming ointments are contraindicated.
- If noticeable improvements are observed a day after the start of conservative treatment, ultrasound or UHF can be used.
Such therapy is continued if the patient is in a stable condition and the temperature does not exceed subfebrile levels. General blood test results should be within normal limits. The pathological process should last no more than 3 days. Also, the patient should have no symptoms of purulent inflammation, and the infiltrate should occupy no more than one quadrant of the gland. If after 48 hours of enhanced conservative therapy there is no positive dynamics, then surgical intervention is indicated.
Lactostasis causes many unpleasant and painful sensations in a nursing woman, and also affects the nutrition of the child. This pathology should be treated immediately. There are many medications and folk recipes for this. Noticeable improvements will come faster if a woman consults a doctor. And she must also take into account the standard rules of feeding and caring for the mammary gland.
Causes and signs of milk stagnation
Blocked milk ducts occur for a number of reasons:
- feeding without changing positions, when the baby absorbs only one lobe of the gland, and in the rest the milk stagnates and cannot fully flow;
- constriction bra with hard underwire;
- inactive breastfeeding due to addiction to bottles and pacifiers;
- injury to the breast, as a result of which the gland swells, the milk ducts are compressed, causing lactostasis;
- excessive lactation or pumping unnecessarily - if there is more milk than needed, the baby does not have time to suck it out, which causes stagnation.
The danger of lactostasis increases if the mother puts the baby to the breast less often than once every 2-3 hours. When a blockage of the milk ducts develops, a number of signs appear in the first days. First, a compaction appears in the gland, resembling a ball. The breasts become hot to the touch, swollen and red. Further, the symptoms of lactostasis in nursing mothers intensify - nagging pain is constant, subsiding slightly after feeding, and body temperature rises.
Typically, the temperature during lactostasis does not reach levels above 37.5 ° C, but if the thermometer shows high readings for 3-4 days, doctors may suspect the development of mastitis. Therefore, it is important to promptly pay attention to the symptoms of stagnation and begin treatment.